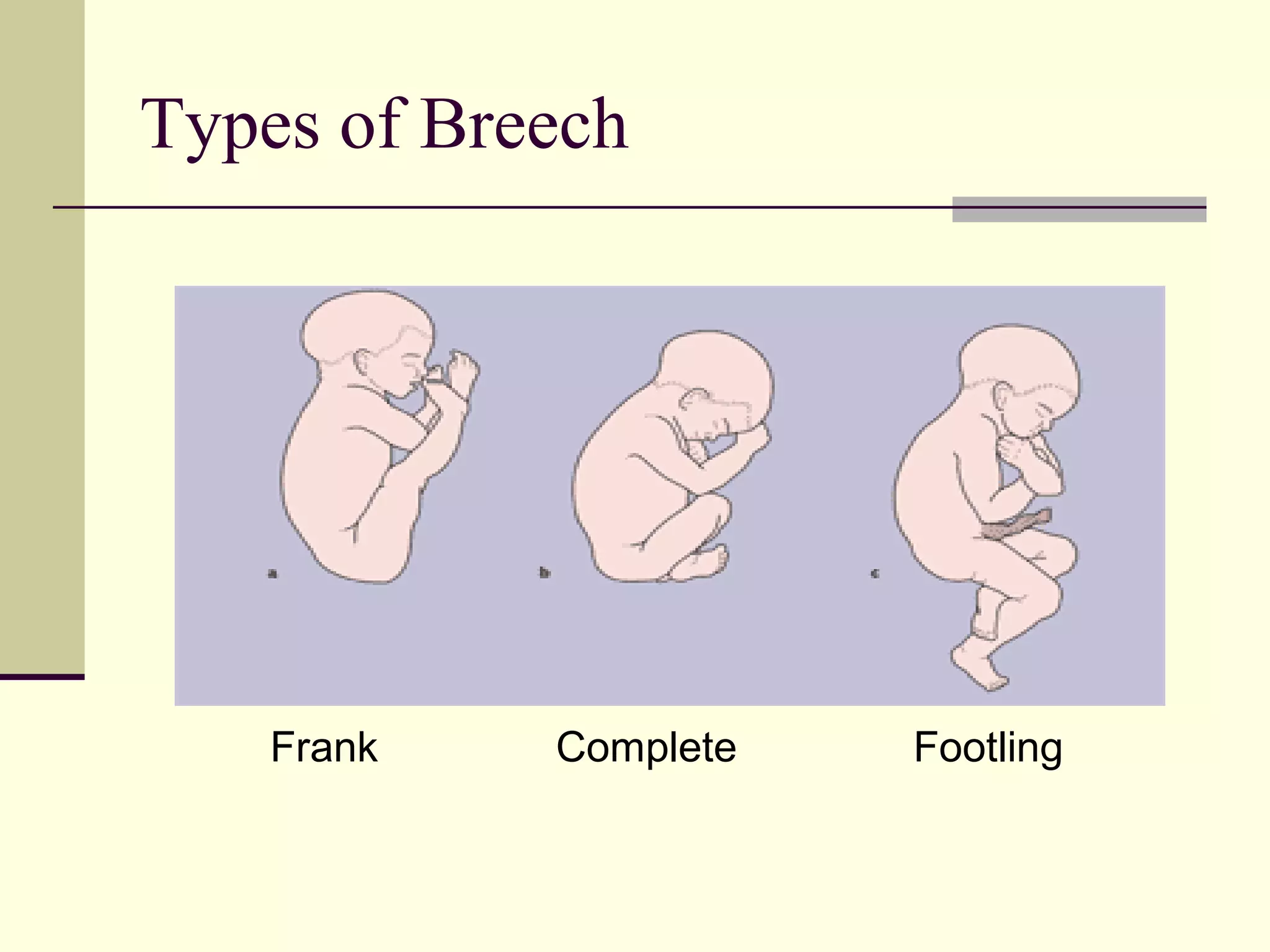
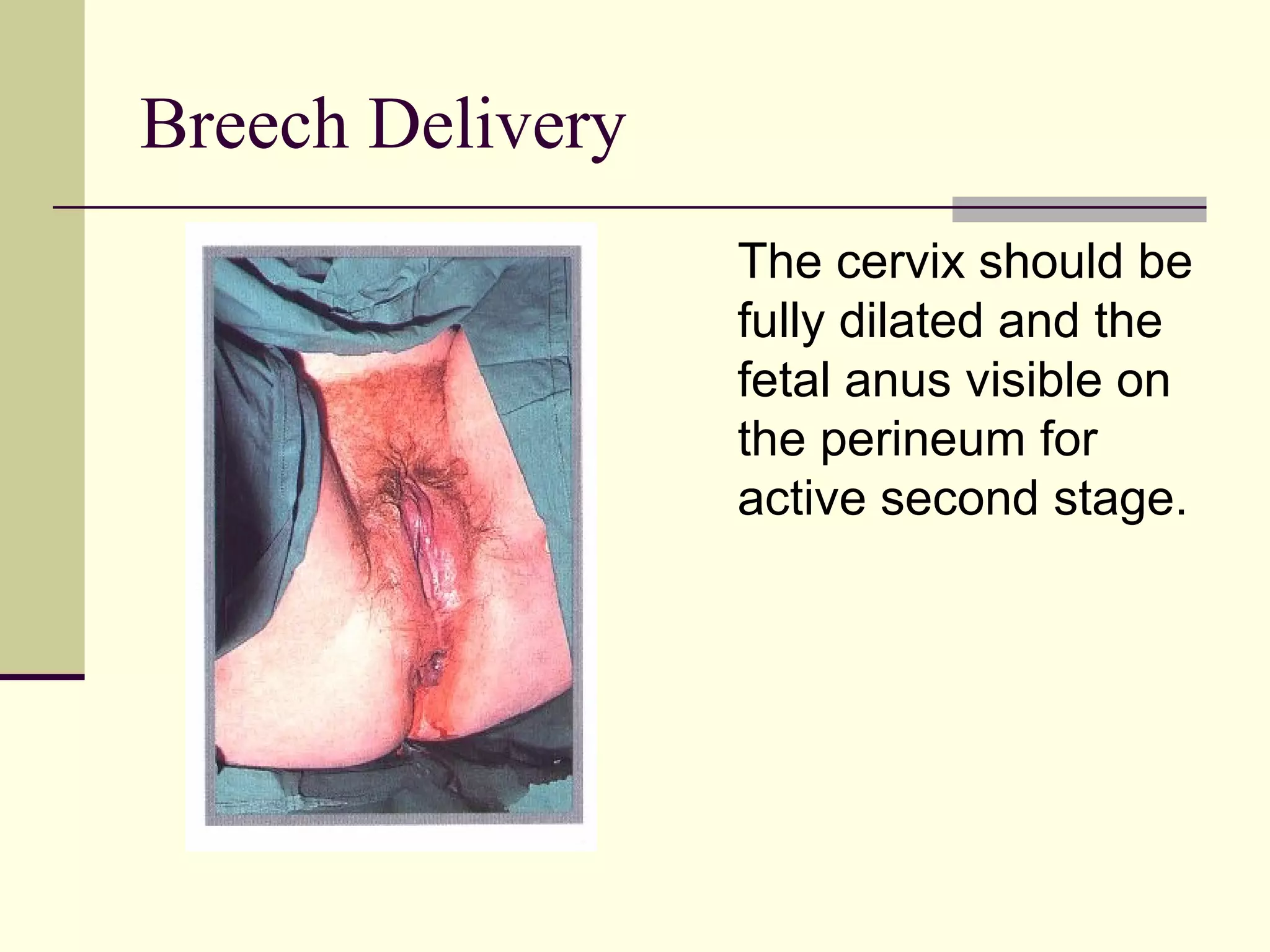
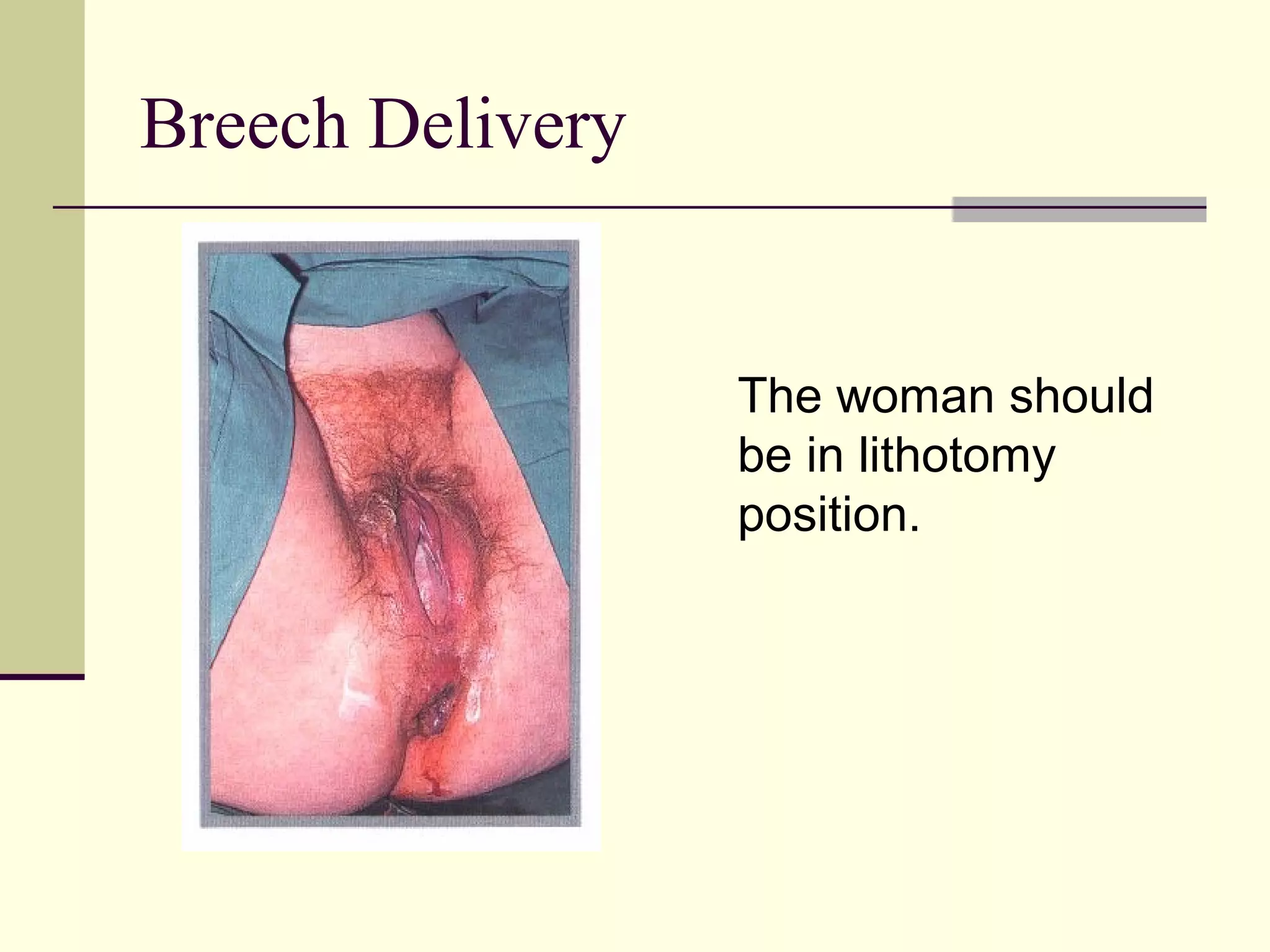
