protocol 1 chetan final.pdf
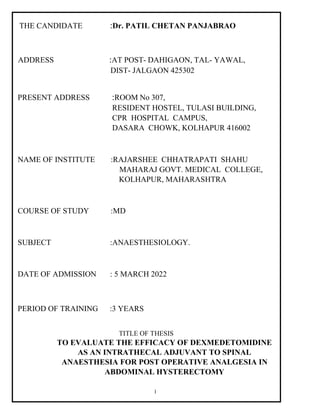
- 1. 1 THE CANDIDATE :Dr. PATIL CHETAN PANJABRAO ADDRESS :AT POST- DAHIGAON, TAL- YAWAL, DIST- JALGAON 425302 PRESENT ADDRESS :ROOM No 307, RESIDENT HOSTEL, TULASI BUILDING, CPR HOSPITAL CAMPUS, DASARA CHOWK, KOLHAPUR 416002 NAME OF INSTITUTE :RAJARSHEE CHHATRAPATI SHAHU MAHARAJ GOVT. MEDICAL COLLEGE, KOLHAPUR, MAHARASHTRA COURSE OF STUDY :MD SUBJECT :ANAESTHESIOLOGY. DATE OF ADMISSION : 5 MARCH 2022 PERIOD OF TRAINING :3 YEARS TITLE OF THESIS TO EVALUATE THE EFFICACY OF DEXMEDETOMIDINE AS AN INTRATHECAL ADJUVANT TO SPINAL ANAESTHESIA FOR POST OPERATIVE ANALGESIA IN ABDOMINAL HYSTERECTOMY
- 2. 2 FOR SUBMITTING PLAN OF WORK OF RESEARCH PROJECT 1)Title of Research Project: "TO EVALUATE THE EFFICACY OF DEXMEDETOMIDINE AS AN INTRATHECAL ADJUVANT TO SPINAL ANAESTHESIA FOR POST OPERATIVE ANALGESIA IN ABDOMINAL HYSTERECTOMY” 2)Name & Designation of: a. Post Graduate Guide: DR. MARUTI PAWAR ASSOCIATE PROFESSOR, DEPT. OF ANAESTHESIOLOGY, RAJARSHEE CHHATRAPATI SHAHU MAHARAJ GOVERNMENT MEDICAL COLLEGE . KOLHAPUR. b. Post Graduate Student: Dr. PATIL CHETAN PANJABRAO MD TRAINEE IN ANAESTHESIOLOGY RAJARSHEE CHHATRAPATI SHAHU MAHARAJ GOVERNMENT MEDICAL COLLEGE KOLHAPUR. 3)Duration of Research Project: 2 Years a.Period which may be needed: January 2023 to December for collection of data 2023 b. Deadline for collecting data: December 2023 c. Period that may be required for analysing the data: January 2024 . to July 2024 d. Deadline for analyzing the data: July 2024
- 3. 3 4)Review of progress of the Research project: Every 3 months a. Review of collected data date: 31 December 2023 b. Review of analysing data date: 31 July 2024 5)Date of Registration: 6) Date of appearing for Examination: 7)Signature: a. Post Graduate Student: b. Post Graduate guide: c. Head of Dept. of concerned subject: d. Head of Dept. of supporting subject: e. Remarks and signature of secretory of Ethical committee: APPROVED / DISAPPROVED DATE: PLACE:KOLHAPUR.
