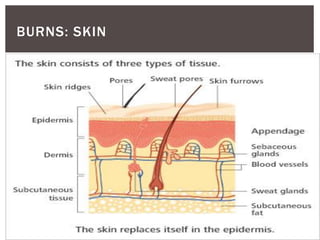
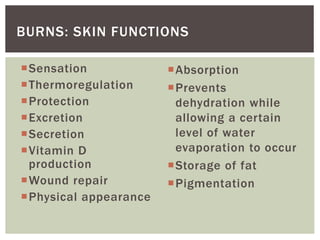
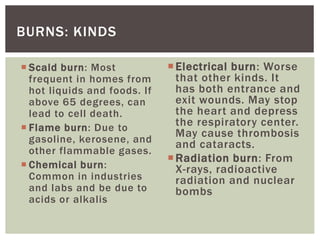
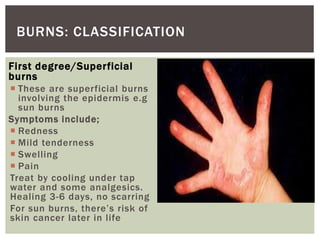
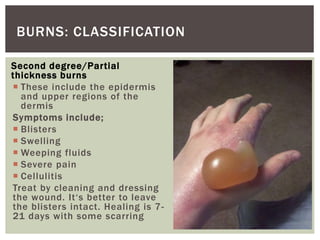
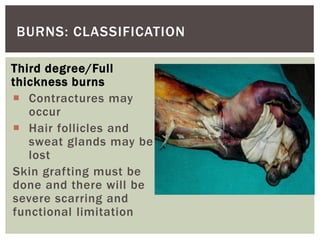
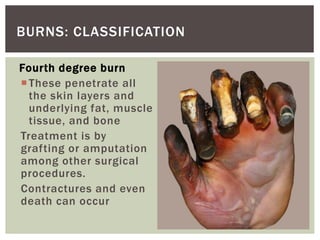
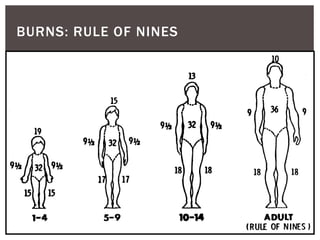
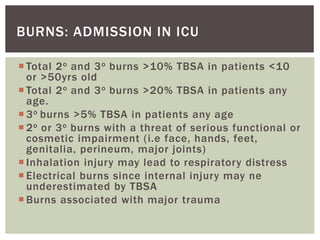
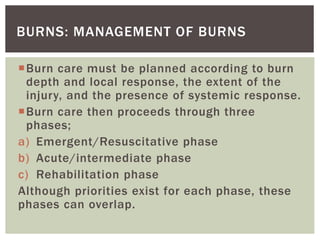
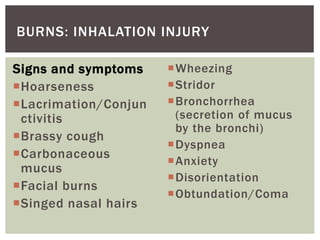
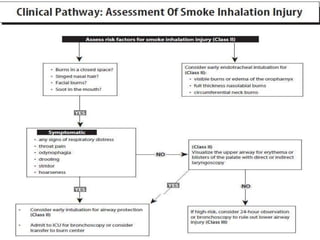
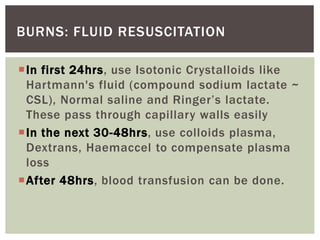
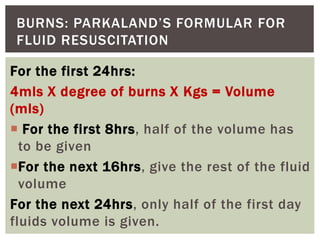
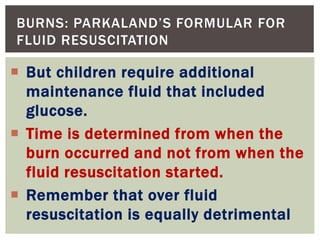
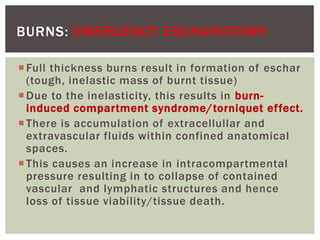
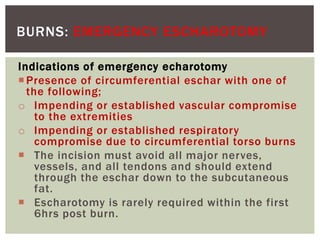
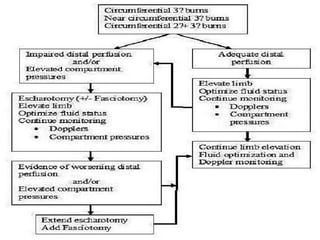
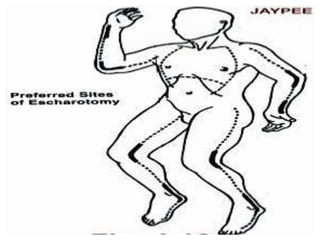
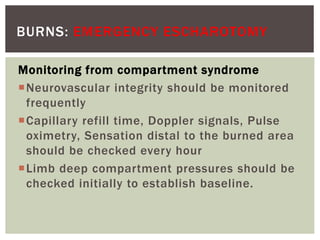
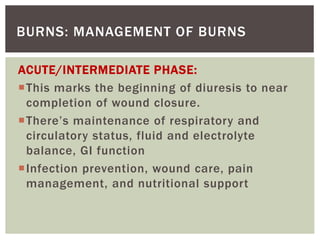
