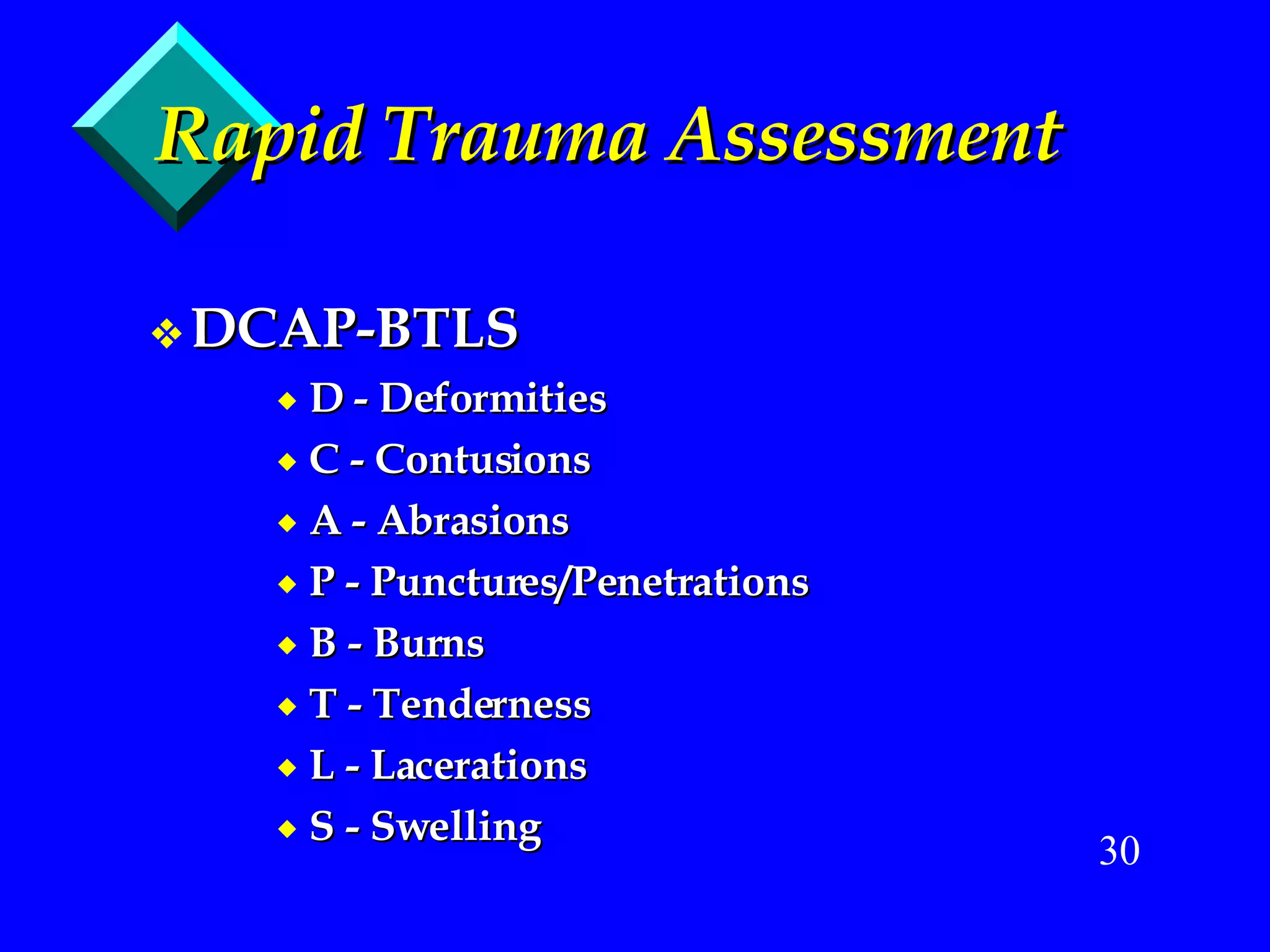
- The document provides guidance on initial assessment and management of trauma patients, emphasizing the importance of quickly identifying and correcting life threats during the primary survey.
