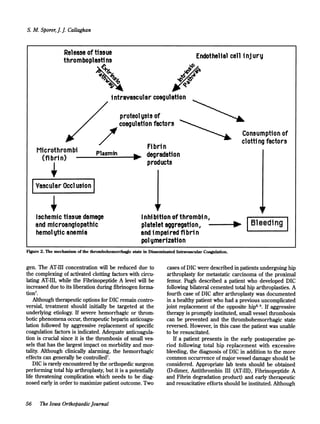
A 82-year-old woman underwent a total hip arthroplasty and developed acute disseminated intravascular coagulation postoperatively. She experienced profuse bleeding through her surgical drain and had a precipitous drop in blood pressure. Despite aggressive treatment including blood transfusions, coagulation factor replacements, and hemodynamic support, her condition deteriorated over the next two weeks with multi-organ dysfunction. She ultimately died from her disseminated intravascular coagulation 14 days after her surgery. Disseminated intravascular coagulation is a life-threatening condition with high mortality that can rarely complicate total hip arthroplasty as seen in this case.