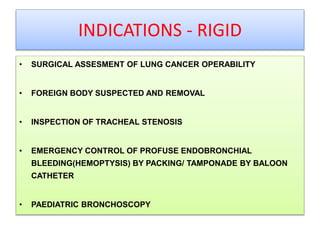
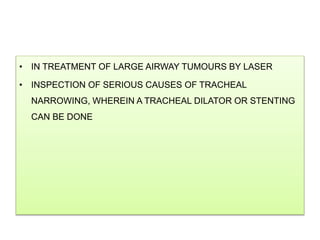
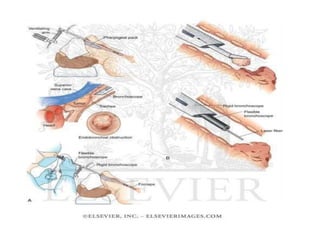
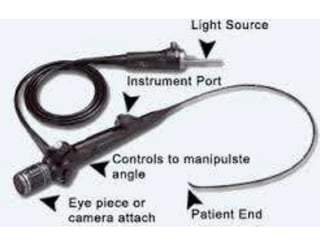
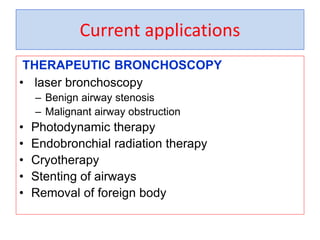
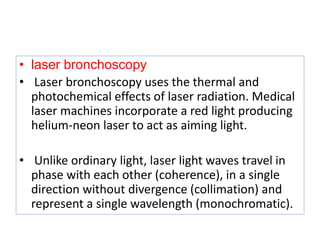
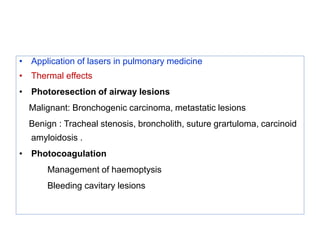
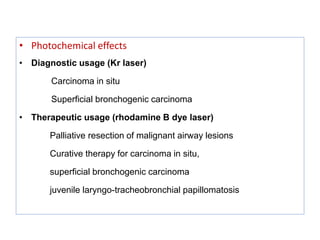
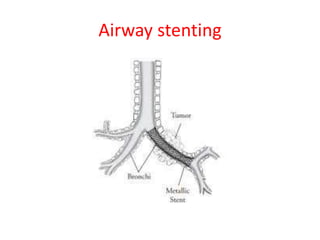
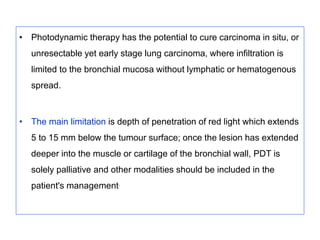
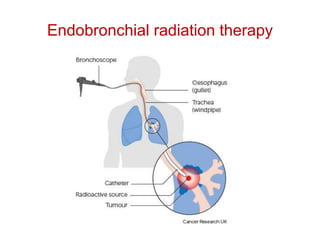
Bronchoscopy is a technique used to visualize the airways for diagnostic and therapeutic purposes. The history began in 1897 with rigid bronchoscopes, but flexible fiberoptic bronchoscopes were invented in 1966, allowing better visualization. Flexible bronchoscopy has now largely replaced rigid bronchoscopy. Bronchoscopy is used for diagnostic and therapeutic procedures like biopsy, foreign body removal, laser therapy, photodynamic therapy, brachytherapy, cryotherapy, and airway stenting.