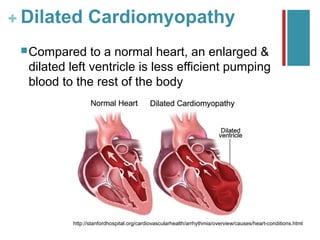
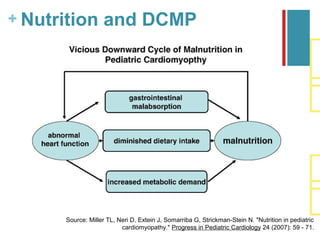
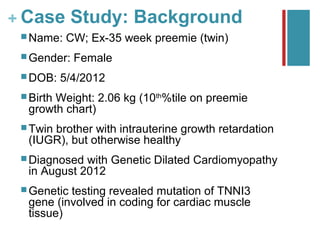
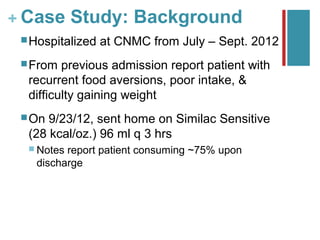
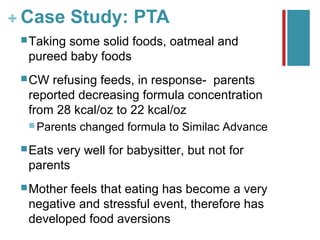
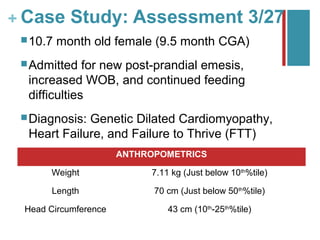
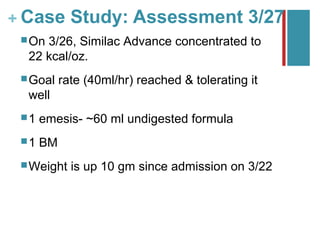
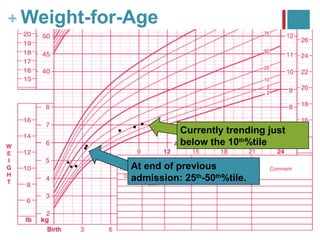
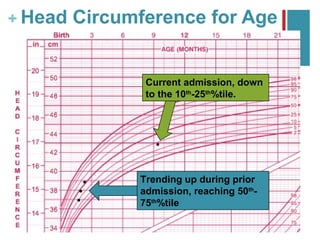
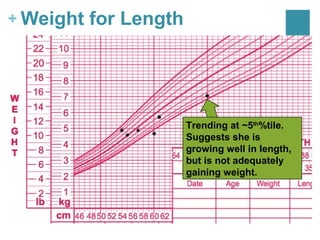
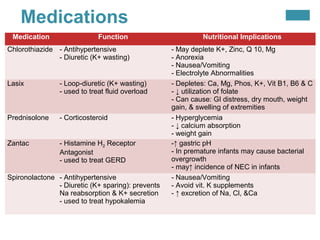
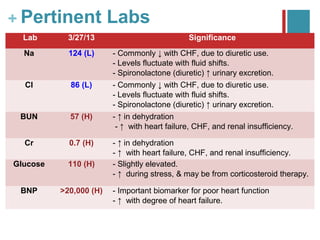
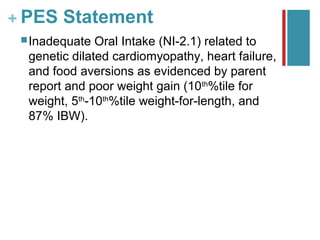
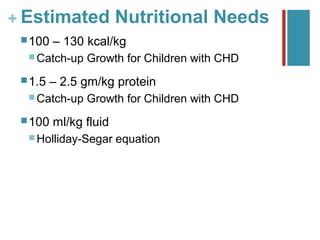
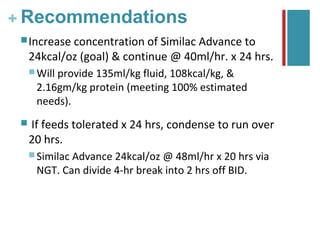
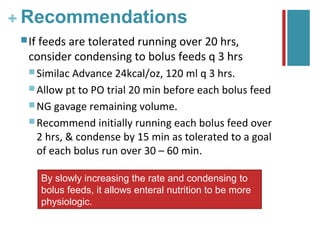
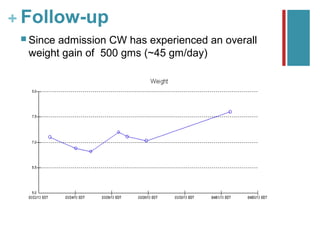
This document summarizes a case study of a 10-month-old female infant diagnosed with genetic dilated cardiomyopathy. The infant was experiencing poor weight gain, recurrent food aversions, and increased work of breathing. An assessment found the infant's weight and weight-for-length were below the 10th percentile. The patient's medications could impact nutrition by causing electrolyte abnormalities and gastrointestinal side effects. The dietitian recommended increasing the concentration of the infant's formula to meet her estimated caloric and protein needs and support catch-up growth. Follow-up found the infant had gained weight but was unstable and enteral intake needed close monitoring.