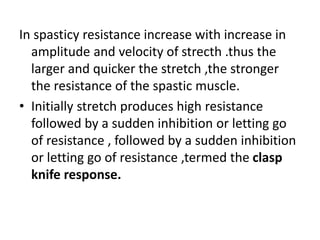
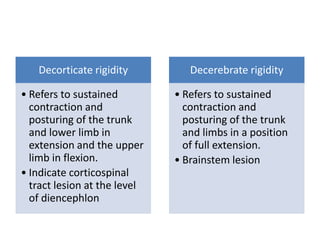
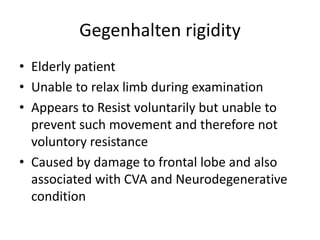
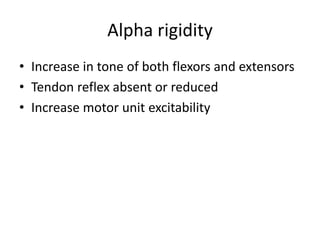
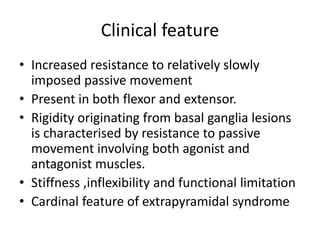
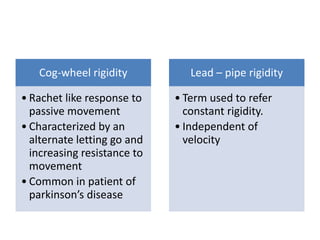
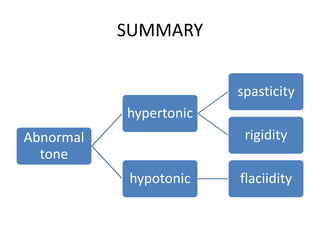
This document defines and describes different types of muscle tone abnormalities. Muscle tone is the resistance offered by muscles to passive stretch. Hypertonia includes spasticity and rigidity, where there is increased resistance to stretch. Spasticity is velocity-dependent and involves exaggerated reflexes. Rigidity is resistance throughout range of motion. Hypotonia involves decreased or absent resistance and flaccidity. Specific types of hypertonia and hypotonia are further described based on their neurological causes and clinical presentations.