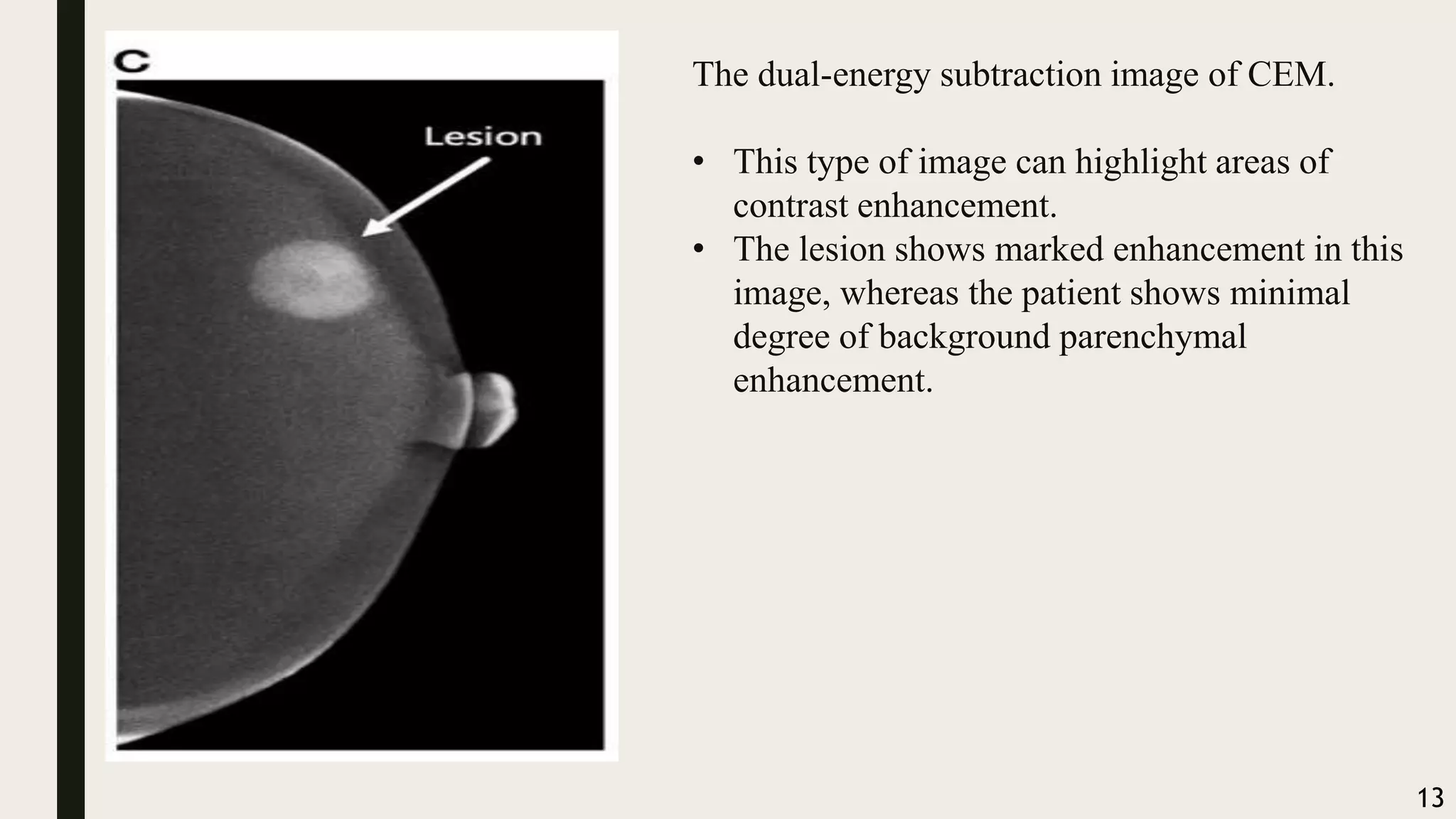
