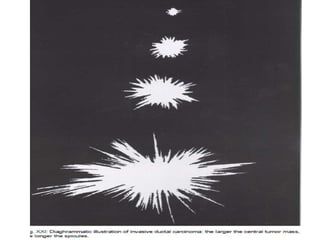
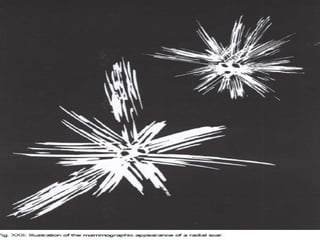
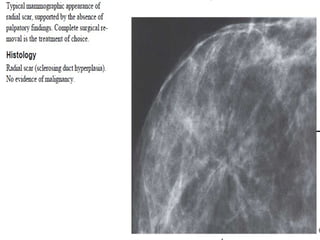
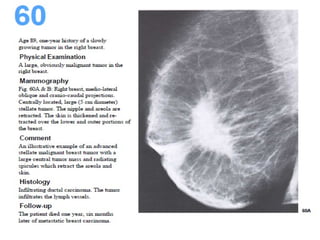
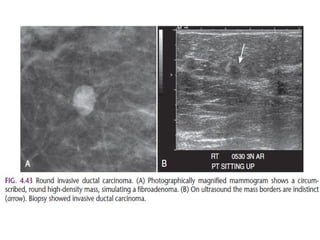
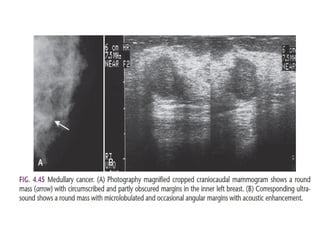
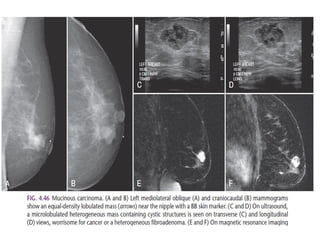
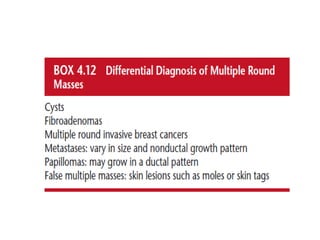
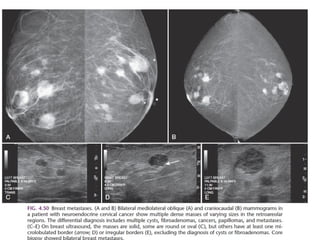
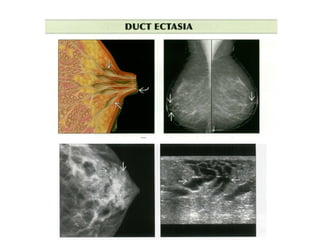
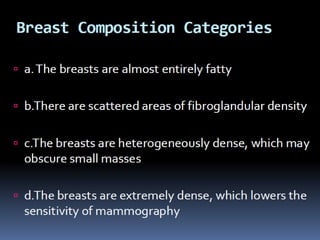
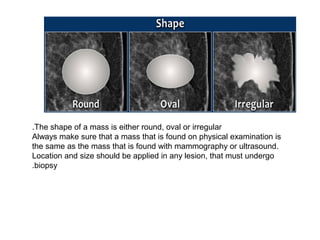
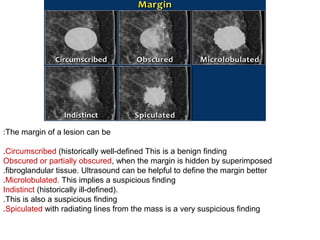
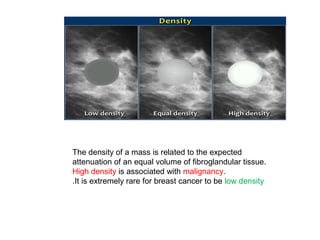
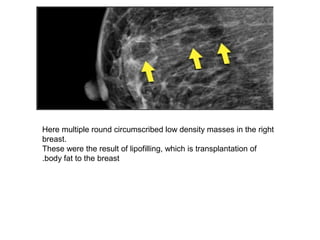
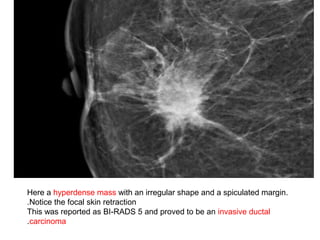
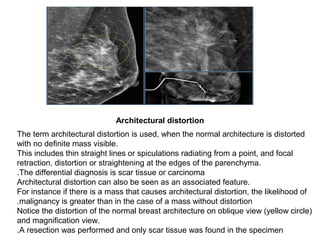
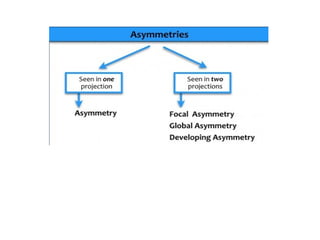
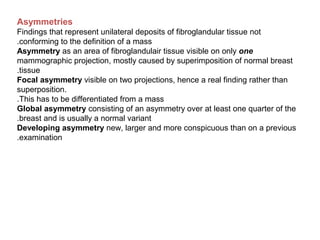
