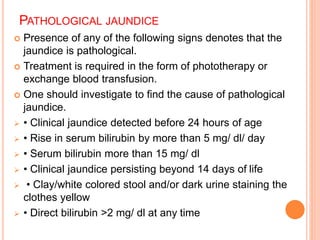
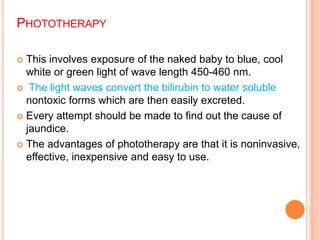
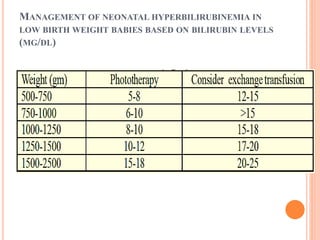
This document discusses neonatal jaundice (hyperbilirubinemia) in newborns. It begins by explaining that jaundice is caused by elevated bilirubin levels, which is a normal occurrence in many newborns due to immature liver function and the breakdown of red blood cells. The document then covers the assessment, types (physiological vs pathological), risk factors, causes, investigations and management of neonatal jaundice. Key points include that physiological jaundice is common in the first week of life but requires treatment if bilirubin levels rise too quickly or become too high. Treatment options discussed are phototherapy and exchange transfusion.