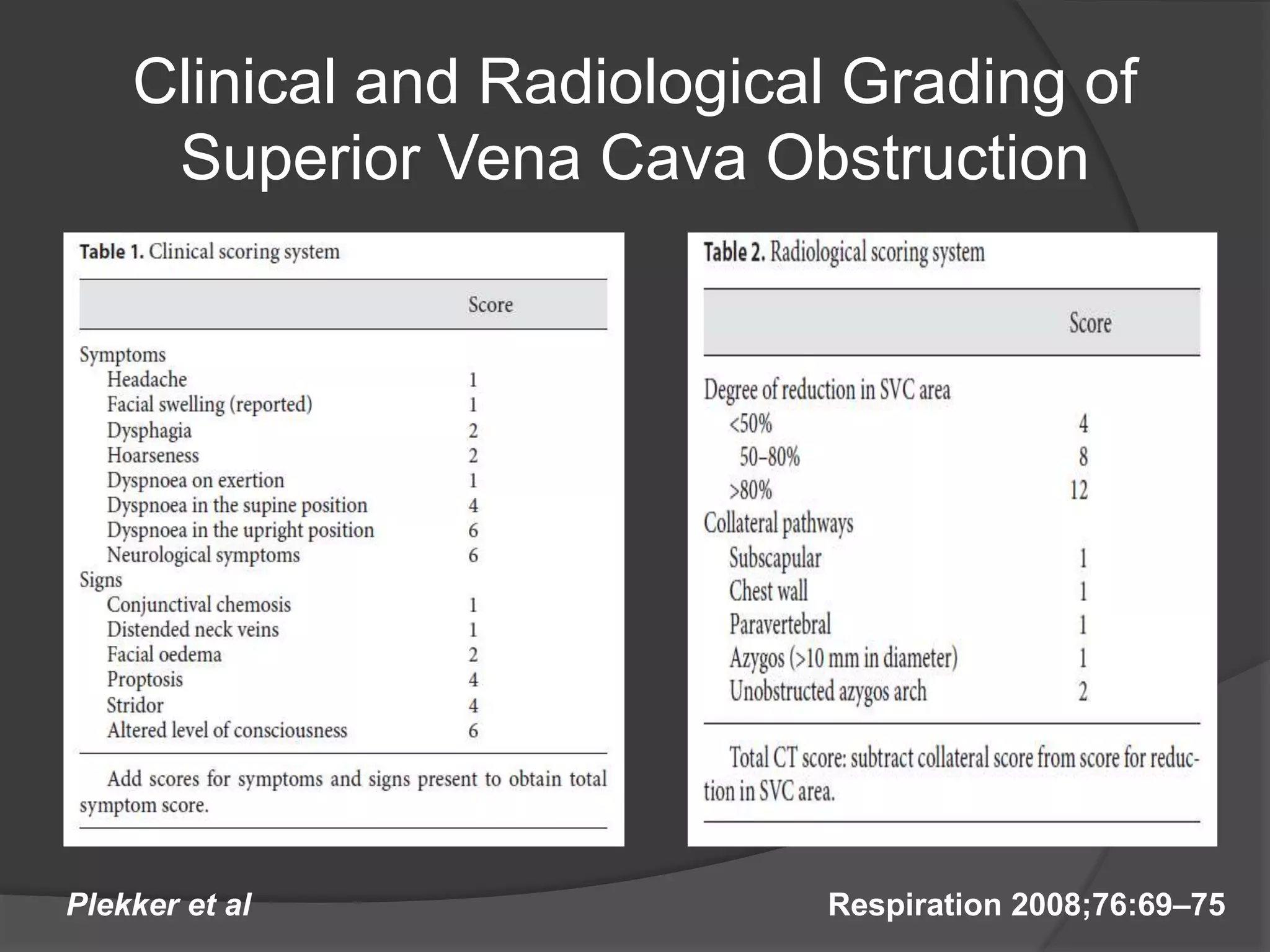
This document discusses Superior Vena Cava Syndrome (SVCS), which occurs when the Superior Vena Cava (SVC) is compressed, reducing blood flow from the head and upper body. The document covers the case presentation of a patient with SVCS, including symptoms, imaging findings, and treatment. It then provides details on the anatomy, etiologies, clinical features, imaging and classification of SVCS. Treatment options for malignant causes of SVCS such as radiation therapy, chemotherapy and stenting are described. A grading system and treatment algorithm for SVCS are also presented.