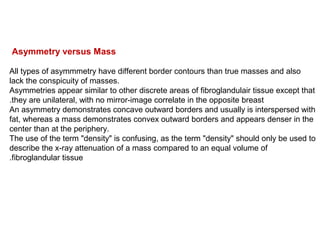
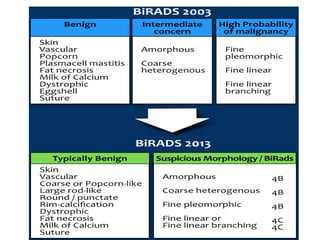
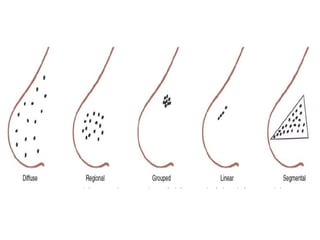
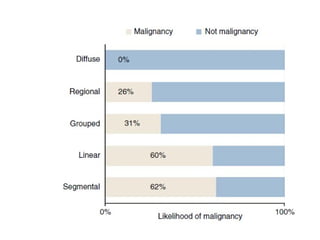
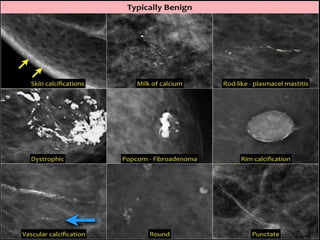
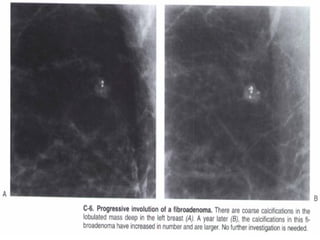
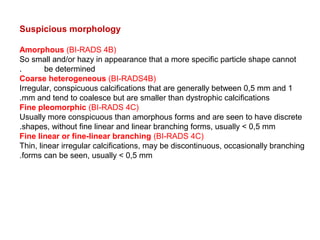
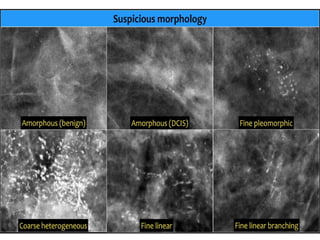
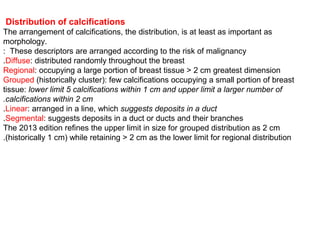
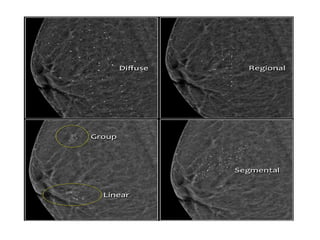
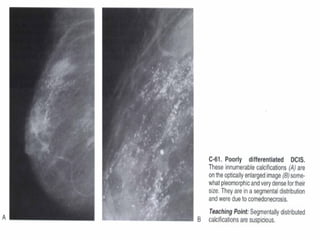
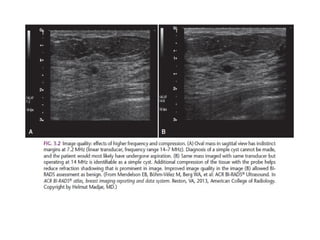
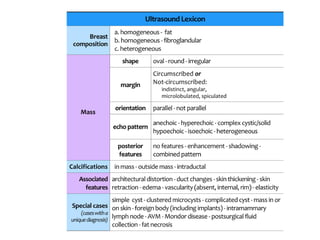
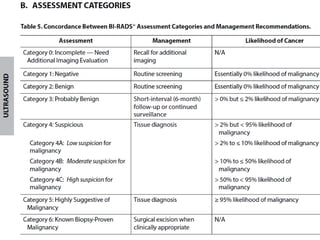
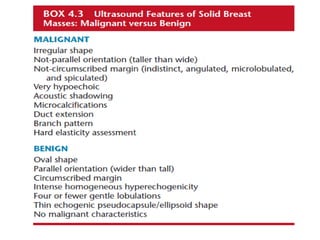
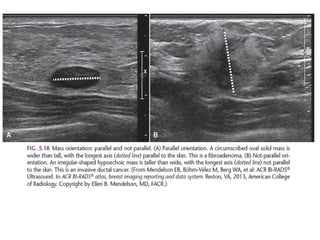
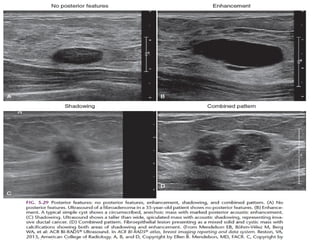
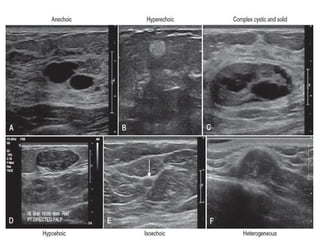