- 4. 4 INDEX SR.NO. CONTENT 1 INTRODUCTION 2 REVIEW OF LITERATURE 3 AIMS AND OBJECTIVES 4 MATERIAL AND METHODS 5 REFERENCES 6 ANNEXURE 6.1 STUDY PROFORMA 6.3 INFORMED CONSENT FORM 7 APPROVAL OF ETHICAL COMMITTEE AND IT’S COMPOSITION 8 APPROVAL OF SCIENTIFIC COMMITTEE AND IT’S COMPOSITION
- 5. 5 INTRODUCTION Pain after gynaecological surgeries is often underrated as it is assumed to be associated with lower pain intensity. This under treatment of pain leads to patient dissatisfaction and other complications. The patient mobility, length of hospital stay and recovery can be hastened by using different analgesic methods. Different modalities of pain management have been effectively used and compared with each other. Abdominal Hysterectomy is one of the most common surgical procedures performed and post‑operative pain associated with it may be moderate to severe. It is associated with delayed return to normal daily activities and may also be related to persistent post‑surgical pain . The major goal in the management of post‑operative pain is minimizing the dose of medications to lessen side effects while still providing adequate analgesia. Various modalities available to control pain after surgery include pharmacological methods, topical analgesics, regional nerve block techniques. They offer a great degree of post‑operative pain relief thus facilitating early ambulation and discharge. Among these modalities regional anaesthetic techniques have proven to be superior in providing satisfactory pain control. One of the basic reasons to add neuraxial adjuvant drugs to intrathecal (IT) or spinal heavy levobupivacaine is to prolong the duration of sensory block thereby providing an extended postoperative pain relief. Our clinical experience suggests that patients undergoing any surgical procedures on uterus usually experience a mild to moderate degree of pain in the immediate postoperative period. This type of pain is usually poorly localized visceral pain and adds to more discomfort than pain to the patient. As most of these procedures are done under spinal anaesthesia, adding a neuraxial adjuvant not only prolongs the duration
- 6. 6 of postoperative analgesia but is also effective in attenuating this poorly localized visceral pain. A number of adjuvants have been added to local anesthetic agents for subarachnoid block to prolong the intra and post operative analgesia. Nonetheless, agents such as clonidine, midazolam, opioids, and neostigmine are associated with varying side effects profile.Opioids are commonly used adjuvant, they produce rapid onset and good quality of surgical block but with side effects such as pruritus, nausea, and vomiting. These prompted further search toward non opioid analgesic. Dexmedetomidine an α2–adrenergic receptor agonist which causes anxiolysis, sedation, analgesia and is sympatholytic with minimal respiratory depression but prolongs the postoperative analgesic effect with minimal side effects. However, there is a paucity of reports in our environment. This study seeks to validate the postoperative analgesic effect produced by intrathecal administration of dexmedetomidine with levobupivacaine for Abdominal Hysterectomies.
- 7. REVIEW OF LITERATURE Minagar M et al. [1] conducted a study to evaluate effects of adding Dexmedetomidine to hyperbaric bupivacaine in lower abdominal surgeries under spinal anaesthesia. Main outcomes were considered pain score, duration of analgesia, hemodynamic changes and adverse side effects like nausea and vomiting. 50 person receive 12.5 mg hyperbaric bupivacaine + 5 µg dexmedetomidine intrathecally while 50 person receive 12.5 mg hyperbaric bupivacaine + 0.5 cc Normal Saline intrathecally. The study concluded that intrathecal dexmedetomidine increases duration of analgesia and reduces post operative pain without changes in hemodynamic parameters and adverse side effects. Gupta R et al. [2] conducted a study aimed to determine efficacy and safety of intrathecal dexmedetomidine added to ropivacaine. Sixty patients were randomly allocated to receive intrathecally either 3 ml of 0.75% isobaric ropivacaine + 0.5 ml normal saline (Group R) or 3 ml of 0.75% isobaric ropivacaine + 5 μg dexmedetomidine in 0.5 ml of normal saline (Group D). The mean time of sensory regression to S2 was 468.3±36.78 minutes in group D and 239.33±16.8 minutes in group R. Duration of analgesia (time to requirement of first rescue analgesic) was significantly prolonged in group D (478.4±20.9 minutes) as compared to group R (241.67±21.67 minutes). The maximum visual analogue scale score for pain was less in group D (4.4±1.4) as compared to group R (6.8±2.2). The study concluded that addition of dexmedetomidine to ropivacaine intrathecally produces a prolongation in the duration of the motor and sensory block. Farokhmehr L et al. [3] studied the effect of different doses of intrathecal dexmedetomidine on hemodynamic parameters and block characteristics after ropivacaine spinal anesthesia in lower-limb orthopedic surgery. In a double-blind trial, 90 patients unundergoing spinal anesthesia for lower-limb orthopedic surgery were included and then randomly assigned to three groups;
