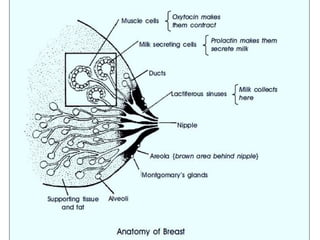
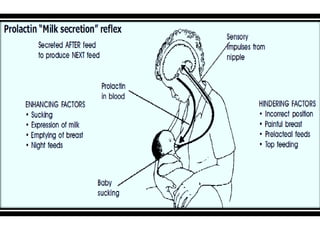
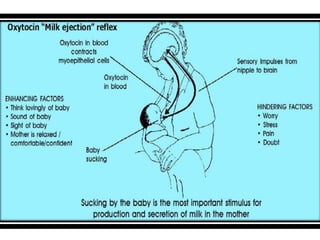
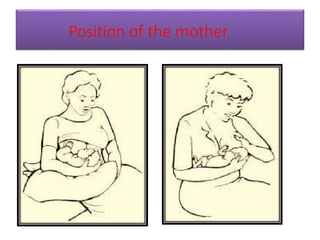
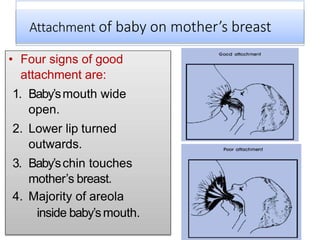
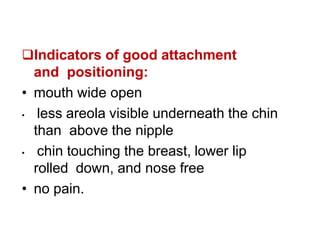
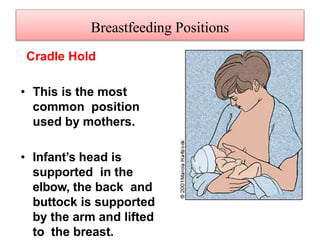
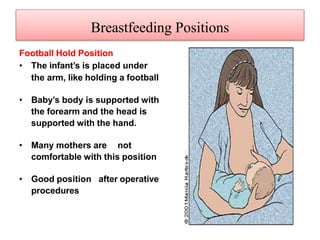
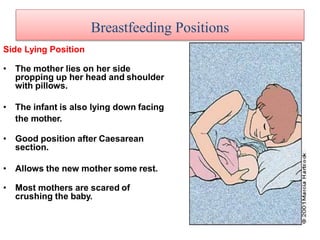
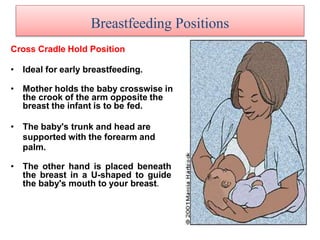
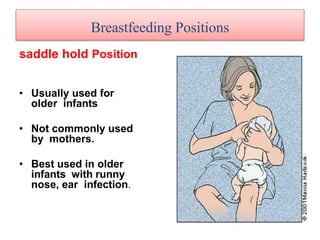
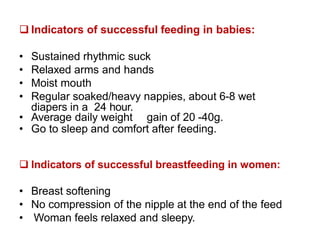
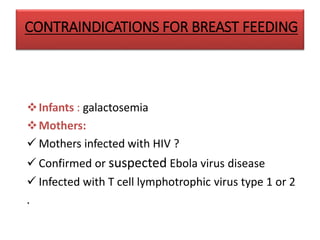
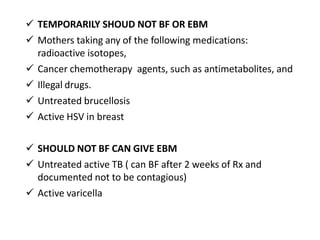
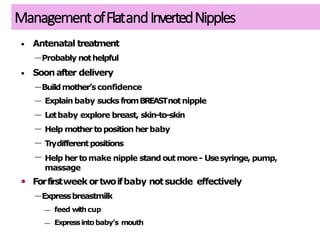
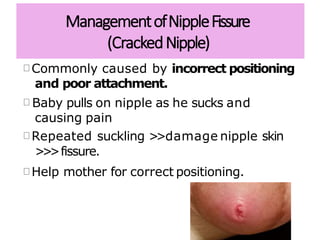
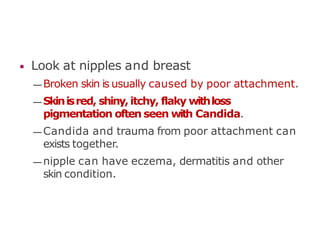
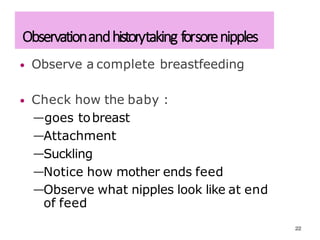
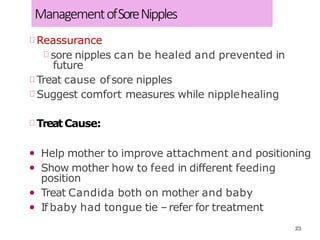
