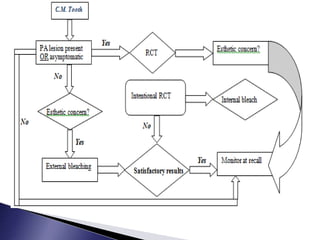
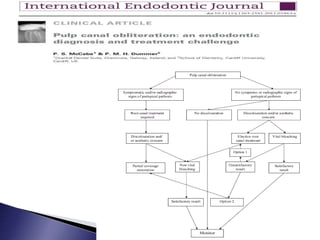
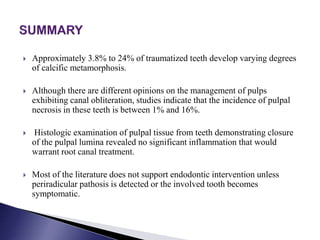
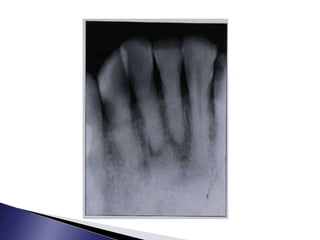
This document discusses calcific metamorphosis (CM), which is hard tissue deposition within the root canal space after traumatic dental injuries. CM is commonly seen in anterior teeth and can partially or fully obliterate the root canal space on radiographs. The document covers the definition, causes, incidence, radiographic appearance, histology, and proposed mechanisms of hard tissue formation in CM. It also discusses the controversy around treating teeth with CM, with most literature recommending observation unless symptoms appear. The document provides tips for locating and negotiating canals when CM is present, including using anatomical knowledge and correlating radiographs with tooth morphology.
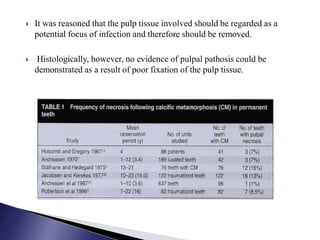

![ Jacobsen and Kerekes conducted a study of 122 traumatized teeth in which
partial canal obliteration was identified in 36% of the cases and total canal
obliteration in 64%.
Only 13% eventually developed pulpal necrosis. Smith [19] performed a
literature review and found that teeth with calcific metamorphosis have a
low incidence of periapical pathosis development (0-16%) and
recommended delaying treatment until symptoms or radiographic changes
develop.
The development of CM following trauma does not justify prophylactic
root canal therapy.](https://image.slidesharecdn.com/calcificmetamorphosis15-190508144531/85/Calcific-metamorphosis-52-320.jpg)