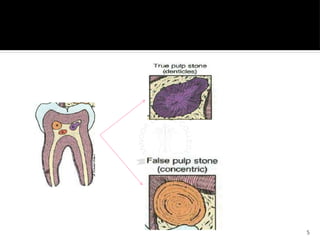
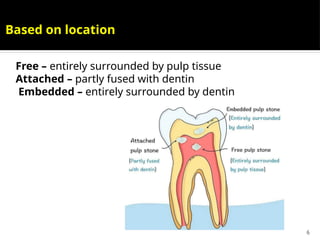
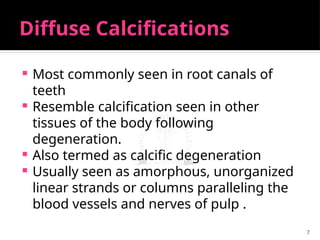
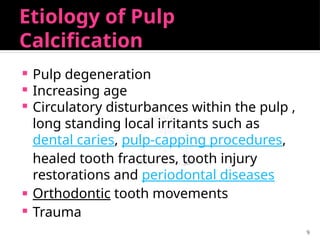
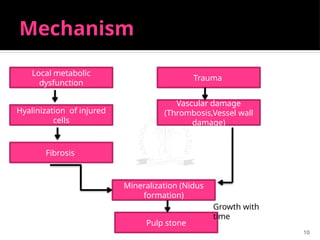
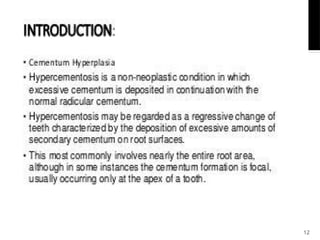
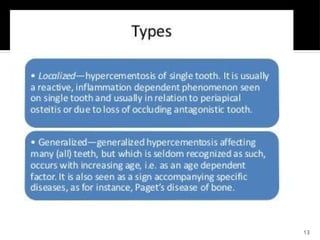
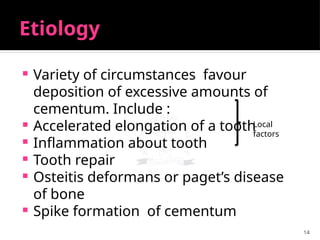
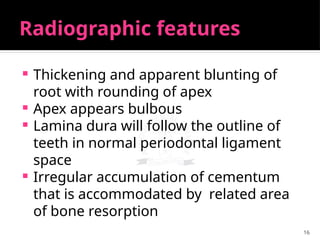
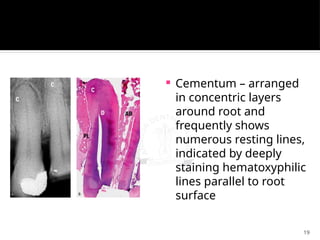
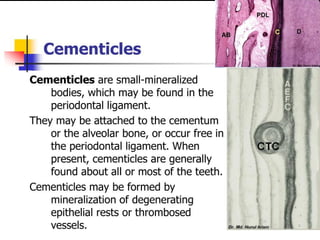
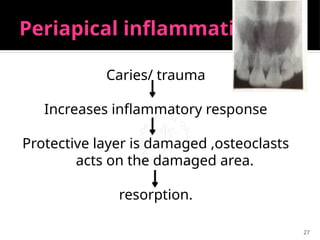
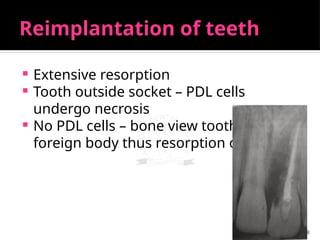
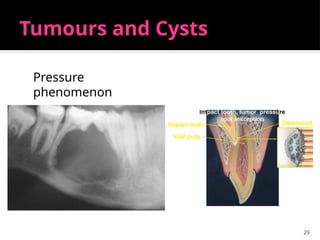
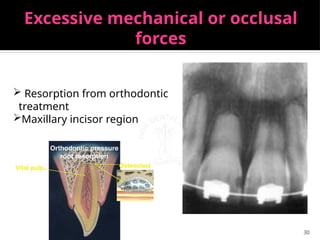
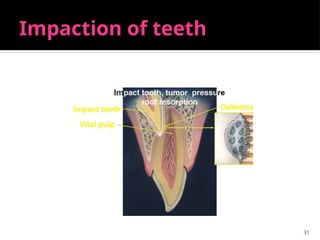
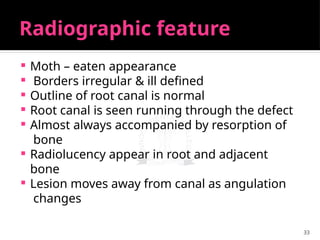
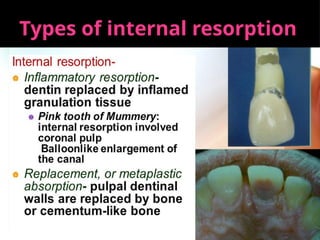
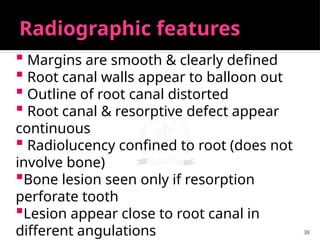
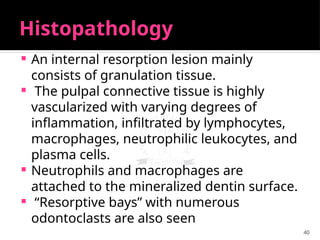
The document discusses regressive alterations in teeth including pulp calcification and hypercementosis, which are common phenomena that can occur with age and various systemic diseases. It outlines types of pulp calcifications, their etiology, clinical features, and treatment, including the significance of tooth resorption, both external and internal. Additionally, it describes the histological and radiographic features associated with these conditions, emphasizing the importance of early identification and treatment options.