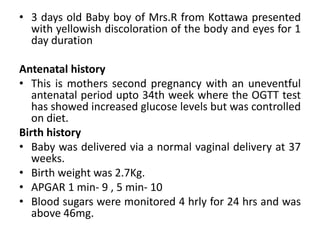
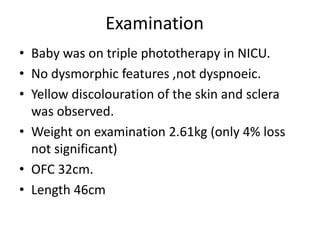
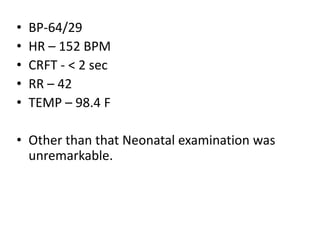
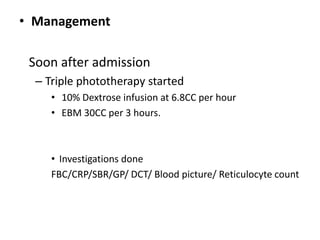
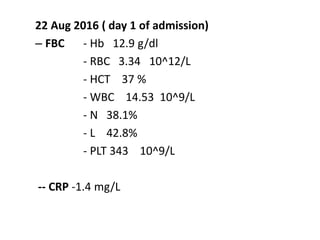
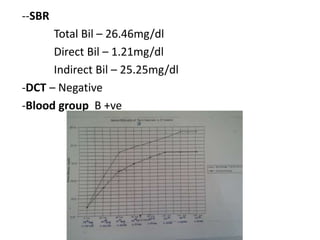
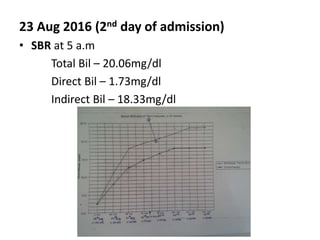
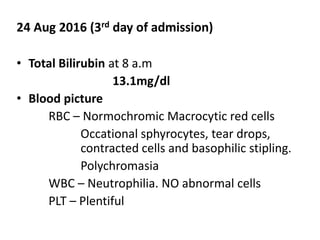
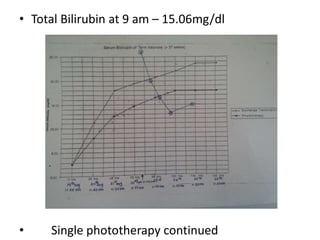
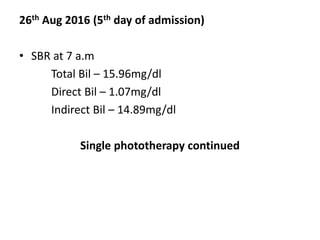
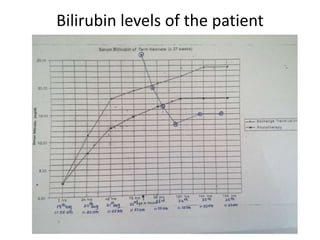
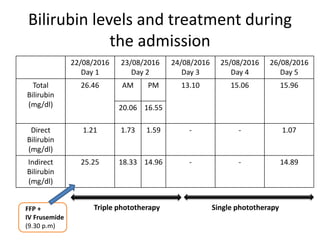
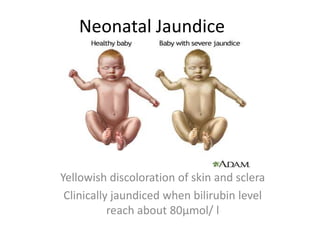
This case presentation describes a 3 day old baby boy who presented with jaundice. The baby's mother had gestational diabetes that was controlled with diet. The baby was delivered vaginally at 37 weeks with normal birth parameters. On the third day of life, the mother noticed the baby had yellow discoloration of the skin and eyes. Laboratory tests found the baby's total serum bilirubin level was above the exchange transfusion threshold. The baby was admitted and started on triple phototherapy. Over the next few days, the bilirubin level decreased with phototherapy and the baby was discharged once the level was significantly below the phototherapy threshold.
![• Usually over 50% of all new born infants become visibly
jaundiced because of,
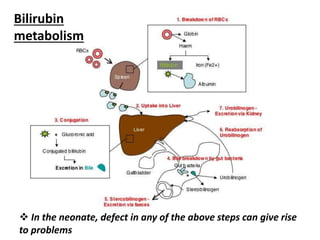
High [Hb] at birth RBC breakdown
RBC life span of infants are short(70 days)
Less efficient bilirubin metabolism
Early neonatal jaundice is important :
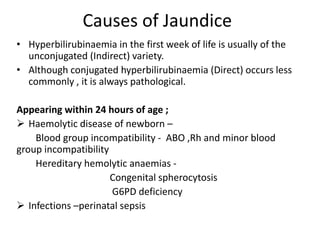
# as it may be a sign of another disorder;
Eg: Haemolytic anaemia
Infection
Metabolic disease
Liver disease
# Unconjugated bilirubin deposition in basal ganglia may
cause Kernicterus](https://image.slidesharecdn.com/casepresentationonneonataljaundicecorrected-160828084805/85/Case-presentation-on-neonatal-jaundice-corrected-27-320.jpg)