- 8. 8 dexmedetomidine 5 μg/kg, dexmedetomidine 10 μg/kg and placebo. Blood pressure, heart rate, and oxygen saturation were recorded in the three groups at the first 15 minutes and then every 15 to 180 minutes at recovery by a resident anesthesiologist, as well as sensory-motor block onset. The visual analog scale scores for the assessment of pain were recorded at recovery, and 2, 4, 6, and 12 hours postoperatively. The Bromage score was higher in the 10 μg/kg dexmedetomidine group (P = 0.0001) with lower pain score as compared with the 5 μg/kg dexmedetomidine and placebo groups (P = 0.0001). Therefore, an increase in dexmedetomidine hastens the onset of sensory-motor block but not causes side effects. Khosravi F et al. [4] did a Comparative Study of Fentanyl vs Dexmedetomidine as Adjuvants to Intrathecal Bupivacaine in Cesarean Section. This study involved 110 pregnant women with ASA I and II and gestational age ≥37 weeks who were candidates for elective cesarean section. They were randomly divided into two groups of 55; Group B-D received 10 mg bupivacaine (0.5%) + 5 μg dexmedetomidine and Group B-F received 10 mg bupivacaine (0.5%) + 25 μg fentanyl, intrathecally. The onset of block, duration of analgesia, the score of pain intensity, hemodynamic changes, Apgar scores, and any adverse events were evaluated. P-value <0.05 was considered statistically significant. It concluded that compared with fentanyl, it seems that adding 5 μg dexmedetomidine to bupivacaine has a better effect on postoperative pain management in cesarean section under spinal anesthesia. Shukla U et al. [5] did a clinical comparison with Dexmedetomidine versus midazolam as adjuvants to intrathecal bupivacaine. A total of 80 patients, scheduled for vaginal hysterectomies, were randomly allocated to Group D (n = 40) to receive intrathecally 3.0 mL 0.5%
- 9. hyperbaric bupivacaine +5 ug dexmedetomidine in 0.5 mL of normal saline; and Group M (n = 40) to receive 3 mL of 0.5% hyperbaric bupivacaine +2 mg midazolam in 0.4 mL (5 mg/mL) +0.1 mL normal saline. The onset, duration of sensory and motor block, time to first postoperative analgesia and side effects were noted. The study concluded intrathecal dexmedetomidine was better adjuvant than midazolam as it produces significantly longer duration of sensory block, reduced doses of postoperative analgesic agents with comparable side-effects. Gupta M et al. [6] studied effect of 3 Different Doses of Intrathecal Dexmedetomidine (2.5µg, 5µg, and 10 µg) on Subarachnoid Block Characteristics. To elucidate the dose-response relationship between ITD and subarachnoid block characteristics, particularly the duration of analgesia and differential analgesia (DA: defined as time difference from the offset of motor blockade to the first analgesic requirement on numerical rating scale = 4.0). Ninety adult (18 - 60 years) patients undergoing elective lower abdominal and lower limb surgeries were randomized into 3 groups to receive intrathecal 0.5% bupivacaine 3 mL with 2.5 µg (group BD2.5), 5µg (group BD5), or 10 µg (group BD10) dexmedetomidine in 0.5 mL normal saline. The 2 segment sensory regression times (TSSRT), duration of motor blockade analgesia, DA, and perioperative adverse effects were assessed. The study concluded that the addition of 10 µg compared with 2.5 µg or 5µg ITD to 0.5% hyperbaric bupivacaine is associated with significantly earlier onset of sensory and motor block as well as prolonged duration of sensory block, motor block, analgesia, and DA with a comparable adverse effect profile.
- 10. 10 AIMS AND OBJECTIVES Aim : To evaluate the efficacy of intrathecal Dexmedetomidine as an adjuvant to Levobupivacaine in spinal anaesthesia in patients undergoing Abdominal Hysterectomy. Objectives: 1. To evaluate the duration of analgesia post operatively using Visual Analogue Scale (VAS). 2. To evaluate total duration of sensory and motor block. 3. To evaluate intra operative hemodynamic changes and side effects.
