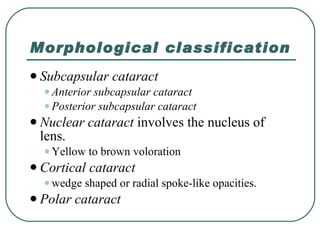
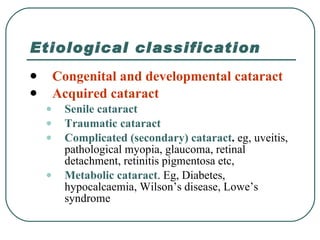
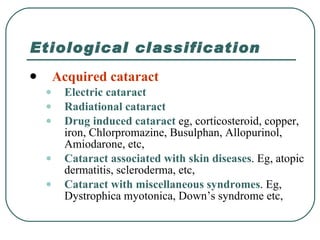
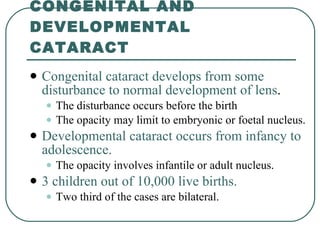
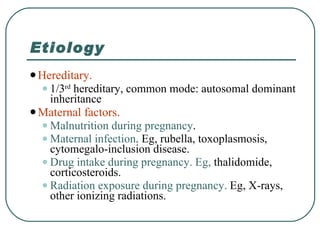
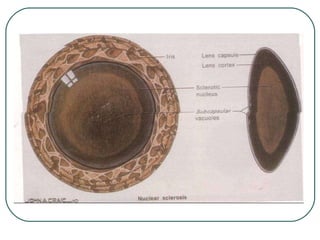
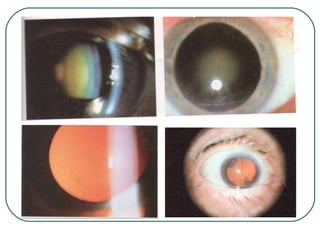
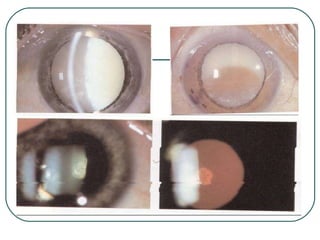
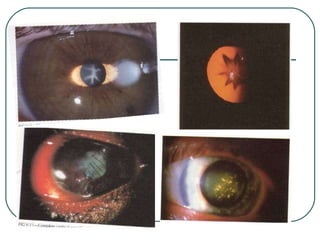
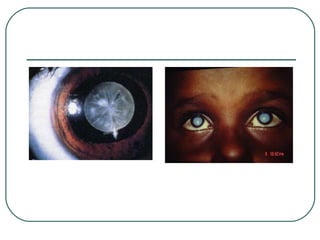
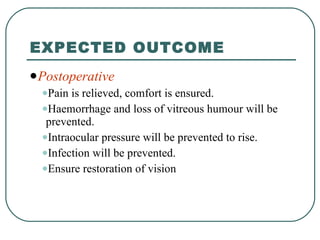
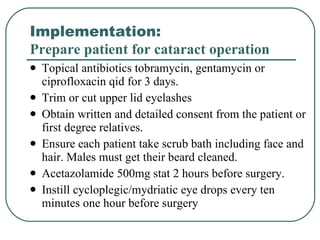
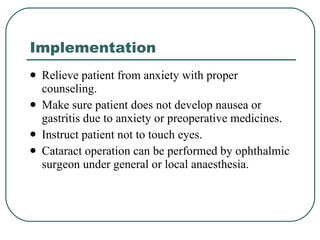
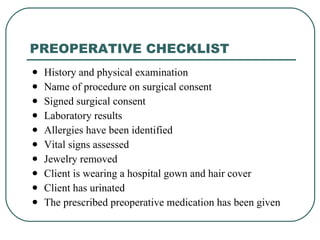
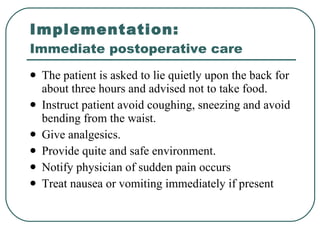
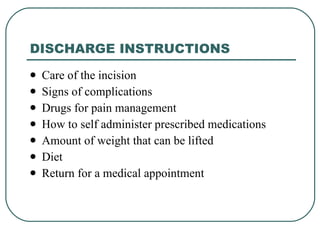
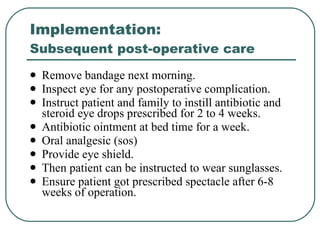
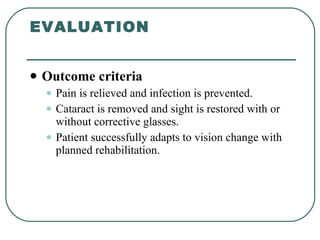
The document provides a comprehensive overview of cataracts, including definitions, classifications, etiologies, and nursing assessments related to cataracts. It describes various types of cataracts, factors influencing their development, and highlights the surgical options available for treatment, such as extracapsular cataract extraction and phacoemulsification. Additionally, it covers preoperative and postoperative care, including patient education and management of complications.