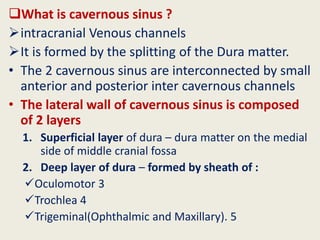
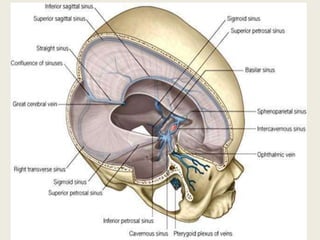
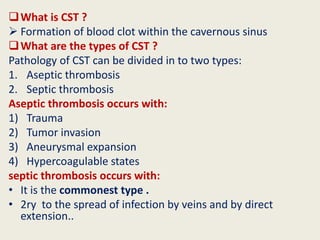
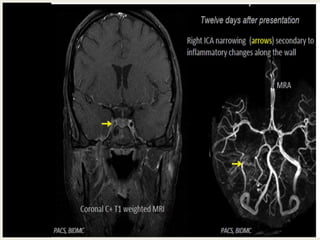
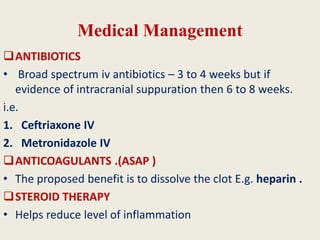
1) Cavernous sinus thrombosis is a blood clot that forms within the cavernous sinus, which is a venous channel within the skull.
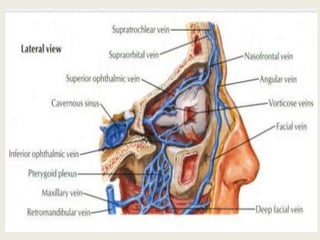
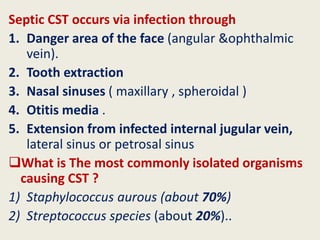
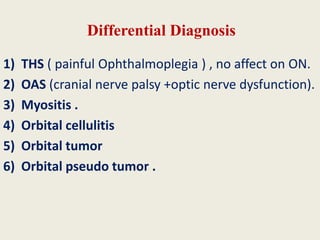
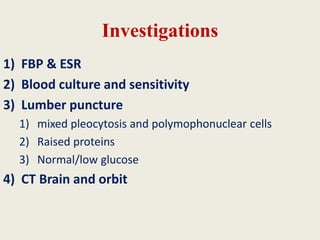
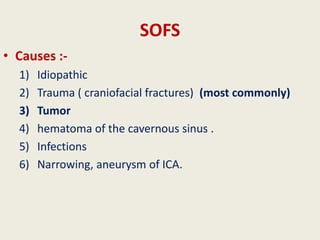
2) It can be aseptic (caused by trauma, tumors, or hypercoagulable states) or septic (caused by bacterial infection spreading from nearby areas like the face, sinuses, or ears).
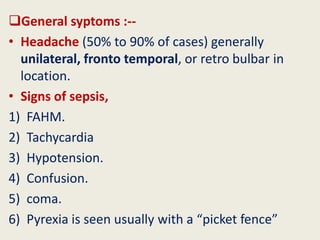
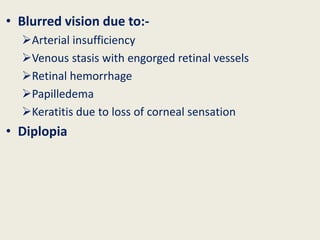
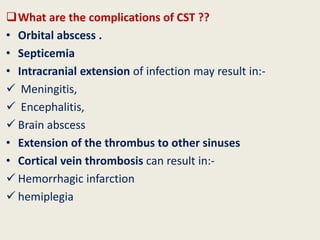
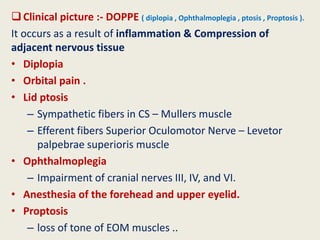
3) The most common symptoms are headaches, signs of sepsis, and ocular issues like proptosis, ophthalmoplegia, ptosis, and blurred vision. Complications can include orbital abscesses, meningitis, or extensions of the clot or infection.