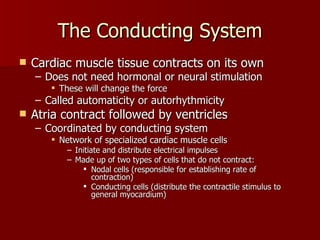
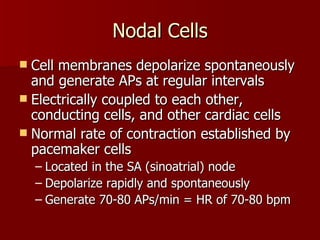
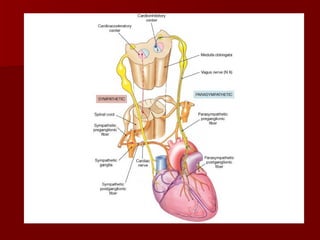
The heart has contractile cells that produce powerful contractions to propel blood flow and a conducting system to control and coordinate the activity of the contractile cells. The conducting system is made up of nodal and conducting cells that initiate and distribute electrical impulses without contracting. It establishes the heart rate and ensures coordinated contraction of the atria and ventricles. The cardiac cycle involves systole where the heart contracts and diastole where it relaxes, moving blood from high to low pressure areas. Cardiac output, the amount of blood pumped per minute, is regulated by factors like blood volume, autonomic innervation, hormones, ion concentration and temperature.