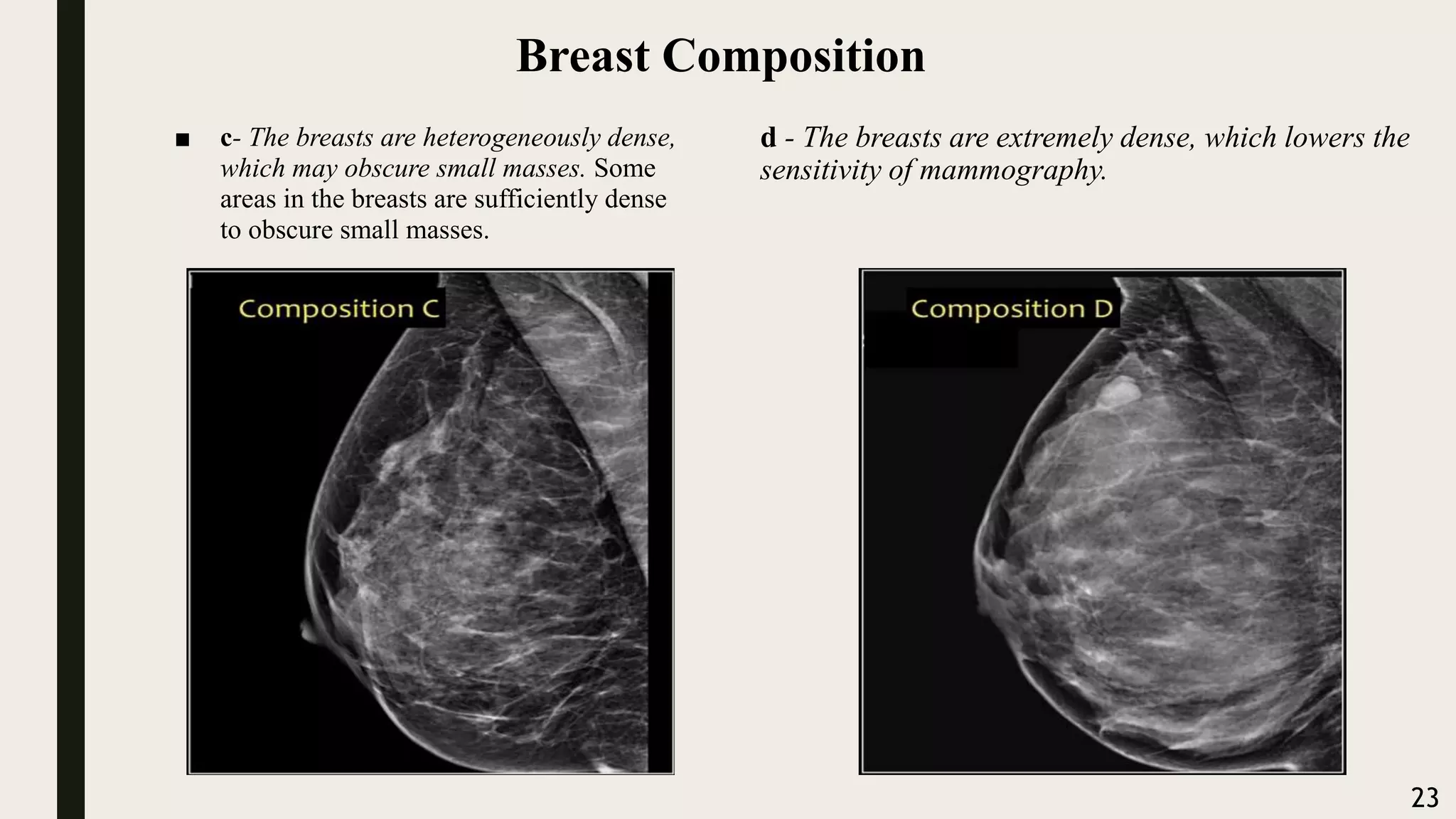