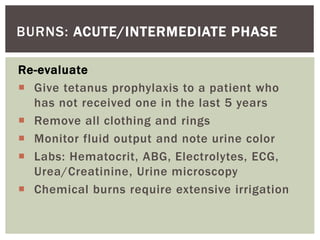
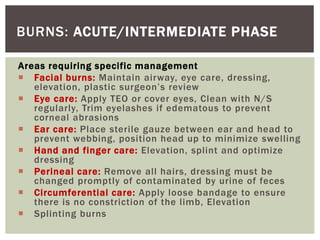
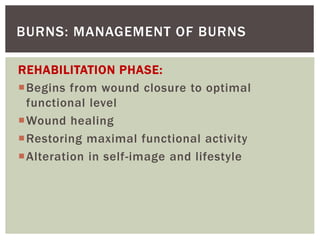
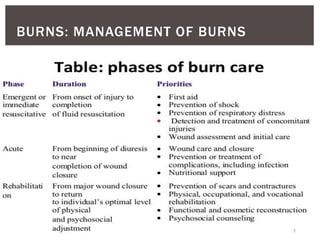
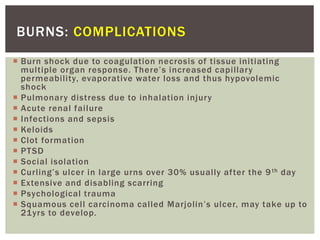
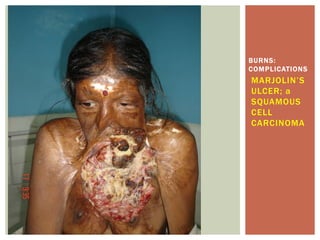
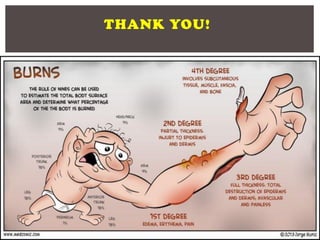
The document provides comprehensive information on burn types, classifications, symptoms, treatment, and management strategies, categorizing burns into first, second, third, and fourth degrees, each with unique characteristics and healing processes. It outlines the importance of fluid resuscitation, infection prevention, pain management, and strategies to enhance healing, emphasizing detailed protocols for emergency care and rehabilitation phases. Additionally, it highlights potential complications from burns, including physical, psychological, and functional implications.