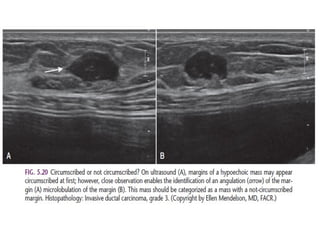
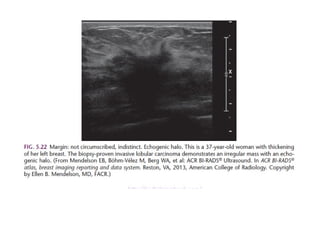
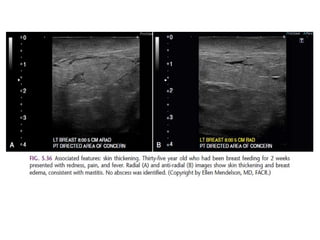
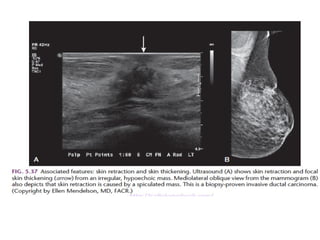
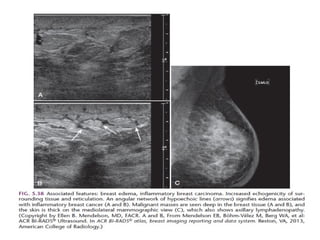
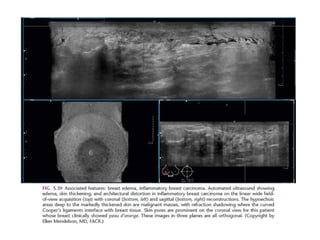
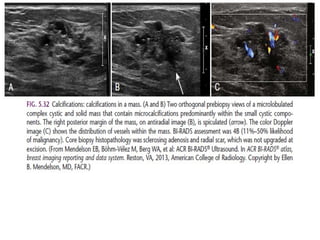
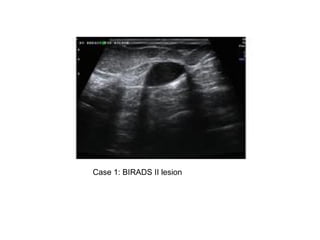
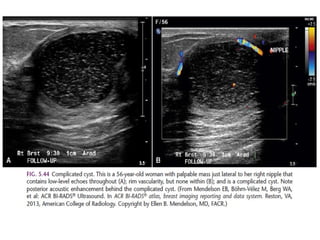
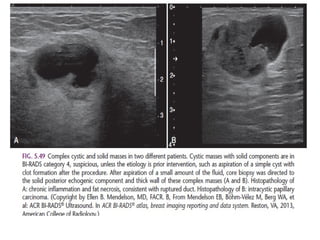
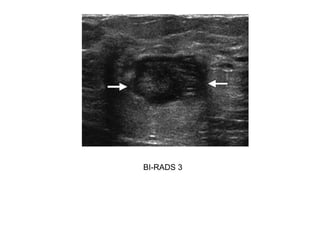
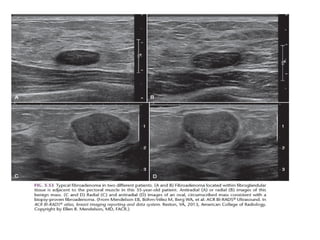
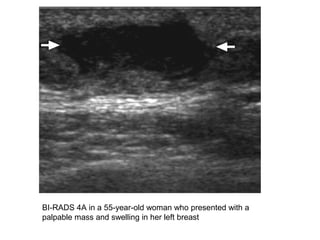
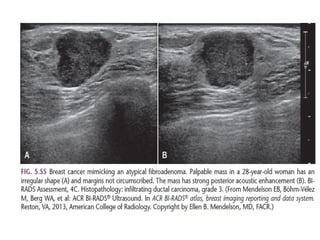
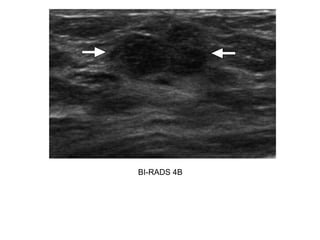
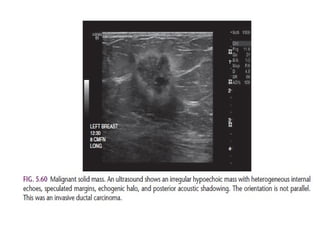
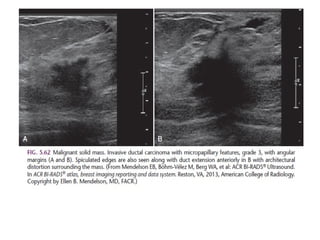
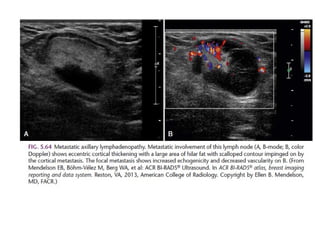
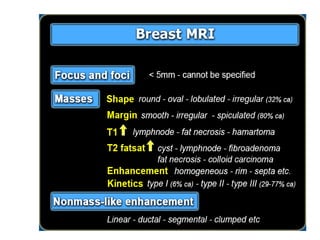