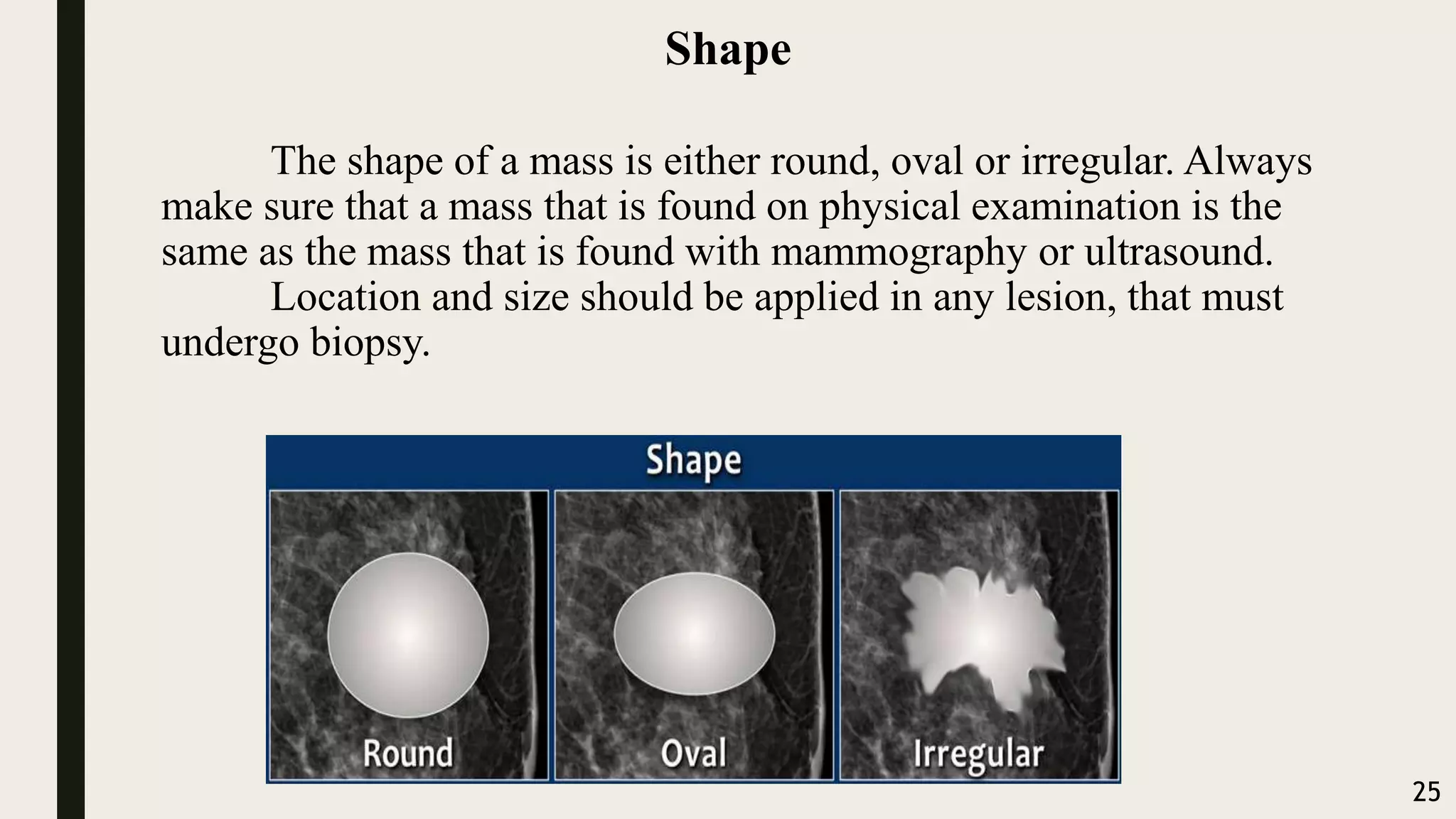