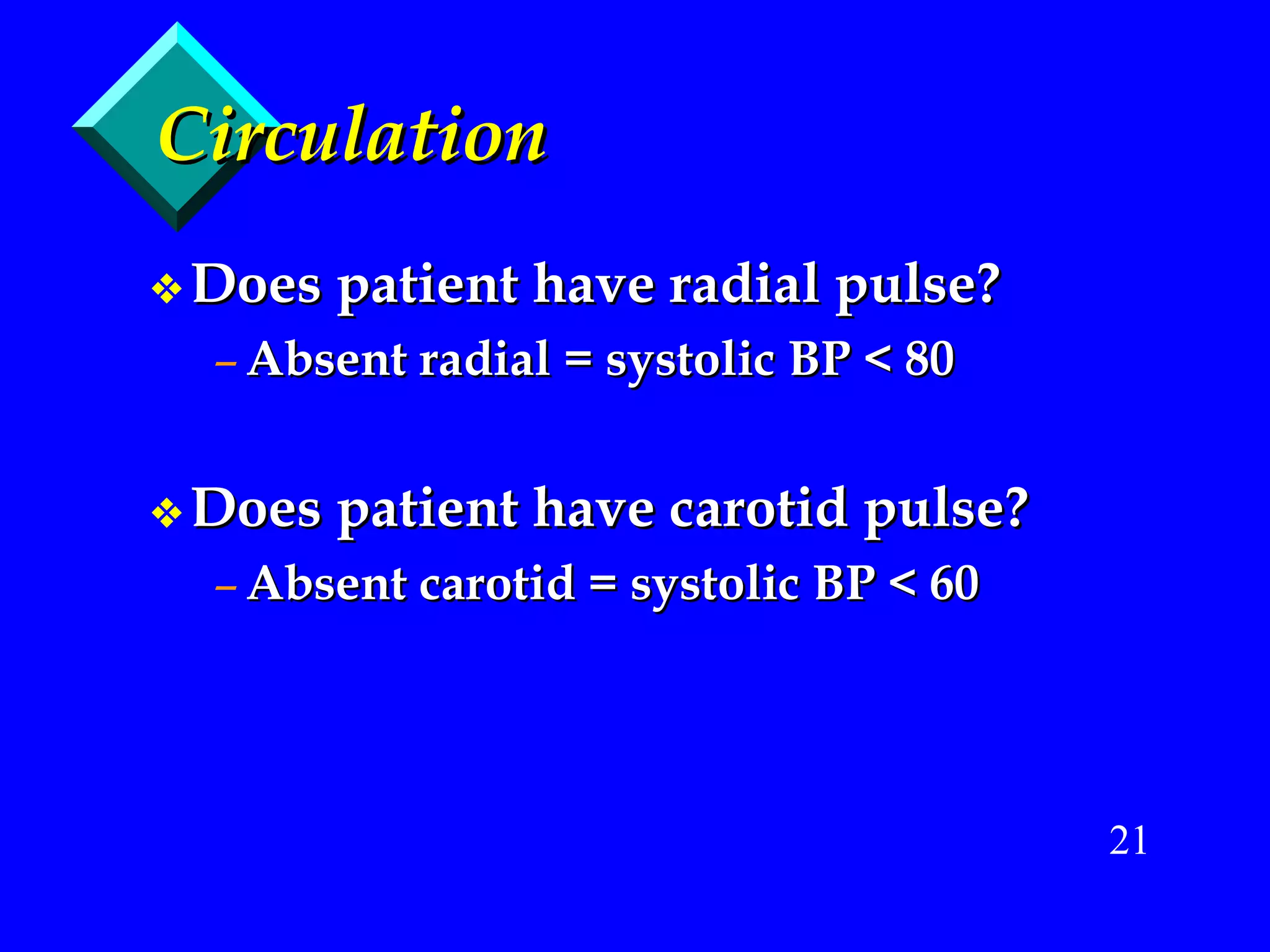
- The primary survey focuses on the ABCs - Airway, Breathing, Circulation. Oxygen should be given immediately if needed and breathing/ventilation issues addressed. Serious bleeding must be controlled.
- Only after life threats are stabilized should a more detailed exam and history be performed, and the patient transported without delay to definitive care. Rapid assessment and treatment is critical for trauma patients.