- 11. Material and Methods Study Area Department of Anesthesiology of a tertiary care hospital. Study Population All female patients undergoing Abdominal Hysterectomy in our hospital. Sample Size Sample size was determined by using the effect sizes from previously published study by using this formula. [Z1-α/2√{2P(100-P)} + Z 1-β√{P1(100-P1)+P2(100-P2)}]² P1-P2 where, n - sample size z - normal deviant at the portion of 95% confidence interval = 1.96 p – prevalence value of post operative pain in Abdominal Hysterectomy (92.7%) With prevalence of post operative pain 92.7% and 5% absolute error, at 95% confidence interval sample size is 104. Study Design A Randomized control study Study Duration 2 Years
- 12. INCLUSION CRITERIA 1. Patients willing to participate in study 2. Patients with age between 18-65 years and who belong to American Society of Anaesthesiologists (ASA) physical status grade I and II. 3. Patients posted for Abdominal Hysterectomy. EXCLUSION CRITERIA 1. Patients refusal. 2. Those with contraindication to spinal anaesthesia. 3. ASA status grade III and IV. 4. Allergy to local anaesthetic or adjuvant medication. 5. Patients with bleeding diathesis or coagulopathy. 6. Local infection at the site of subarachanoid block. 7. Patient requiring other stronger analgesics other than injection Tramadol within 24 hr.
- 13. Methodology A.After approval of institutional ethical committee and taking written informed consent from the participating patients, the patients will be randomly allocated to 2 groups (Group I and Group II) of 52 each. Group I will receive 3 ml of 0.5% Hyperbaric Levobupivacaine (15 mg) and 0.5 ml normal saline (total 3.5ml). Group II will receive 3 ml of 0.5% Hyperbaric Levobupivacaine (15 mg) with 10 μg Dexemedetomidine made up to 0.5 ml with normal saline (total 3.5 ml). B. Standard pre-operative, intra-operative and post-operative protocols will be followed. C. During the pre-anaesthetic check-up patients will be explained about VAS and the level of analgesia in the postoperative period will be recorded with score 0 indicating no pain and 10 indicating severe pain.Baseline parameters like pulse, blood pressure; ECG will be measured before the surgical procedure. Intravenous line will be secured and patients preloaded with Ringer’s lactate 10 ml/kg body weight over 20 to 30 minutes. D.All spinal blocks will be administered with patient in sitting position using the midline approach at L2-3 or L3-L4 vertebral interspaces. Skin infiltration will be done by raising a wheal with 0.5ml of 2% Lignocaine plain. The subarachnoid space will be entered using a 25-gauze Quincke’s spinal needle. Once free flow of Cerebrospinal fluid is recognized, the intrathecal anaesthetic solution in a standardized dose will be injected over 20 seconds. Group I will receive 3 ml of 0.5% Hyperbaric Levobupivacaine (15 mg) and 0.5 ml normal saline (total 3.5ml). Group II will receive 3 ml of 0.5% Hyperbaric Levobupivacaine (15 mg) with 10 μg Dexemedetomidine made up to 0.5 ml with normal saline (total 3.5 ml).Immediately following the injection, patients will be made to lie
- 14. in the supine position. Continuous monitoring of hemodynamic parameters will be done and readings will be recorded every 5 minutes for first 30 minutes, thereafter every 10 minutes till the end of surgery. E. The onset of sensory block will be tested by ‘pin-prick method’ using a hypodermic needle at 2 minutes interval. The time of onset will be taken from the time of injection of drug into subarachnoid space to loss of pinprick sensation. The highest level of sensory block, duration of sensory blockade taken as time from onset to time of return of pinprick sensation to S1(heel) dermatomal area will be noted. VAS will be recorded at an interval of 0,0.5, 1,2,4,6,8,12,24 hours postoperatively. Duration of complete analgesia will be noted and rescue analgesics will be given to the patients when VAS ≥4. The cutoff point of our study will be the time when the patient demand the first dose of rescue analgesia. F. The onset of motor block will be assessed with ‘Modified Bromage Score’. The time interval between injections of drug into subarachnoid space, to the patient’s inability to lift the straight extended leg will be taken as onset time (Bromage 3). The duration of motor block will be taken from time of injection to complete regression of motor block (ability to lift the extended leg) (Bromage 0). Modified Bromage Scale :- • Grade0- Full flexion of knees and feet. • Grade1- Just able to flex knees, full flexion of feet. • Grade2- Unable to flex knees, but some flexion of feet possible. • Grade3- Unable to move legs or feet.