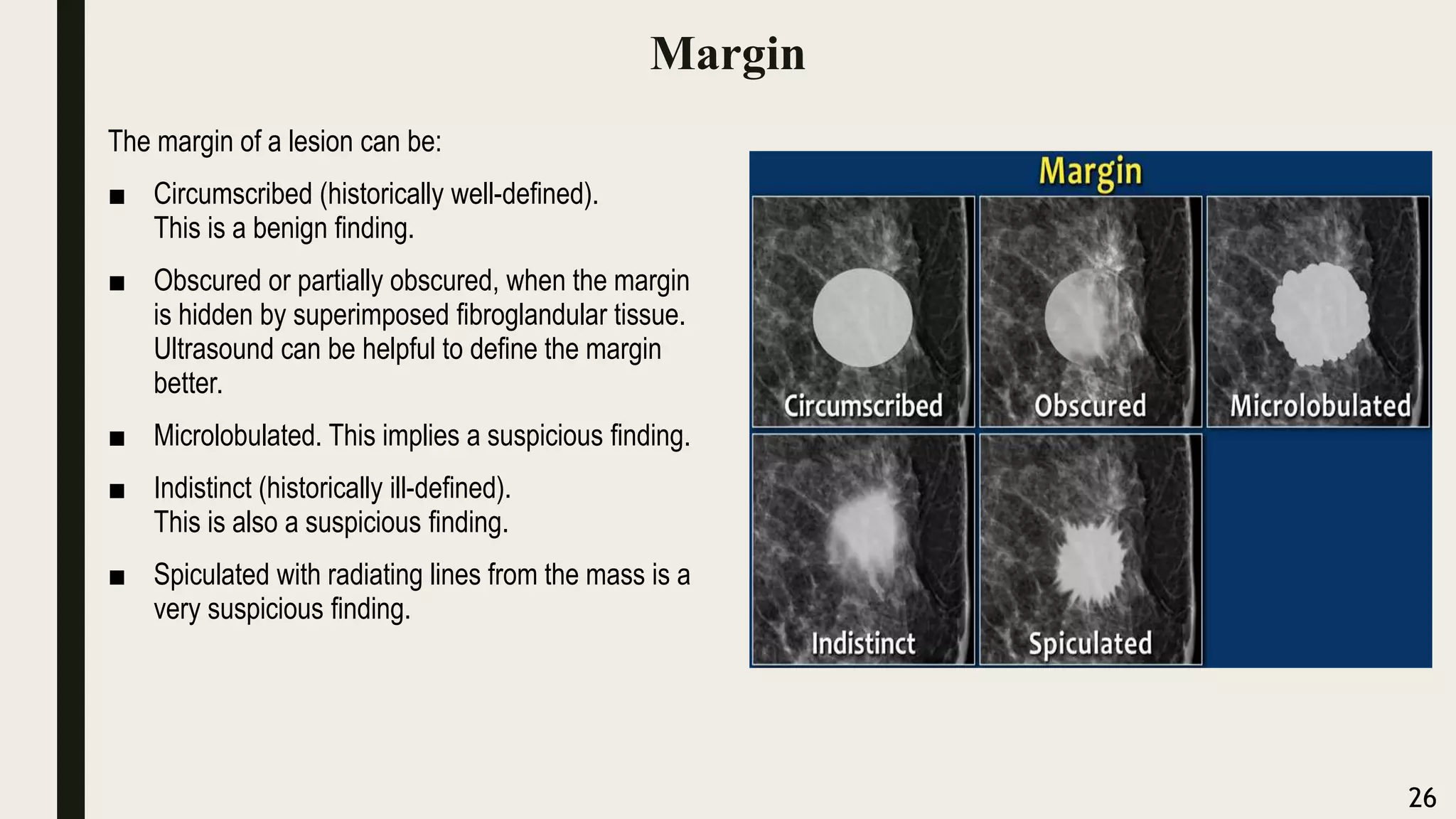
