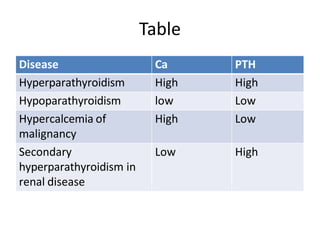
1. Disorders of the parathyroid glands involve abnormalities in the regulation of calcium and phosphate levels by parathyroid hormone (PTH). Hyperparathyroidism and hypoparathyroidism can both lead to changes in calcium levels.
2. Hyperparathyroidism is most commonly caused by a single parathyroid adenoma and results in elevated PTH and calcium levels. It can cause symptoms of bone loss, kidney stones, and abdominal pain. Hypoparathyroidism results from low PTH levels and causes low calcium levels and symptoms of muscle spasms.
3. Diagnosis involves measuring calcium and PTH levels, and imaging tests may be used to locate parathy




![Endocrine Regulation of [Ca++]ECF
http://courses.washington.edu/conj/bess/calcium/calcium.html
1. PTH stimulates the release of Ca++ from
bone, in part by stimulating bone
resorption.
2. PTH decreases urinary loss of Ca++ by
stimulating Ca++ reabsorption.
3. PTH
stimulates
intestine
indirectly
Ca++ absorption in the small
by stimulating synthesis of
1,25(OH)2D in the kidney.](https://image.slidesharecdn.com/disordersoftheparathyroidglands-141113110252-conversion-gate021-230212182058-b78894a8/85/disordersoftheparathyroidglands-141113110252-conversion-gate02-1-pdf-5-320.jpg)