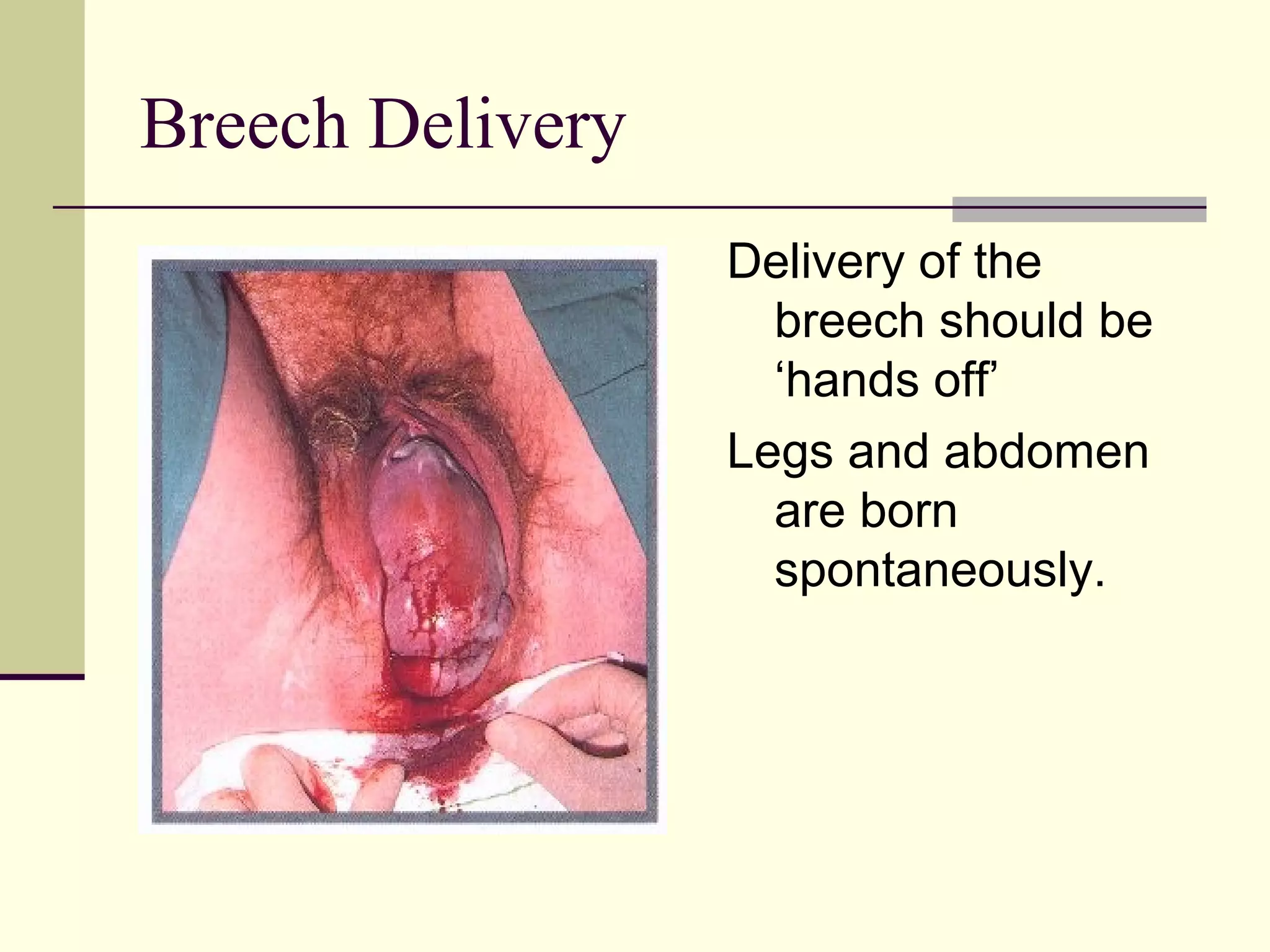
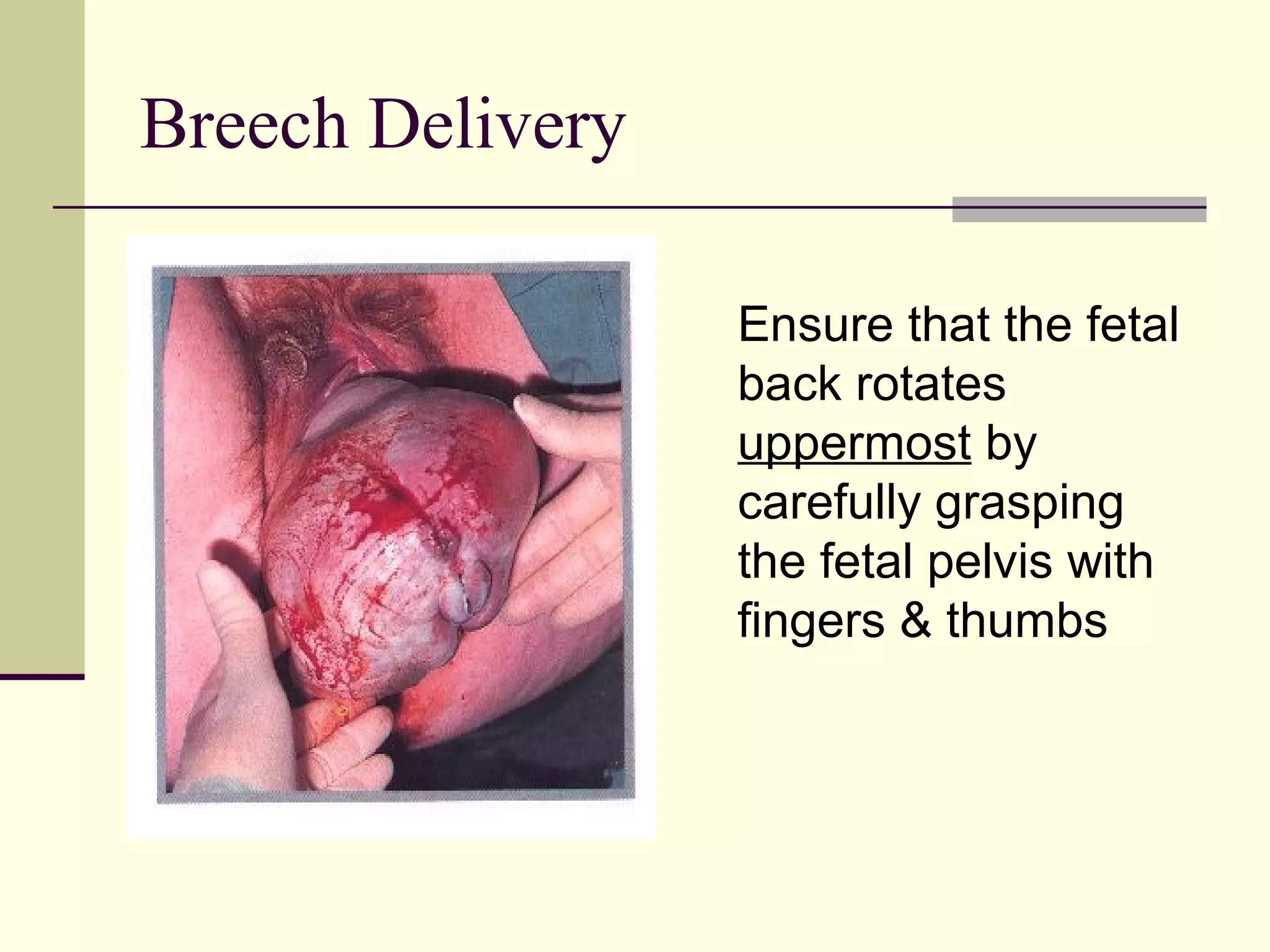
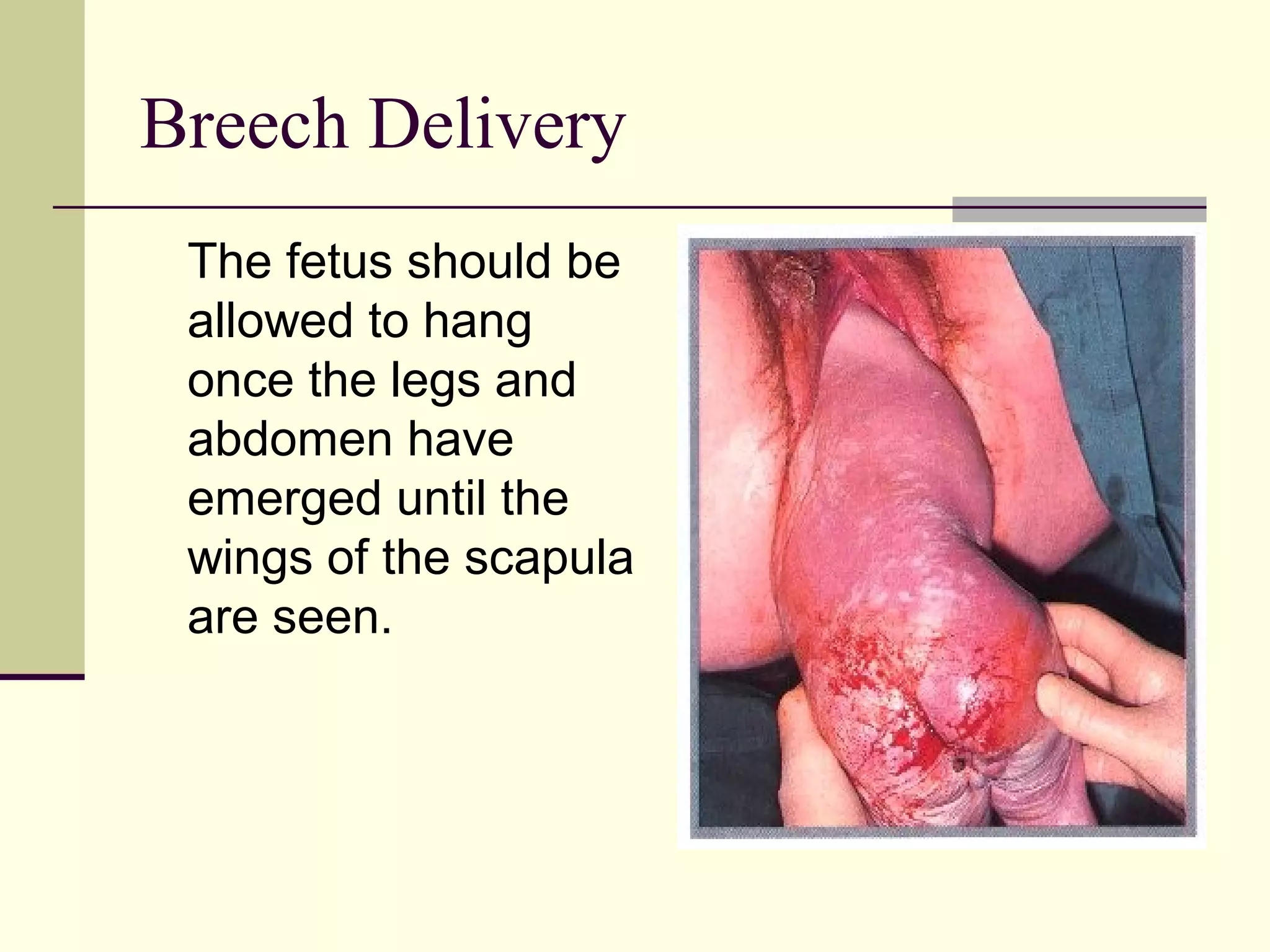