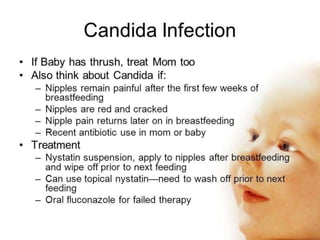
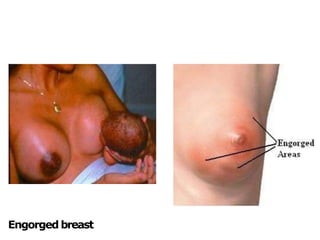
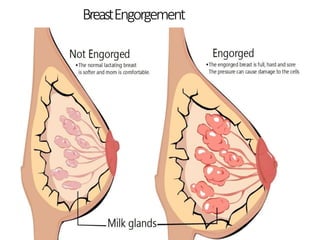
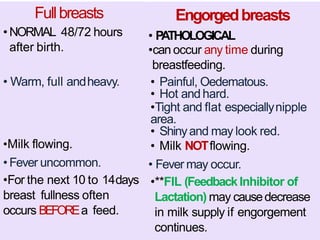
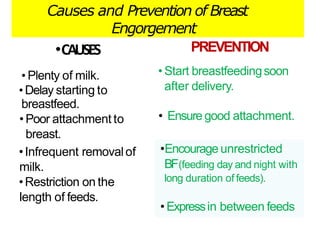
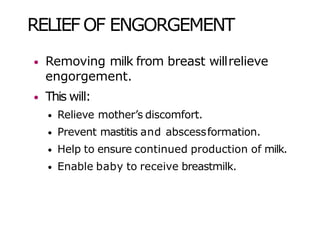
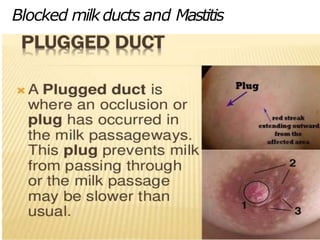
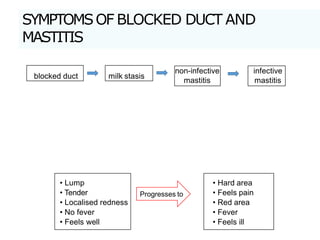
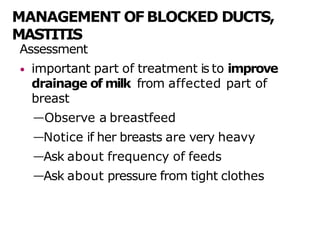
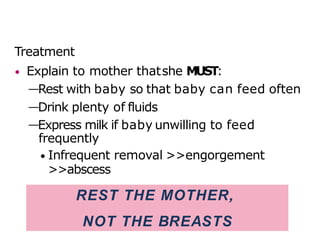
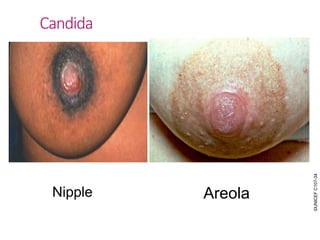
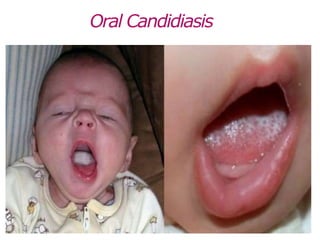
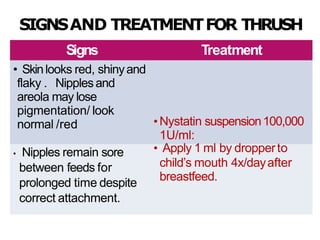
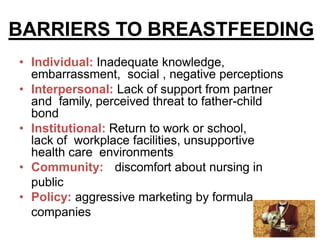
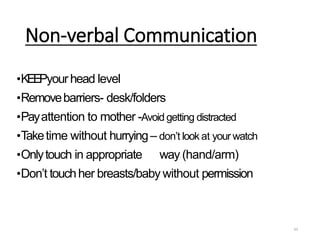
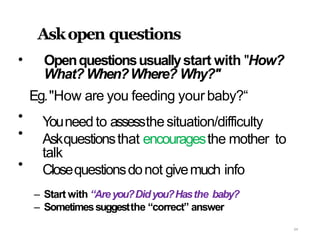
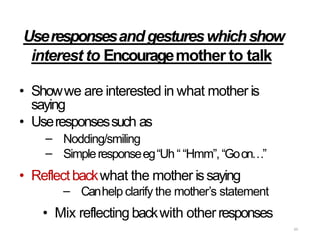
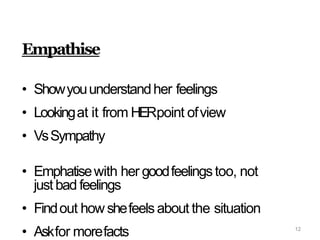
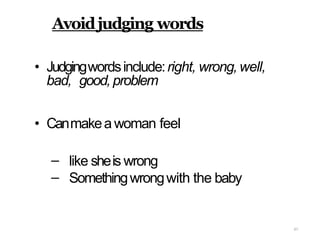
