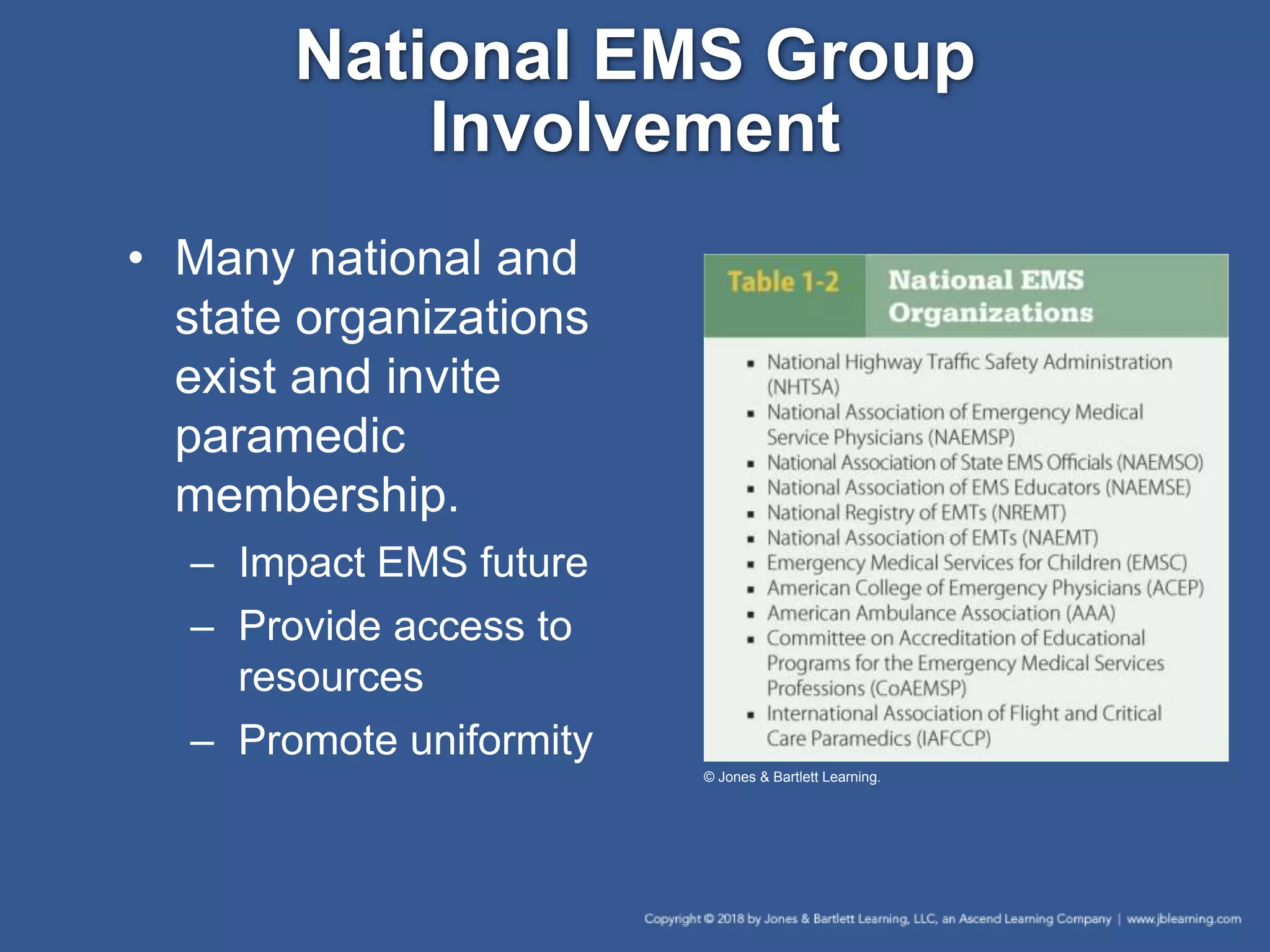
This chapter discusses the history and development of Emergency Medical Services (EMS) systems. It covers the roles of various EMS personnel like EMTs, paramedics, and medical directors. The chapter also addresses important topics like quality improvement, medical research, ethics, and evidence-based practice within EMS. Overall, the chapter provides an overview of the key aspects of EMS systems and the roles and responsibilities of EMS professionals.