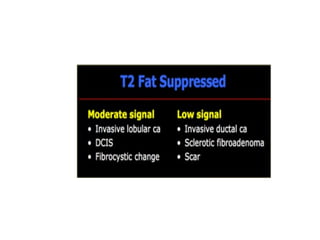
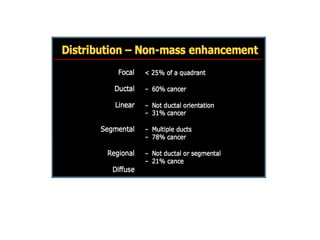
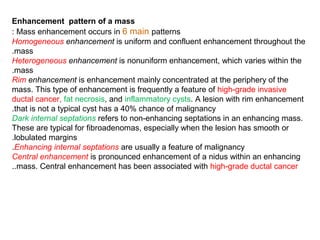
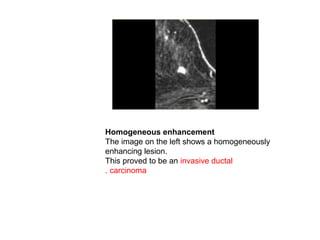
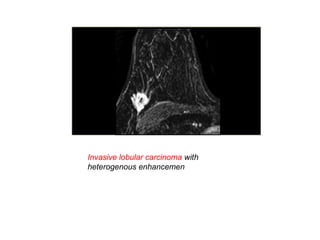
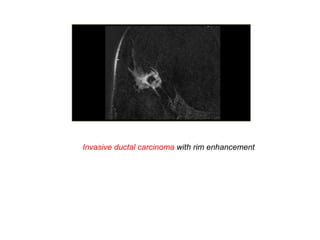
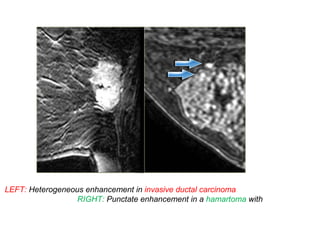
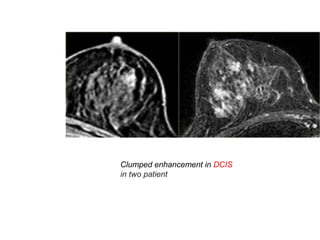
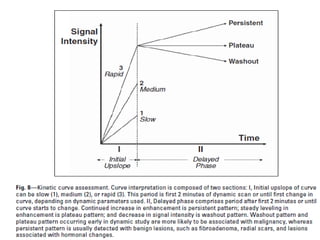
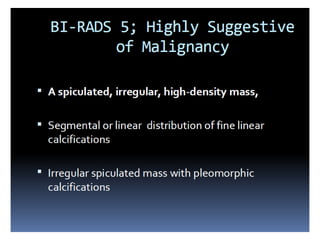
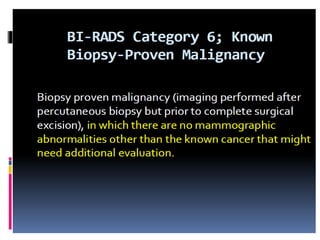
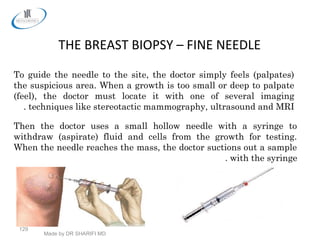
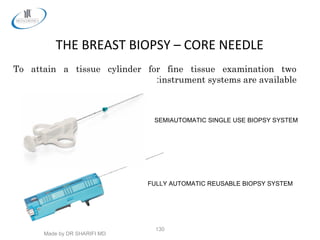
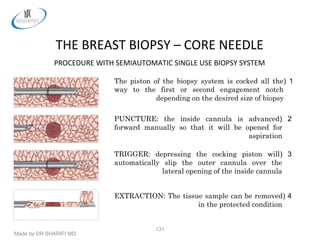
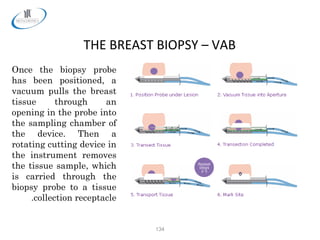
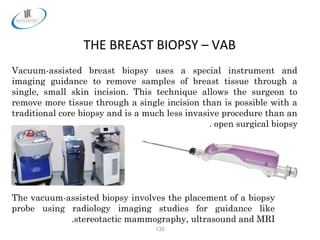
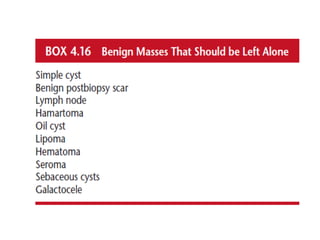
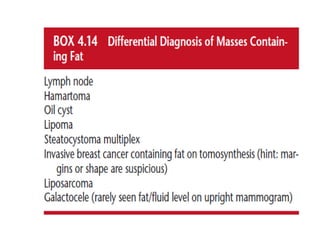
