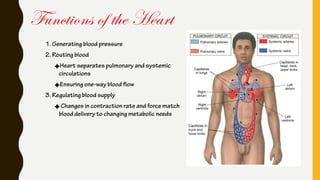
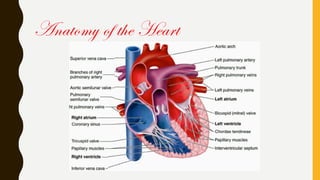
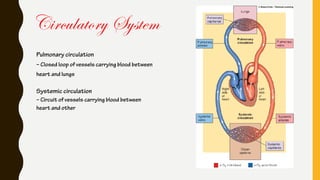
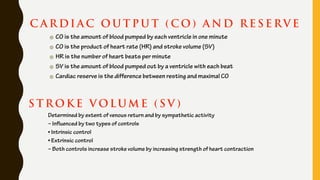
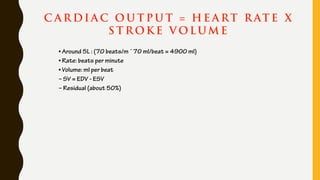
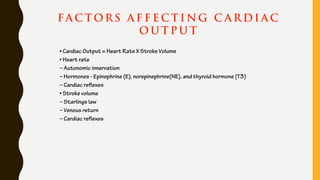
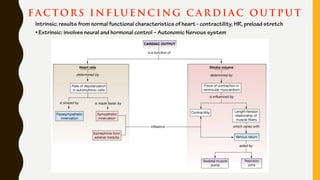
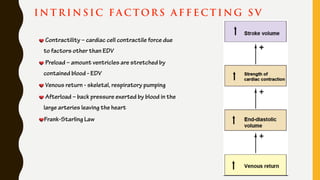
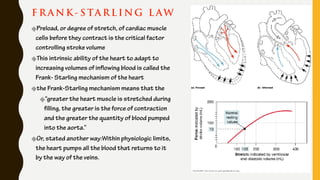
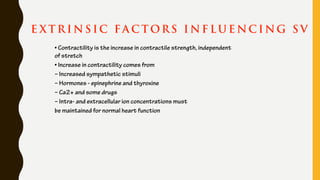
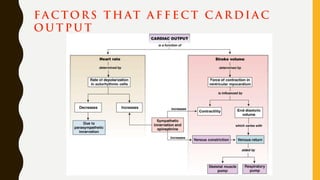
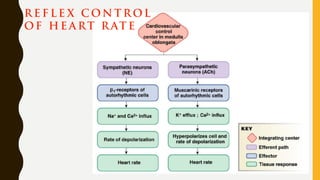
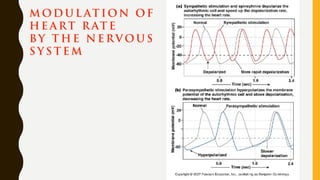
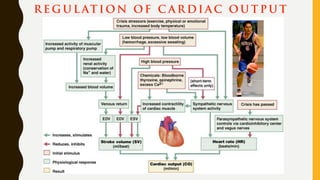
The heart functions to pump blood throughout the body via two circulatory systems - pulmonary and systemic. It generates blood pressure and ensures one-way blood flow. Cardiac output, the amount of blood pumped, is determined by heart rate and stroke volume. Intrinsic factors like the Frank-Starling mechanism and extrinsic neural and hormonal controls regulate cardiac output in response to the body's changing needs.