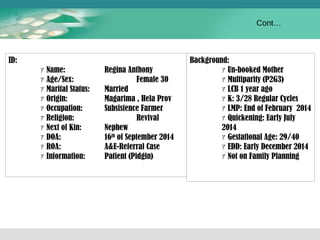
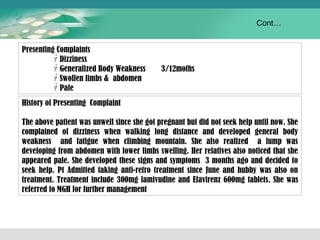
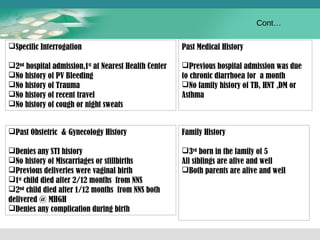
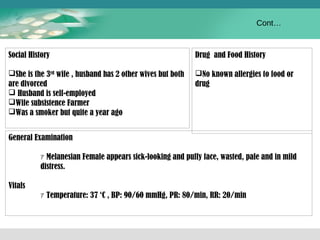
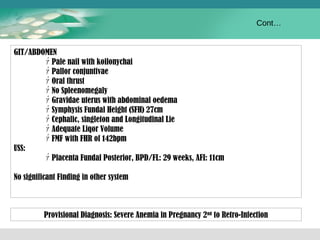
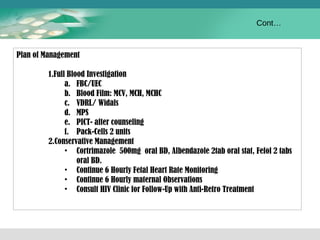
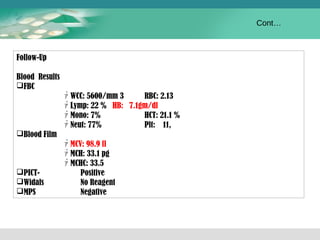
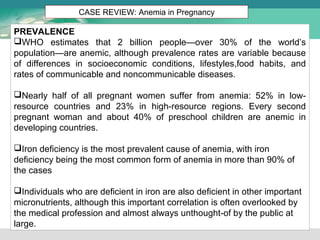
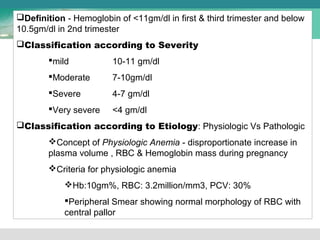
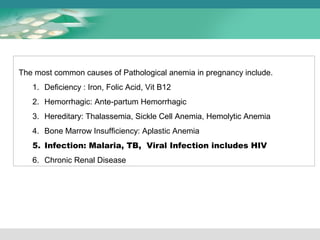
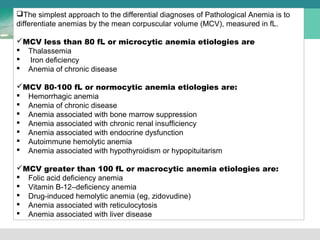
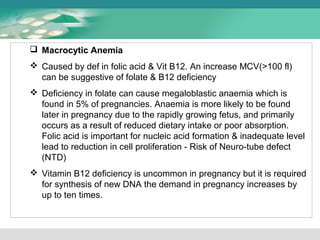
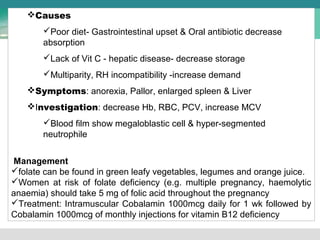
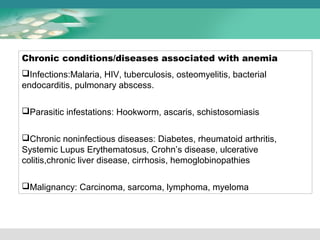
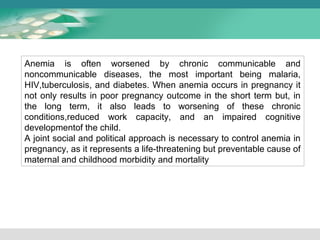
Regina Anthony, a 30-year-old pregnant woman at 27 weeks gestation, presented with dizziness, generalized body weakness, swollen limbs, and paleness for 3 months. On examination, she appeared pale and sickly. Laboratory results showed severe anemia with a hemoglobin of 7.1 g/dL. She was diagnosed with severe anemia in pregnancy secondary to HIV infection. She received blood transfusions, antiretroviral therapy, and treatment for anemia. Anemia is common in pregnancy and can be caused by iron deficiency, infection, or other nutritional deficiencies. It poses serious risks if left untreated.