- 15. G. Side effects like sedation, nausea, vomiting, shivering will be monitored in the recovery room and then patient shift to the ward. H. The patients will receive tramadol 2 mg/kg IV if VAS ≥4 in the first 4 h after the surgery. For persistent VAS ≥4 in this period, diclofenac 75 mg IV will be administered. After 4 h, patients will be administered oral diclofenac 75 mg if VAS ≥4. Injection ondansetron (4 mg) IV will be given for post‑operative nausea and vomiting. Post operative analgesia and total analgesic consumption in the 24 h postoperative period will be the primary objective of the study. I. The patients will be interviewed at 0, 0.5, 1, 2, 4, 6, 8, 12 and 24 Hr after surgery. VAS scores at rest and at knee flexion, duration after which first analgesic was demanded by the patient, incidence of nausea, vomiting as well as the overall patient satisfaction will also be observed. J. The data will be entered using Microsoft excel sheet and will be analysed using Statistical Package for Social Sciences (SPSS) version 22.0 software (IBM Corp. Released 2011. IBM SPSS Statistics for windows, Version 20.0. Armonk, NY: IBM Corp.). Catagorical data will be presented in form of frequency and proportion. as test of significance for qualitative data inform of frequency and proportion. Chi‑square test will be used as test of significance for qualitative data.Continous data like VAS score will be analysed using mean and standard deviation and Mann-Whitney U test A probability of P < 0.05 will considered statistically significant.
- 16. References [1] Nwachukwu C, Idehen HO, Edomwonyi NP, Umeh B. Postoperative analgesic effect of intrathecal dexmedetomidine on bupivacaine subarachnoid block for open reduction and internal fixation of femoral fractures. Niger J ClinPract. 2020 Feb;23(2):172- 178. doi: 10.4103/njcp.njcp_142_19. PMID: 32031091 [2] Minagar M, Alijanpour E, Jabbari A, Rabiee SM, Banihashem N, Amri P, Mir M, HedayatiGoodarzi MT, Esmaili M. The efficacy of addition of dexmedetomidine to intrathecal bupivacaine in lower abdominal surgery under spinal anesthesia. Caspian J Intern Med. 2019 Spring;10(2):142-149. doi: 10.22088/cjim.10.2.142. PMID: 31363392; PMCID: PMC6619478. [3] Patro SS, Deshmukh H, Ramani YR, Das G. Evaluation of Dexmedetomidine as an Adjuvant to Intrathecal Bupivacaine in Infraumbilical Surgeries. J ClinDiagn Res. 2016 Mar;10(3):UC13-6. doi: 10.7860/JCDR/2016/17987.7379. Epub 2016 Mar 1. PMID: 27134975; PMCID: PMC4843360. [4] Gupta R, Bogra J, Verma R, Kohli M, Kushwaha JK, Kumar S. Dexmedetomidine as an intrathecal adjuvant for postoperative analgesia. Indian J Anaesth. 