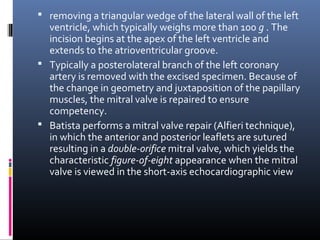
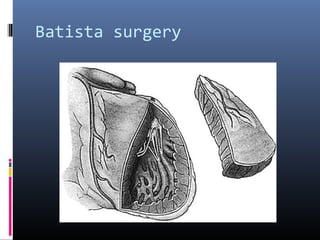
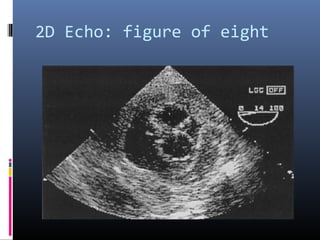
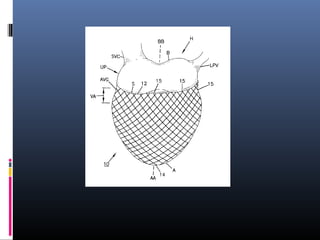
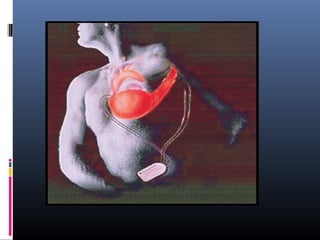
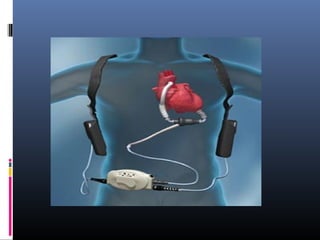
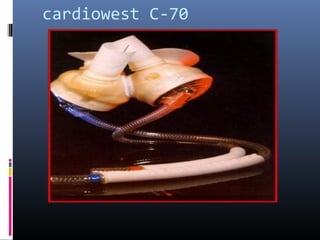
The document discusses various surgical treatments for dilated cardiomyopathy (DCM) and restrictive cardiomyopathy (RCM), whose end result is often heart failure. The main treatments discussed are the Batista operation which removes part of the left ventricle to reduce its size, ventricular restoration surgery to return the heart to a more normal elliptical shape, devices to constrain or compress the ventricles, dynamic cardiomyoplasty which uses stimulated muscle to augment heart function, ventricular assist devices to partially or fully replace pump function, and heart transplantation as a last resort. Recent advances include smaller continuous flow pumps that are easier to implant.