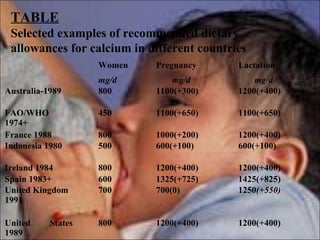
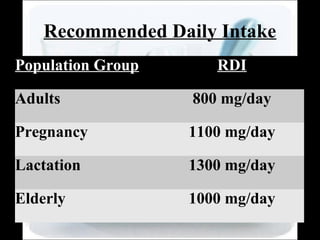
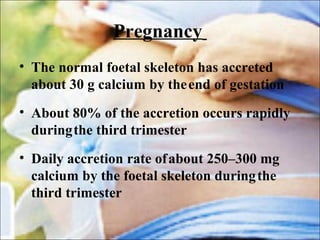
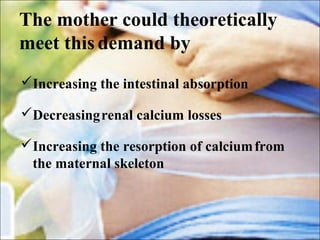
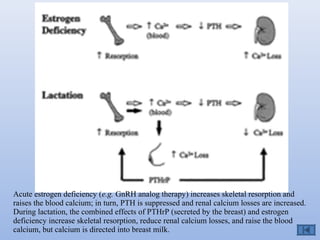
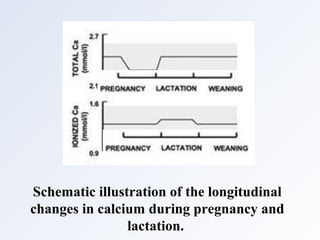
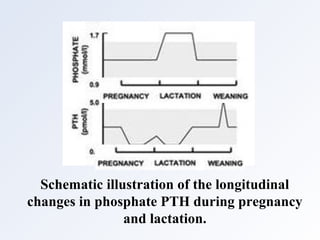
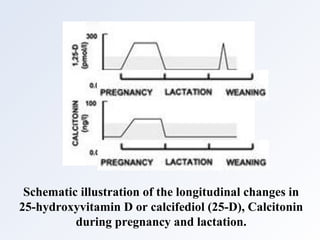
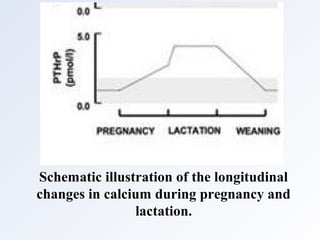
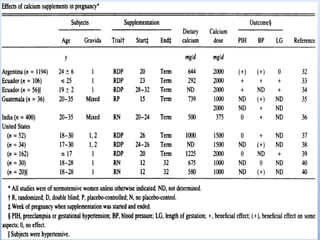
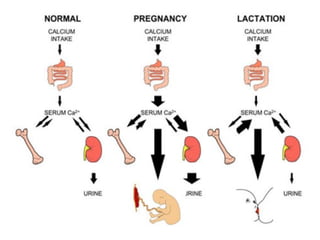
During pregnancy and lactation, calcium requirements increase substantially to support the developing fetus and breastfeeding infant. The placenta transfers 200-300mg of calcium daily to the fetus during pregnancy, while breastmilk contains 280-400mg of calcium that is secreted daily during lactation. To meet these demands, women undergo physiological adaptations like increased intestinal calcium absorption facilitated by elevated vitamin D and intestinal calbindin levels. They also experience decreased urinary calcium excretion through effects of PTHrP and estrogen. These changes, along with calcium mobilization from maternal bones, enable women to direct calcium to the fetus and breastmilk. Low calcium intake can potentially impact fetal and infant growth and development as well as maternal bone health.