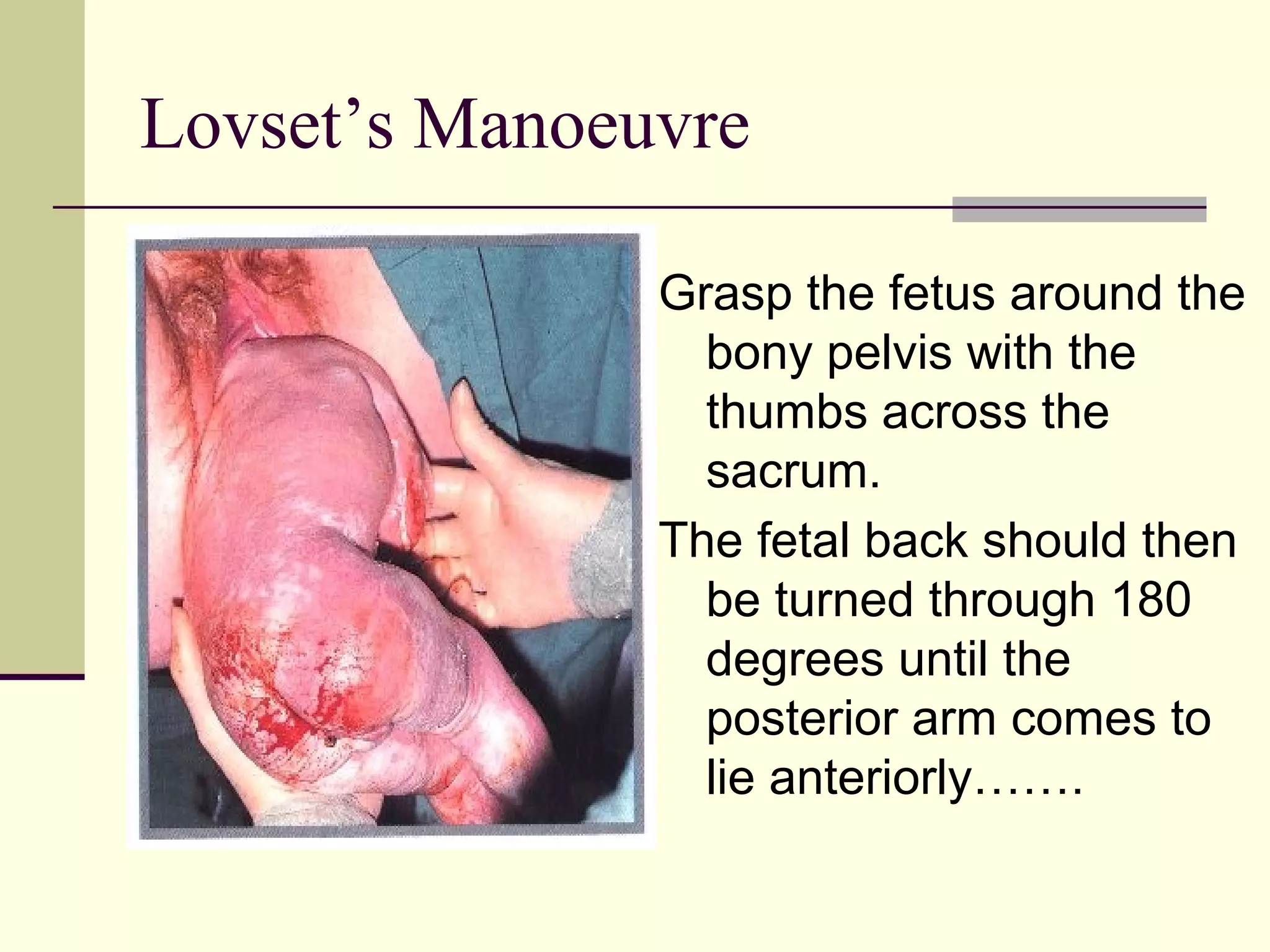
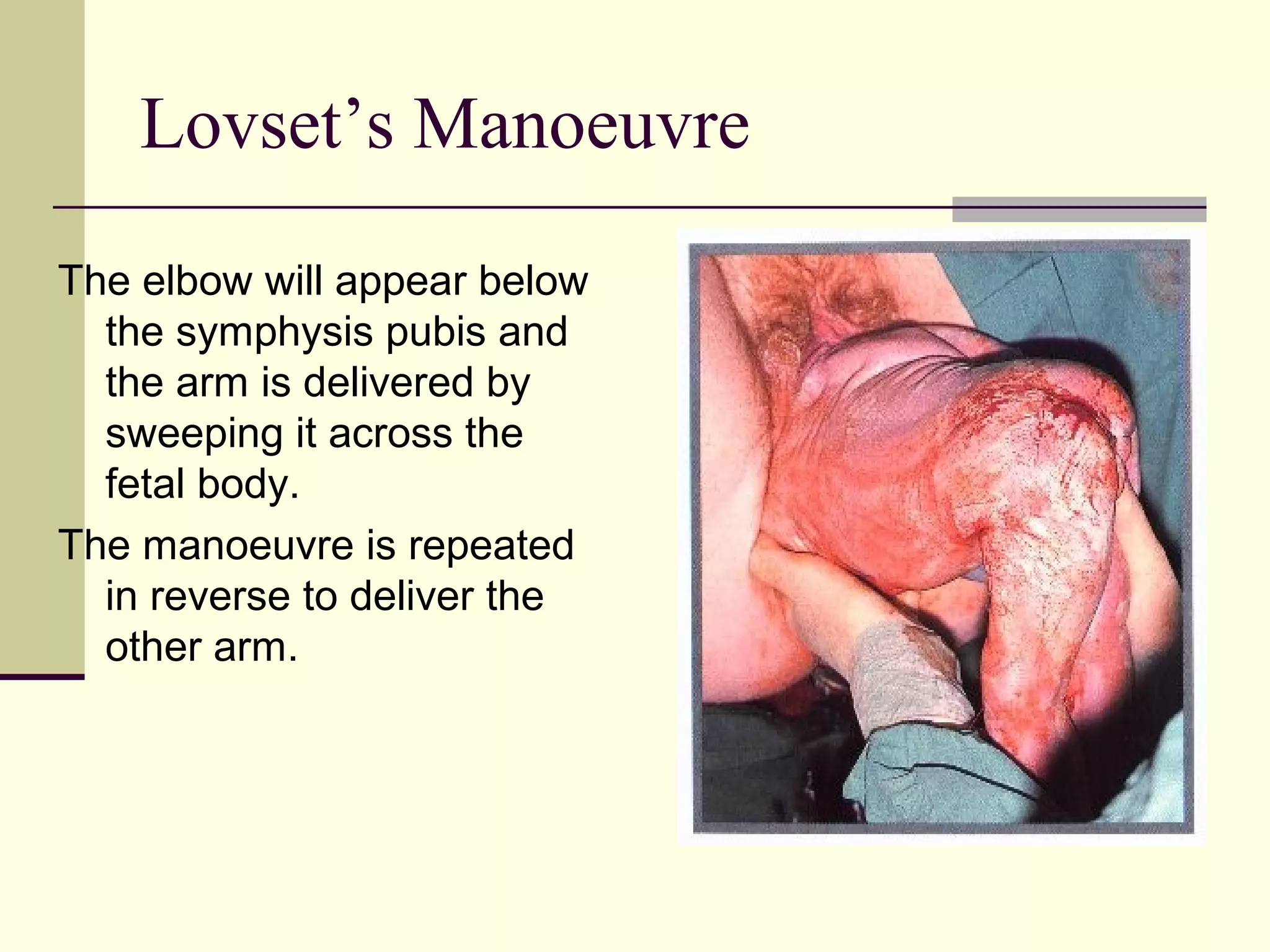
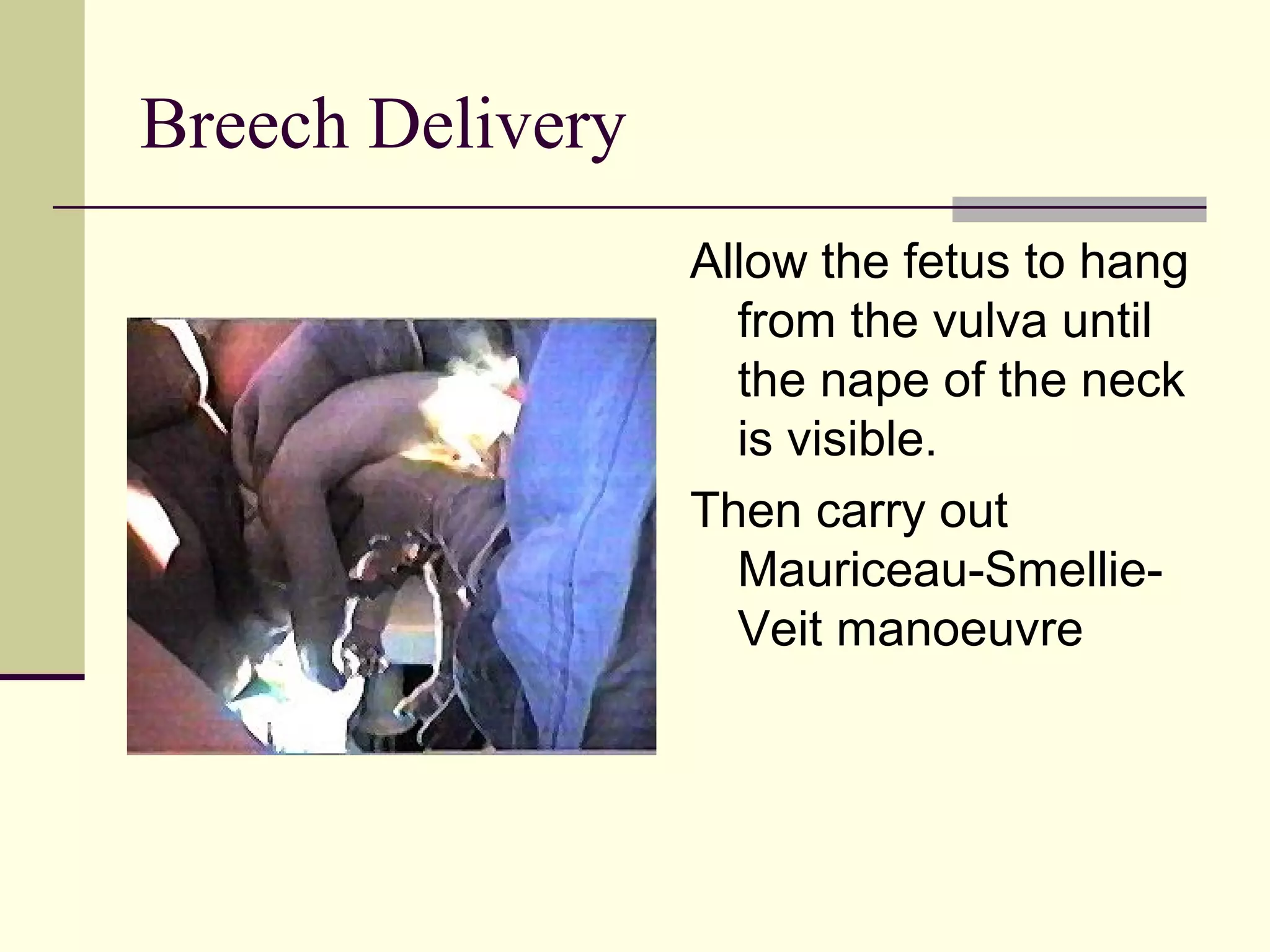
