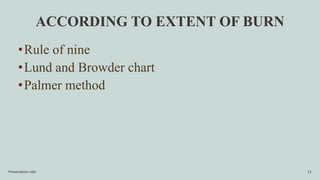
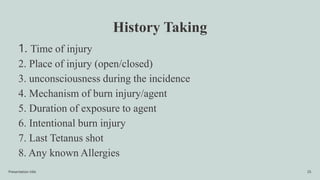
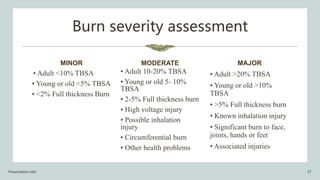
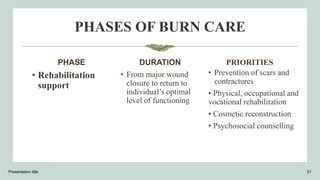
This document provides an overview of burns, including their anatomy, physiology, classification, treatment, and management. It begins with definitions of burns and classifications according to depth and extent. It then discusses the standard phases of burn care - the emergent/resuscitative phase focuses on fluid resuscitation and wound care, the acute/intermediate phase on preventing infection and wound closure, and the rehabilitation phase on minimizing scarring and functional loss. Complications are also reviewed. The document aims to give healthcare practitioners an understanding of burns and their multifaceted management.