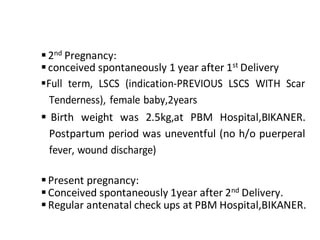
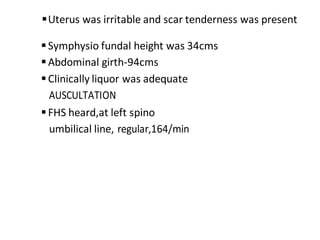
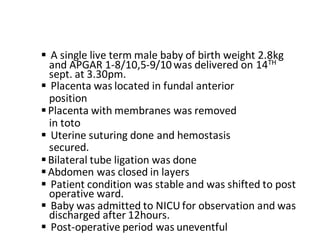
A 32-year-old woman, G3P2L2, presented with 9 months of amenorrhea and abdominal pain for 2 hours. She had a history of two previous cesarean sections. On examination, the uterus was enlarged corresponding to 32 weeks with a single fetus in cephalic presentation. An emergency cesarean section was performed under spinal anesthesia due to scar tenderness, delivering a healthy male baby. The postoperative period was uneventful.