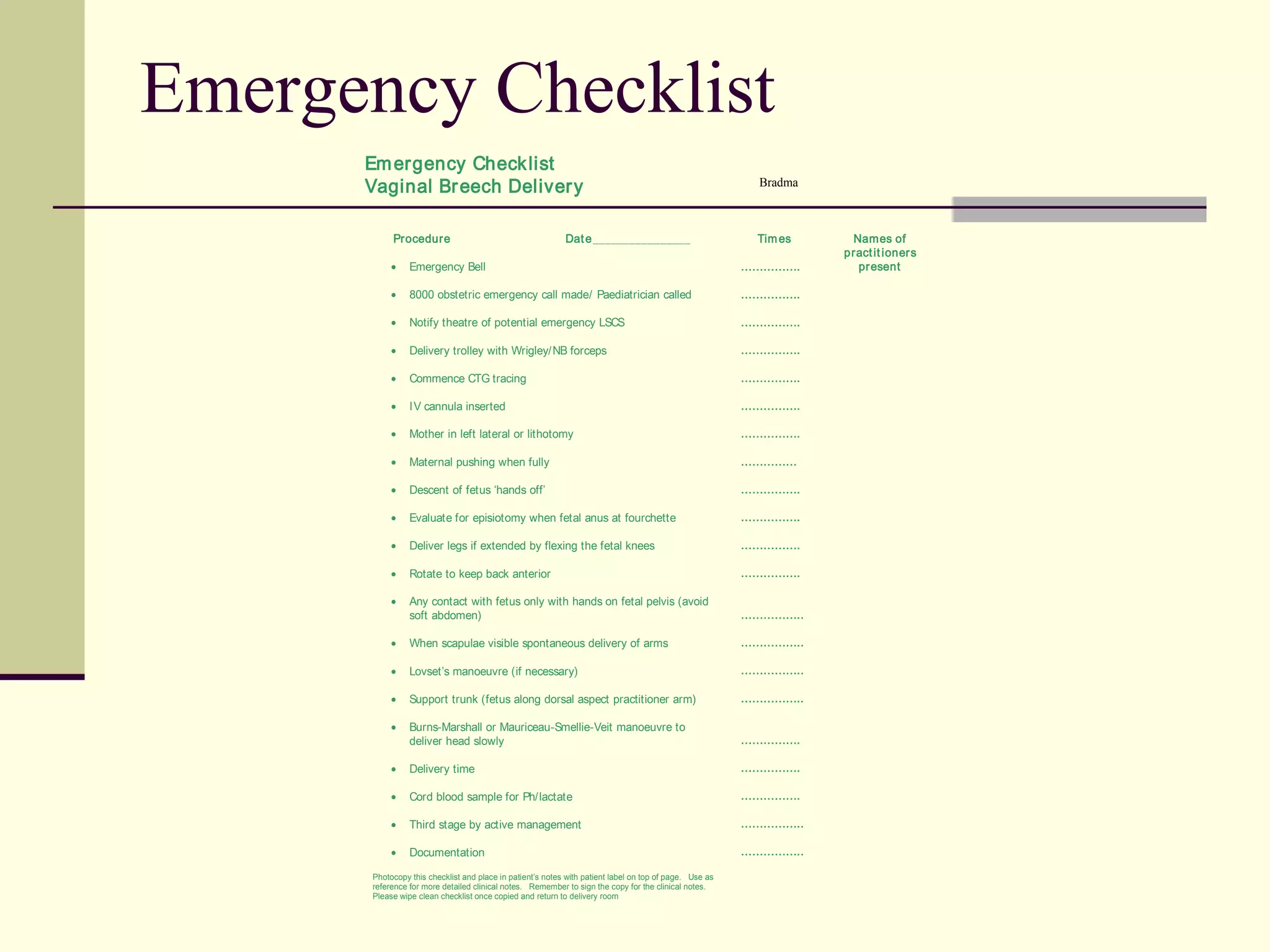
This document discusses the diagnosis and management of breech presentations and breech births. It notes that breech presentations occur in 3-4% of term births. Risk factors include primigravidity, uterine anomalies, and fetal anomalies. For a vaginal breech birth, the cervix must be fully dilated and the fetal anus visible. The breech should be allowed to descend spontaneously and maneuvers like Lovset's may be needed to deliver the arms. The Mauriceau-Smellie-Veit maneuver is then used to slowly deliver the head. Complications may require emergency cesarean section.