2011 Jul;55(4):347-51. doi: 10.4103/0019-5049.84841. PMID: 22013249; PMCID: PMC3190507. [5] Farokhmehr L, Modir H, Yazdi B, Kamali A, Almasi-Hashiani A. Effect of different doses of intrathecal dexmedetomidine on hemodynamic parameters and block characteristics after ropivacaine spinal anesthesia in lower-limb orthopedic surgery: a randomized clinical trial. Med Gas Res. 2019 Apr-Jun;9(2):55-61. doi: 10.4103/2045-9912.260645. PMID: 31249252; PMCID: PMC6607861. [6] Khosravi F, Sharifi M, Jarineshin H. Comparative Study of Fentanyl vs Dexmedetomidine as Adjuvants to Intrathecal Bupivacaine in Cesarean Section: A Randomized, Double-Blind
- 17. Clinical Trial. J Pain Res. 2020 Oct 7;13:2475-2482. doi: 10.2147/JPR.S265161. PMID: 33116789; PMCID: PMC7548853. [7] Shukla U, Prabhakar T, Malhotra K, Srivastava D. Dexmedetomidine versus midazolam as adjuvants to intrathecal bupivacaine: A clinical comparison. J AnaesthesiolClinPharmacol. 2016 Apr-Jun;32(2):214-9. doi: 10.4103/0970-9185.182105. PMID: 27275052; PMCID: PMC4874077. [8] Gautam B, Niroula S, Sharma M, Lama SM. Effects of Intrathecal Dexmedetomidine as an Adjuvant to Hyperbaric Bupivacaine for Spinal Anaesthesia in Adults Undergoing Elective Infra-umbilical Surgery. JNMA J Nepal Med Assoc. 2017 Oct-Dec;56(208):379-87. PMID: 29453466. [9] Kapinegowda ST, Anandswamy TC, Narayanappa VH, Kumar S, Hatti P. To Compare the Effects of Different Doses of Dexmedetomidine on Intrathecal Bupivacaine in Infraumbilical Surgeries: A Prospective, Randomized, Double-blind Clinical Study. Anesth Essays Res. 2017 Oct-Dec;11(4):847-853. doi: 10.4103/aer.AER_257_16. PMID: 29284837; PMCID: PMC5735476. [10] Naaz S, Bandey J, Ozair E, Asghar A. Optimal Dose of Intrathecal Dexmedetomidine in Lower Abdominal Surgeries in Average Indian Adult. J ClinDiagn Res. 2016 Apr;10(4):UC09-13. doi: 10.7860/JCDR/2016/18008.7611. Epub 2016 Apr 1. PMID: 27190922; PMCID: PMC4866220. [11] Gupta M, Gupta P, Singh DK. Effect of 3 Different Doses of Intrathecal Dexmedetomidine (2.5µg, 5µg, and 10 µg) on Subarachnoid Block Characteristics: A Prospective Randomized Double Blind Dose-Response Trial. Pain Physician. 2016 Mar;19(3):E411-20. PMID: 27008297. [12] Singh A, Gupta A, Datta PK, Pandey M. Intrathecal levobupivacaine versus bupivacaine for inguinal hernia surgery: a randomized controlled trial. Korean J Anesthesiol. 2018
- 18. Jun;71(3):220-225. doi: 10.4097/kja.d.18.27191. Epub 2018 Apr 24. PMID: 29684982; PMCID: PMC5995016. [13] Afonso J, Reis F. Dexmedetomidine: current role in anesthesia and intensive care. Rev Bras Anestesiol. 2012 Jan-Feb;62(1):118-33. doi: 10.1016/S0034-7094(12)70110-1. PMID: 22248773. [14] C Paul, G Barasch, Bruce F Collen. Clinical Anaesthesia, 6th edition, Lippincort, Williams and Wilkins, 2006:700-706.
