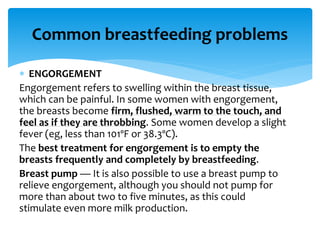
Breastfeeding is highly beneficial for both the baby and the mother, promoting immunity, reducing health risks, and facilitating emotional bonding. Proper techniques and frequent nursing sessions are emphasized, with recommendations for addressing common challenges like engorgement and sore nipples. Continued breastfeeding alongside solid food can further enhance the child's immune system and support overall health.