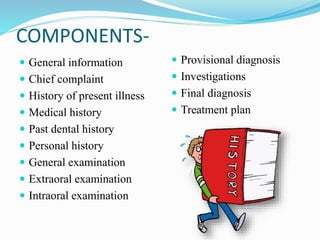
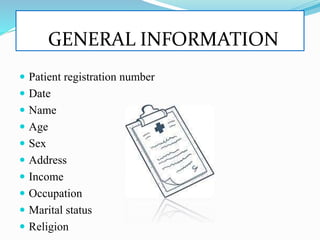
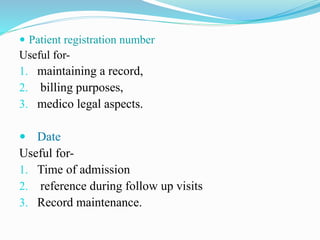
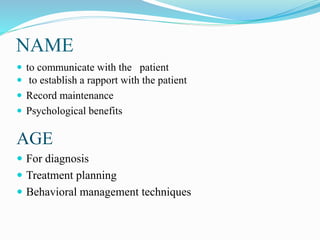
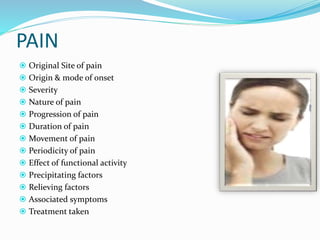
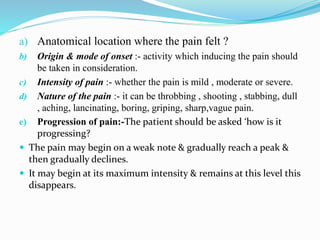
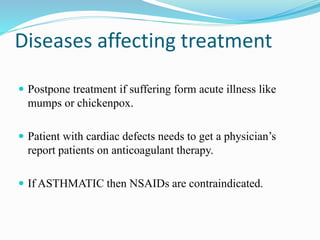
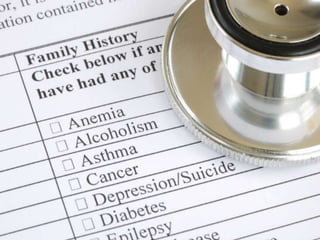
This document provides information on taking a case history for dental patients. It defines a case history and lists its objectives, which include establishing a relationship with the patient, providing information for diagnosis and treatment decisions. The components of a case history are outlined, including general information, chief complaint, medical and dental history, and examinations. Details are given on collecting information for each component, such as symptoms, medications, habits, and family history. Taking a thorough case history is important for understanding the patient's condition and developing an appropriate treatment plan.