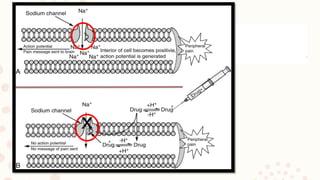
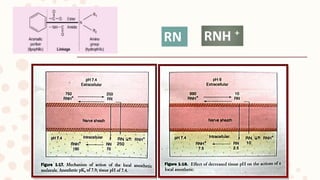
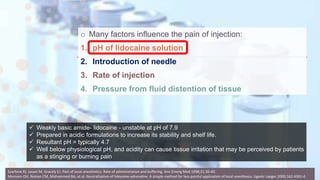
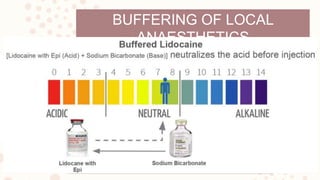
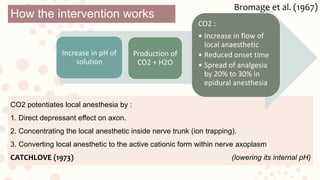
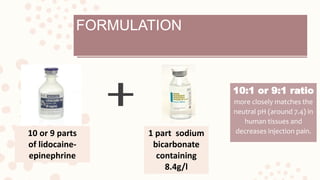
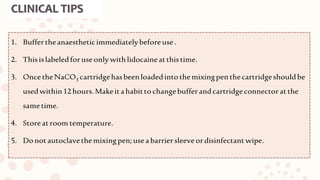
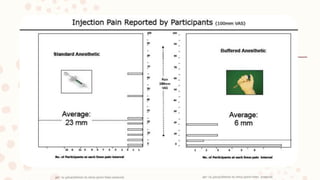
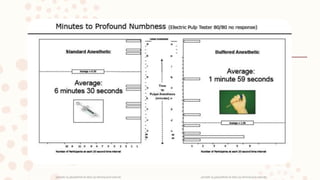
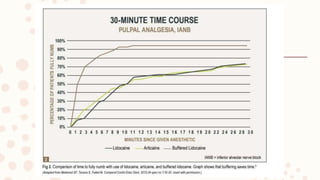
The document discusses the mechanisms of buffered local anaesthetics, particularly lidocaine, and factors that affect pain during injection, such as pH and injection rate. It emphasizes the benefits of buffering, including faster onset and reduced pain, while outlining clinical tips and considerations for use. The conclusion highlights that buffered local anaesthetics significantly increase the likelihood of successful anesthesia with minimal discomfort.