- 19. ANNEXURE CASE RECORD PROFORMA “TO EVALUATE THE EFFICACY OF DEXMEDETOMIDINE AS AN INTRATHECAL ADJUVANT TO SPINAL ANAESTHESIA FOR POST OPERATIVE ANALGESIA IN ABDOMINAL HYSTERECTOMY” DEMOGRAPHIC DATA : Date- Group A / B Name- Age- Yrs Weight- Kgs Blood Group- Adm. No. PREOP ASSESSMENT- Pulse- /min BP- mm Hg Hb- gm% TLC- /cu mm DLC- P- L- M- E- Urine R/M- Any other- ASA physical status- Emergency-Yes/No Time of Spinal anaesthesia – Time of start of surgery - Level of anaesthesia achieved - Time for loss of pin prick sensation in S1- Time for return of pin prick sensation in S1- Time for Modified Bromage Scale Grade 3- Time for return of Modified Bromage Scale Grade 0-
- 20. Vas at rest 0 min 30 min 60 min 2h 4h 6h 8h 12h 24h Group I P Group II P* P** P=value calculated using Mann-whitney test *P value compared with the baseline of the same group **Pvalue comparing both the groups with each other. Time of completion of surgery- HR BP VAS Score Analgesic dose Analgesic time Post op 2 4 6 8 12 24
- 21. Time to first dose of Tramadol (from spinal anesthesia) – Total dose of Tramadol and diclofenac in 24 hrs- COMPLICATIONS - Drowsiness Nausea Vomiting Pruritus Any Other
- 22. CONSENT FORM Subject Identification number for this trial - Title of the project: “ TO EVALUATE THE EFFICACY OF DEXMEDETOMIDINE AS AN INTRATHECAL ADJUVANT TO SPINAL ANAESTHESIA FOR POST OPERATIVE ANALGESIA IN ABDOMINAL HYSTERECTOMY” Name of the principal investigator: DR. . PATIL CHETAN PANJABRAO Tel No: Name: - Age: - Sex: - Address: - I, the undersigned have been duly informed regarding the study undertaken by research trainee Dr.PATIL CHETAN PANJABRAO, his research guide in above said study is Dr. MARUTI PAWAR. The study will be conducted in R.C.S.M., Government Medical College &ChhatrapatiPramilaraje Hospital Kolhapur.All the investigations pertaining to my diagnosis will be conducted with my due consent. The information obtained or used will be maintained confidential. For academic and scientific purpose, the operation / procedure may be televised or photographed At any juncture, I can withdraw from the study without any prior intimation. I am duly informed and agree to participate in this study. During this study period if any health complaint arises I will consult Dr. PATIL CHETAN PANJABRAO Everything is explained to me in my regional language and I have understood it. Signature of Relative: - Signature of Patient: - Relatives Name: - Patients Name: - Relation: - Witnesses:
- 23. INFORMED CONSENT IN MARATHI रुग्ण माहिती पूणण संमतीपत्र “TO EVALUATE THE EFFICACY OF DEXMEDETOMIDINE AS AN INTRATHECAL ADJUVANT TO SPINAL ANAESTHESIA FOR POST OPERATIVE ANALGESIA IN ABDOMINAL HYSTERECTOMY” रुग्णाचे नाव: वय: ल ंग: रुग्णा याचे नाव: नोंदणी क्रमांक: डॉक्टरांचे नाव: मी, खा ी सिी/अंगठा करणार श्री/श्रीमती ............................................. या पत्राद्वारे स्वत:च्या जबाबदारी वर “TO EVALUATE THE EFFICACY OF DEXMEDETOMIDINE AS AN INTRATHECAL ADJUVANT TO SPINAL ANAESTHESIA FOR POST OPERATIVE ANALGESIA IN ABDOMINAL HYSTERECTOMY” “या हवषयाच्या वैद्यकीय अभ्यासासाठी संमती देत आिे या अभ्यासाच्या स्वरुपाची म ा डॉक्टरांनी पूणण कल्पना दद ी आिे व माझ्या सवण शंकाचे समाधानकारक हनरसन के े आिे म ा माहित आिे दक या अभ्यासादरम्यान मी कुठल्यािी क्षणी, कुणा ािी न सांगता िा अभ्यास सोडून जाण्याचा ककंवा सिभागीण िोण्याचा िक्क म ा आिे. माझा आजार, माझ्यावर करण्यात येणार औषधौउपचार आहण तपासण्या इत्याकदंची माहिती संशोधनासाठी वापरण्यास माझी संमती आिे, असे करताना माझी ओळख आहण वैद्यकीय माहिती गोपनीय रािी असे मी गृिीत धरतो/धरते रुग्णाची सिी / अंगठा: ददनांक : साक्षीदाराची सिी: ददनांक: मी वरी अभ्यासाचे स्वरूप, उद्देश आहण त्याचे दुष्पररणामयांची संपूणण माहिती रुग्णास दद ी आिे. डॉक्टरांची सिी: ददनांक . ... . . . . . .
