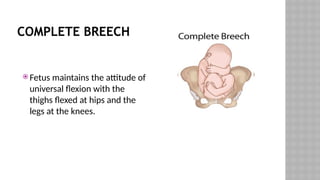
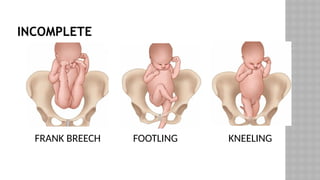
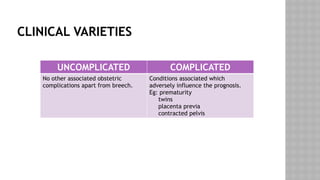
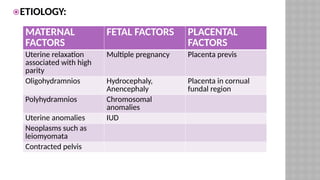
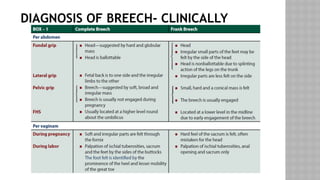
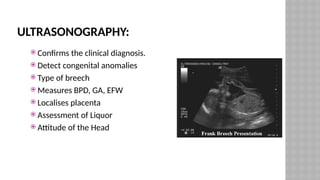
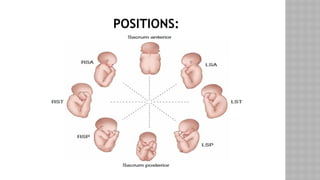
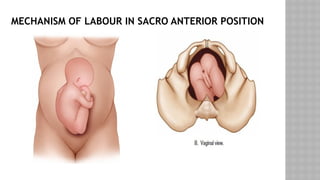
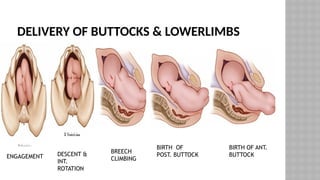
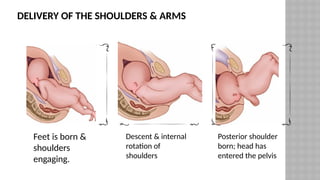
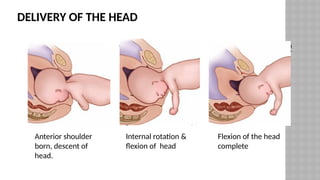
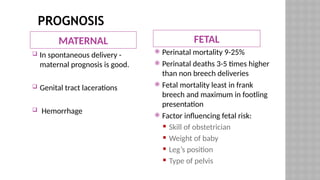
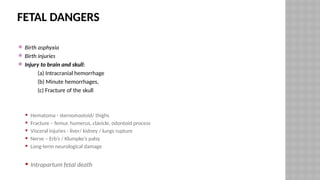
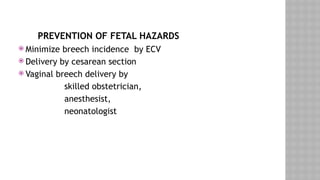
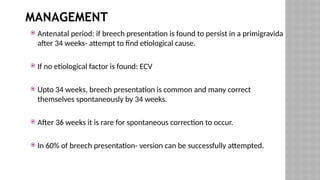
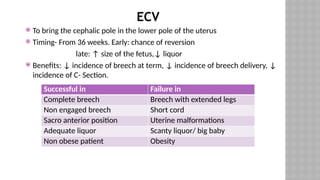
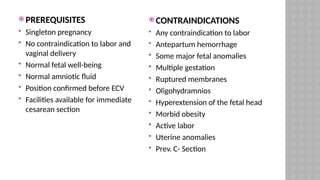
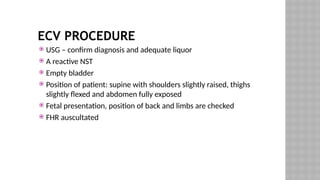
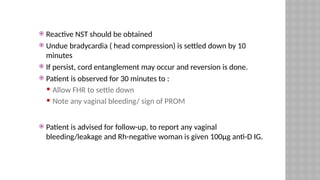
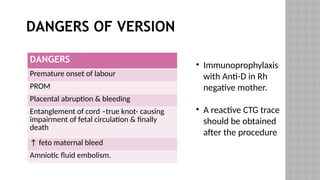
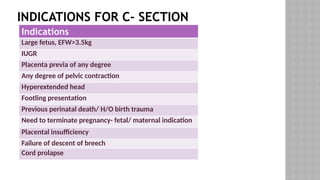
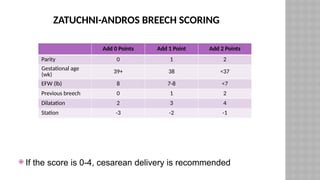
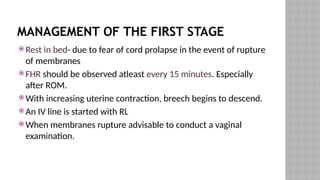
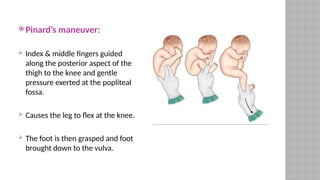
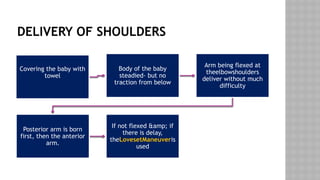
