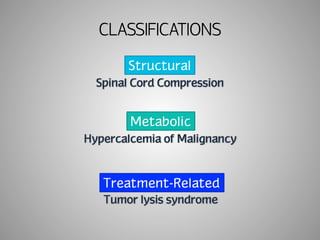
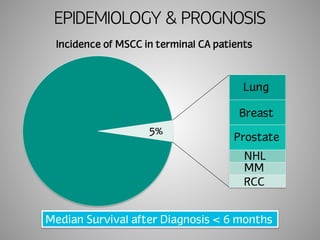
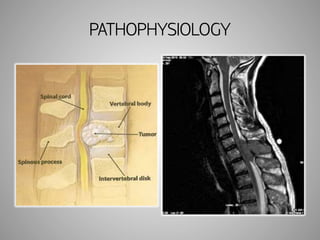
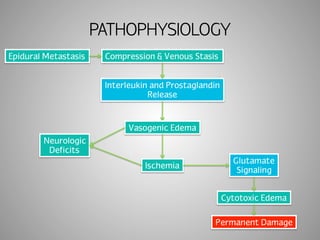
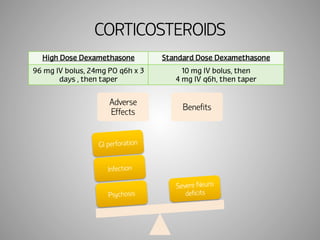
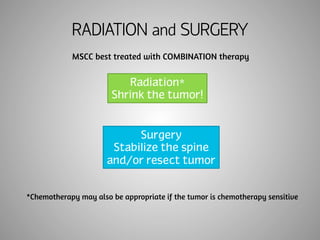
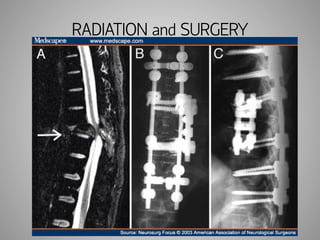
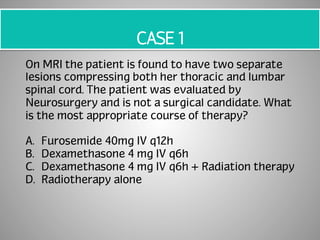
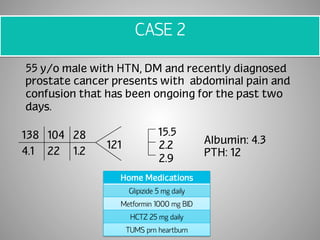
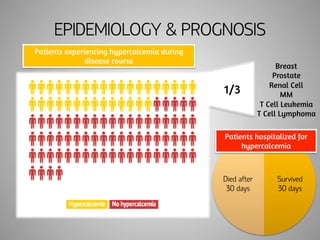
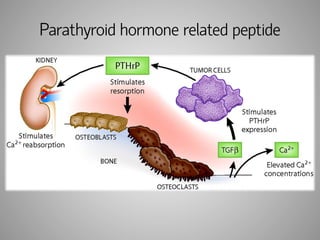
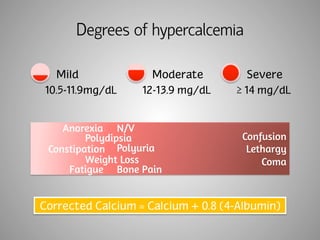
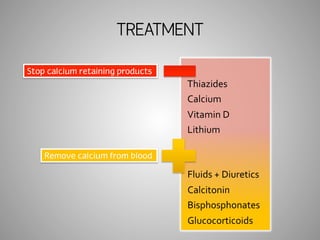
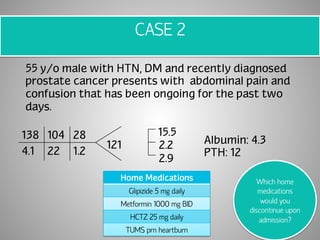
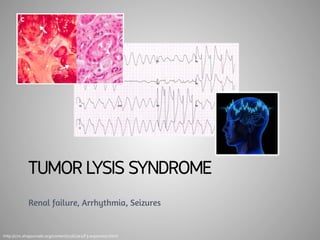
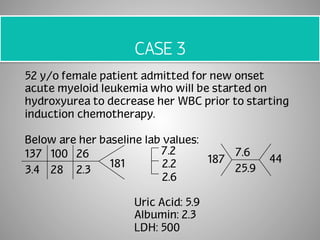
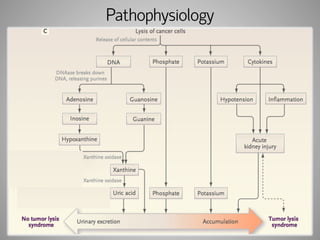
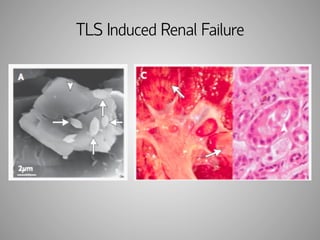
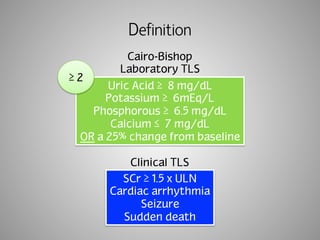
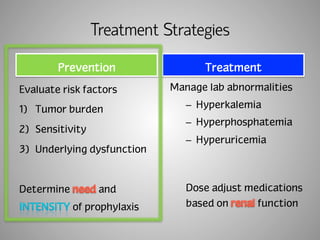
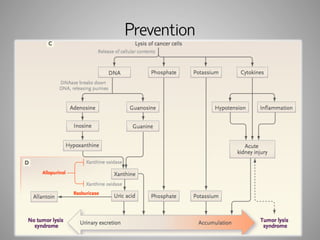
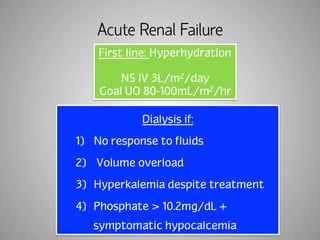
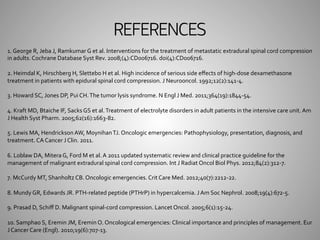
The document outlines the management and treatment strategies for several oncologic emergencies including malignant spinal cord compression (MSCC), hypercalcemia of malignancy, and tumor lysis syndrome (TLS). It emphasizes the need for early recognition and intervention, with specific treatment options such as corticosteroids, radiotherapy, and hydration protocols, alongside management of associated complications. The document also includes case studies to illustrate clinical decision-making in real-world scenarios.