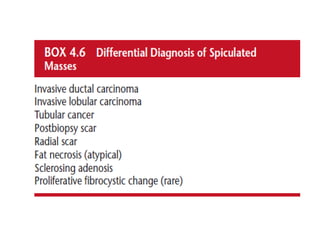
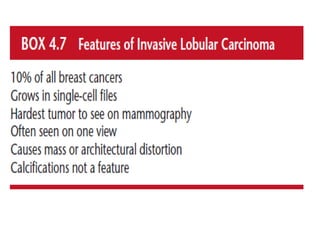
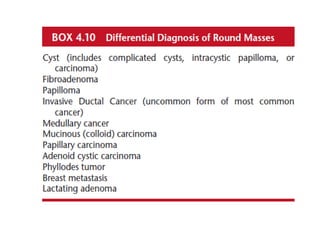
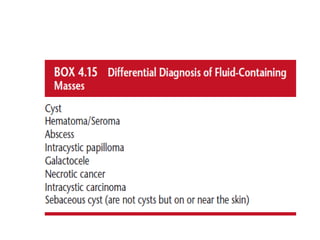
The document provides information about various breast imaging techniques and biopsy procedures. It discusses the appearance of masses and lesions on mammography including characteristics like shape, margin, density, and enhancement patterns. It also describes different types of calcifications and their typical benign or suspicious morphologies. Additionally, the document outlines procedures for fine needle biopsy, core needle biopsy, and vacuum-assisted biopsy. Key details about each technique are given, such as how samples are obtained and analyzed to determine if a growth is benign or malignant.