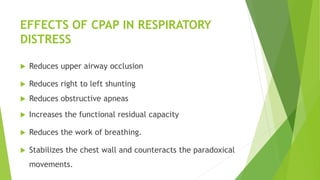
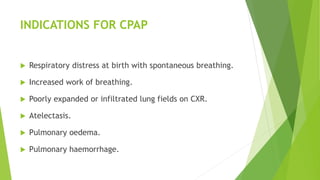
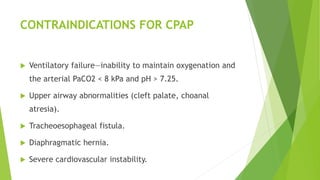
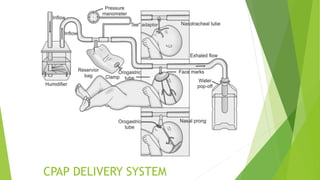
CPAP is a method of providing positive airway pressure throughout the respiratory cycle to prevent airway collapse in infants with respiratory distress. It works by distending the alveoli to reduce work of breathing and improve oxygenation. CPAP is indicated for respiratory distress at birth or with conditions like atelectasis or pulmonary edema. It is contraindicated in cases of ventilatory failure or major airway abnormalities. CPAP systems use continuous gas flow through an interface, like nasal prongs, to maintain positive pressure. Infants on CPAP require monitoring and weaning should be based on clinical criteria like stable oxygen saturations without distress.