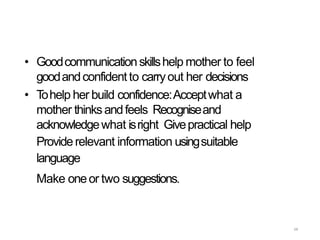
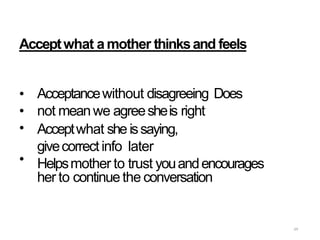
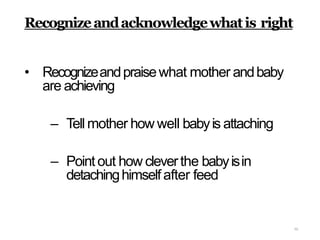
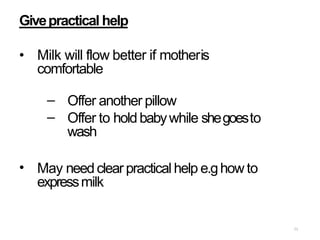
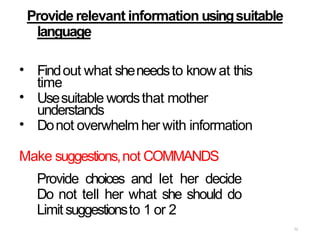
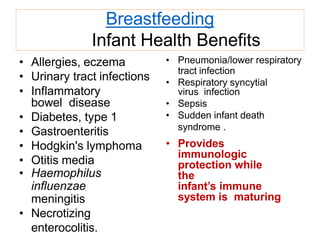
This document provides information on breastfeeding. It discusses the importance of breastfeeding for infant health and development. It covers breast anatomy and milk production. It also describes different breastfeeding positions and signs of successful attachment and feeding. The document discusses common breast conditions like engorgement, blocked ducts, mastitis and thrush. It provides guidance on managing these conditions and preventing nipple soreness. The document emphasizes the importance of counseling to support breastfeeding mothers.