- 24. UNDERTAKING BY THE INVESTIGATOR For submission of Research proposal to Ethics Committee of R.C.S.M GMC & C.P.R Hospital Kolhapur 1] Full name-DR. PATIL CHETAN PANJABRAO Address - Department Of Anaesthesiology, RCSM,GMC&CPR Hospital Kolhapur 2] Name and address of the medical college, hospital or other facility where the clinical trial will be conducted: RCSM, GMC & CPR Hospital Kolhapur 3] Name and address of all clinical laboratory facilities to be used in the study: 4] Name and address of all clinical laboratory facilities to be used in the study: 5] Name and address of the Ethics Committee that is responsible for approval and continuing review of the study. Institutional Ethics Committee, R.C.S.M GMC & C.P.R Hospital Kolhapur 6] Names of the other members of the research team (Co-or sub-Investigators) who will be assisting the Investigator in the conduct of the investigation(s): DR. MARUTI PAWAR Associate Professor Department of Anaesthesiology, RCSM GMC& CPR Hospital Kolhapur
- 25. 7] Protocol Title and study number (if any) of the clinical trial to be conducted by the Investigator. : “TO EVALUATE THE EFFICACY OF DEXMEDETOMIDINE AS AN INTRATHECAL ADJUVANT TO SPINAL ANAESTHESIA FOR POST OPERATIVE ANALGESIA IN ABDOMINAL HYSTERECTOMY” NUMBER OF CASES WILL BE: 104 8] Commitments i. I have reviewed the clinical protocol and agree that it contains all the necessary information to conduct the study. I will not begin the study until all necessary Ethics Committee and regulatory approvals have been obtained. ii. I agree to conduct the study in accordance with the current protocol. I will not implement any deviation from or changes of the protocol without agreement by the Sponsor and prior review and documented approval/favourable opinion from the Ethics Committee of the amendment, except where necessary to eliminate an immediatehazard(s) to the trial Subjects or when the change(s) involved are only logistical or administrative in nature. I agree to personally conduct and/or supervise the clinical trial at my site. iii. I agree to inform all Subjects that the drugs are being used for investigational purposes and I will ensure that the requirements relating to obtaining informed consent and ethics committee review and approval specified in the GCP guidelines are met. iv. I agree to report to the Sponsor all adverse experiences that occur in the course of the investigation(s) in accordance with the regulatory and GCP guidelines. v. I have read and understood the information in the Investigator’s broacher, including the potential risks and side effects of the drug. vi. I agree to ensure that all associates, colleagues and employees assisting in the conduct of the study are suitably qualified and experienced and they
- 26. have been informed about their obligations in meeting their commitments in the trial. vii. I agree to maintain adequate and accurate records and to make those records available for audit/inspection by the Sponsor, Ethics Committee, Licensing Authority or their authorized representatives, in accordance with regulatory and GCP provisions; I will fully cooperate with any study related audit conducted by regulatory officials or authorized representatives of the Sponsor. viii. I agree to promptly report to the Ethics Committee all changes in the clinical trial activities and all unanticipated problems involving risks to human subjects or others. ix. I agree to inform all unexpected serious adverse events to the Sponsor as well as the Ethics Committee within seven days of their occurrence. x. I will maintain confidentiality of the identification of all participating study patients and assure security and confidentiality of study data. xi. I agree to comply with all other requirements, guidelines and statutory obligations as applicable to clinical investigators participating in clinical trails. 9] Signature of Investigators with Name and Date : Principal Investigator : DR PATIL CHETAN PANJABRAO Co-Investigator : DR MARUTI PAWAR ASSOCIATE PROFESSOR DEPARTMENT OF ANAESTHSIOLOGY R.C.S.M GOVT. MEDICAL COLLEGE CPR HOSPITAL,KOLHAPUR