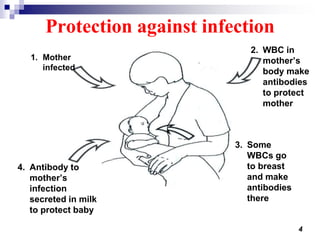
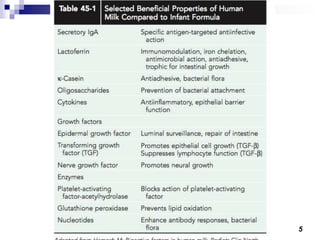
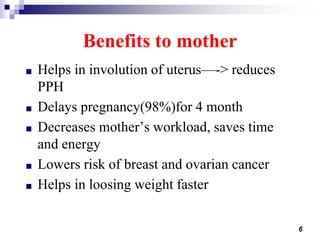
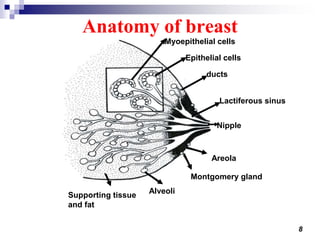
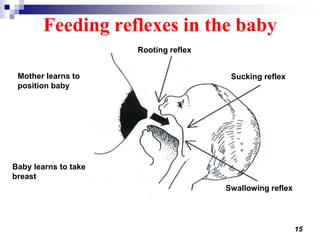
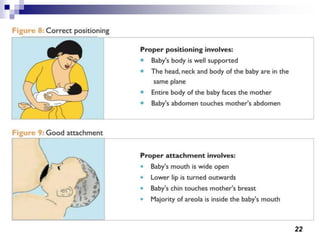
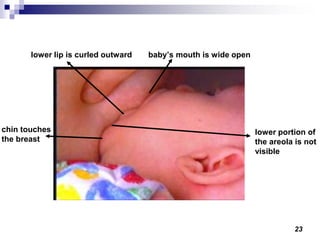
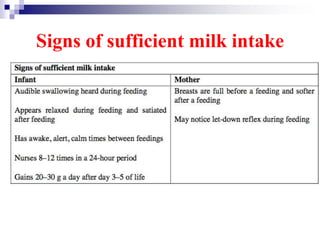
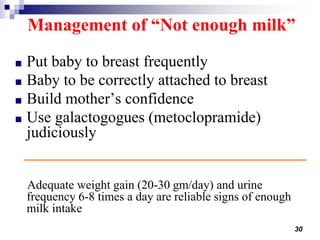
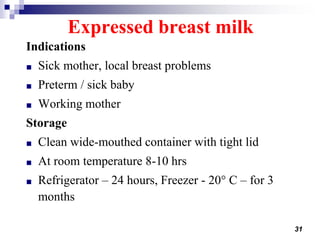
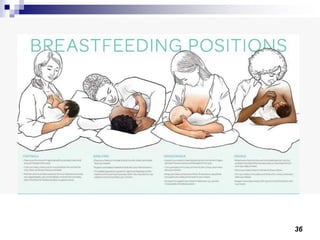
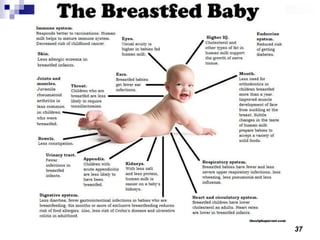
Breastfeeding provides significant benefits to both babies and mothers. For babies, breast milk contains essential nutrients for growth and development, protects against infection through antibodies and immune factors, and promotes emotional bonding. Benefits to mothers include reduced risk of ovarian and breast cancer, faster weight loss after birth, and delayed return of fertility. Successful breastfeeding requires a motivated mother, an active baby with proper sucking reflexes, and support from health professionals to ensure correct positioning and frequent feeding. Expressing and storing breast milk allows mothers to continue providing breast milk when separated from their babies.