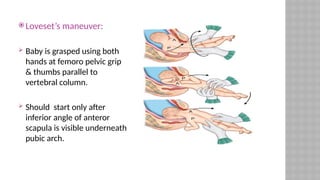
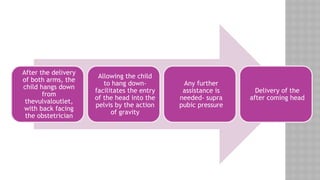
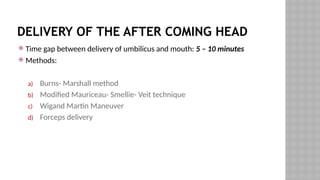
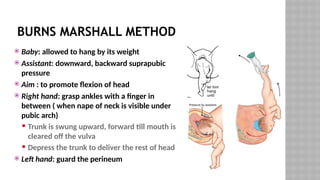
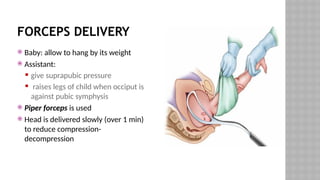
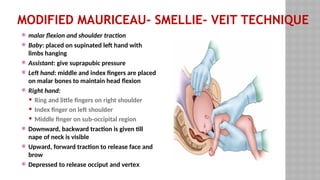
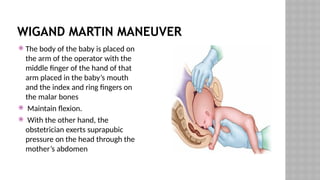
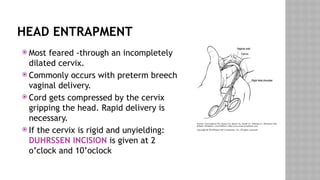
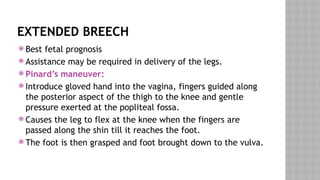
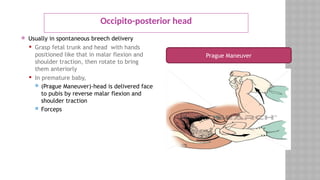
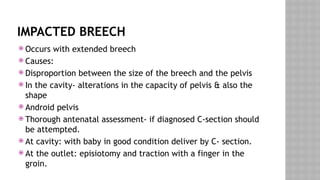
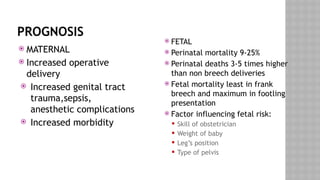
The document provides an extensive overview of breech presentation in fetal delivery, including definitions, types, prevalence, causes, diagnosis, and management strategies. It emphasizes the risks associated with breech births, such as higher perinatal mortality and complications during labor, while detailing prevention methods like external cephalic version (ECV) and indications for cesarean deliveries. Lastly, the document discusses clinical maneuvers for managing breech deliveries and potential complications during the process.