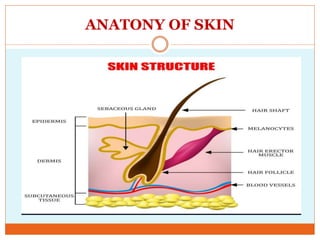
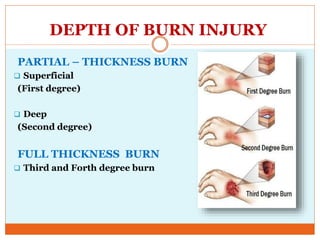
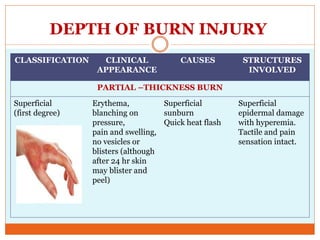
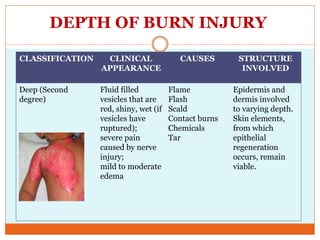
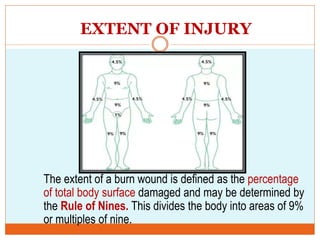
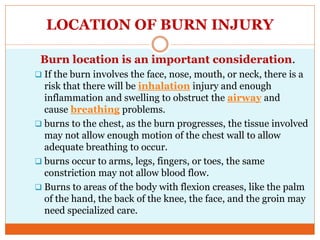
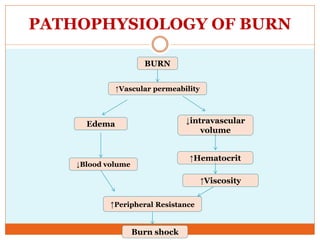
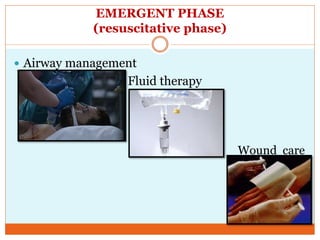
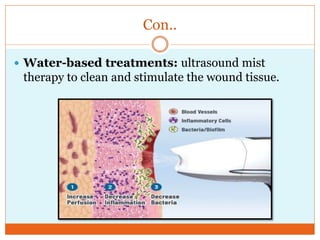
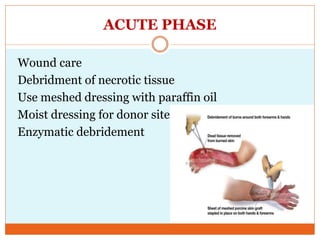
This document provides information on burns including definitions, causes, classifications, management, and complications. It defines a burn as an injury caused by heat, cold, electricity, chemicals, friction or radiation. Burns are classified based on depth (partial thickness or full thickness) and extent (percentage of total body surface area affected). Management involves addressing airway, breathing, circulation, fluid resuscitation, wound care including cleaning, dressing and grafting, pain management, nutrition, and rehabilitation. Complications can include shock, infection, scarring and long term psychological impacts.