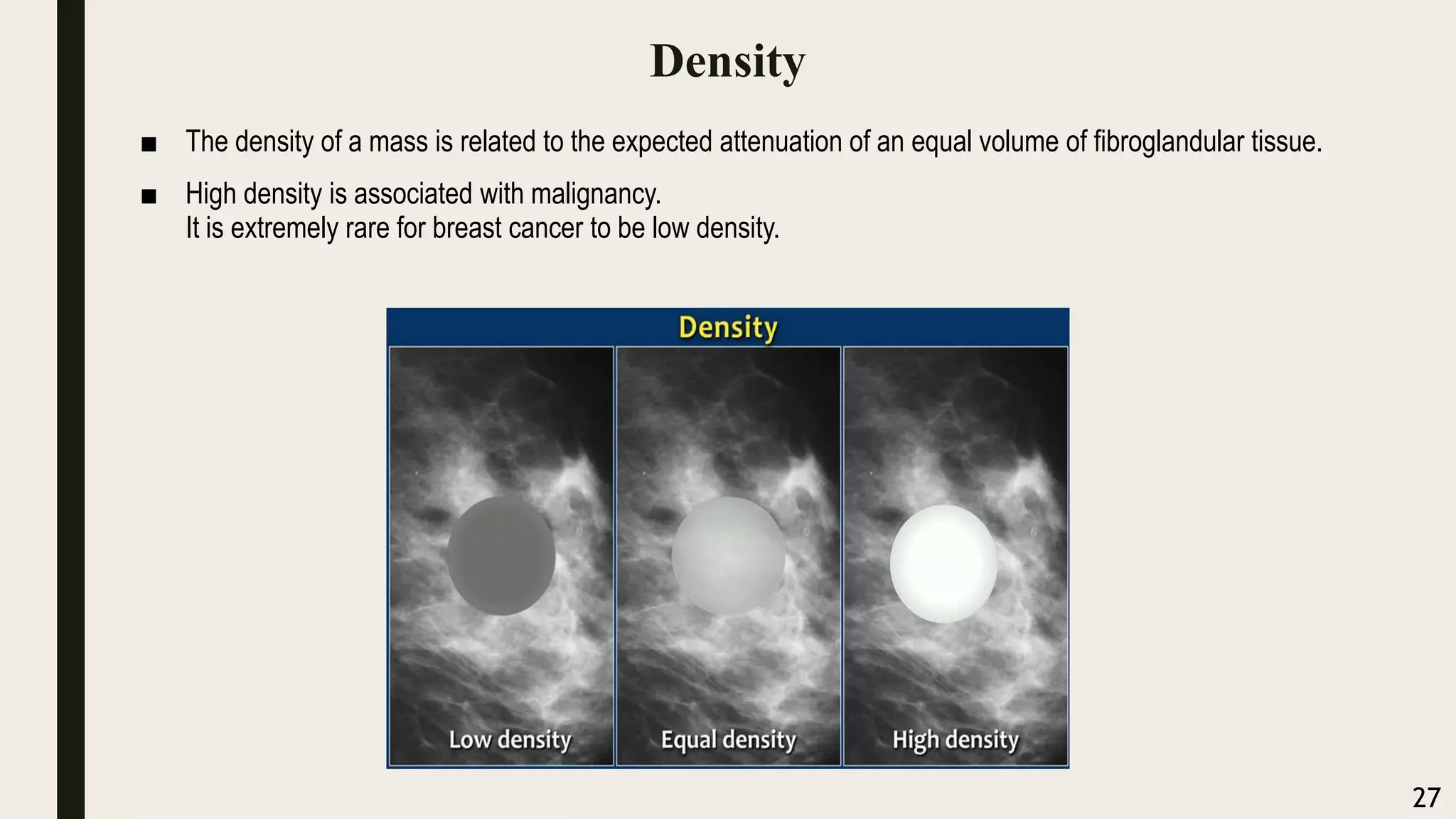
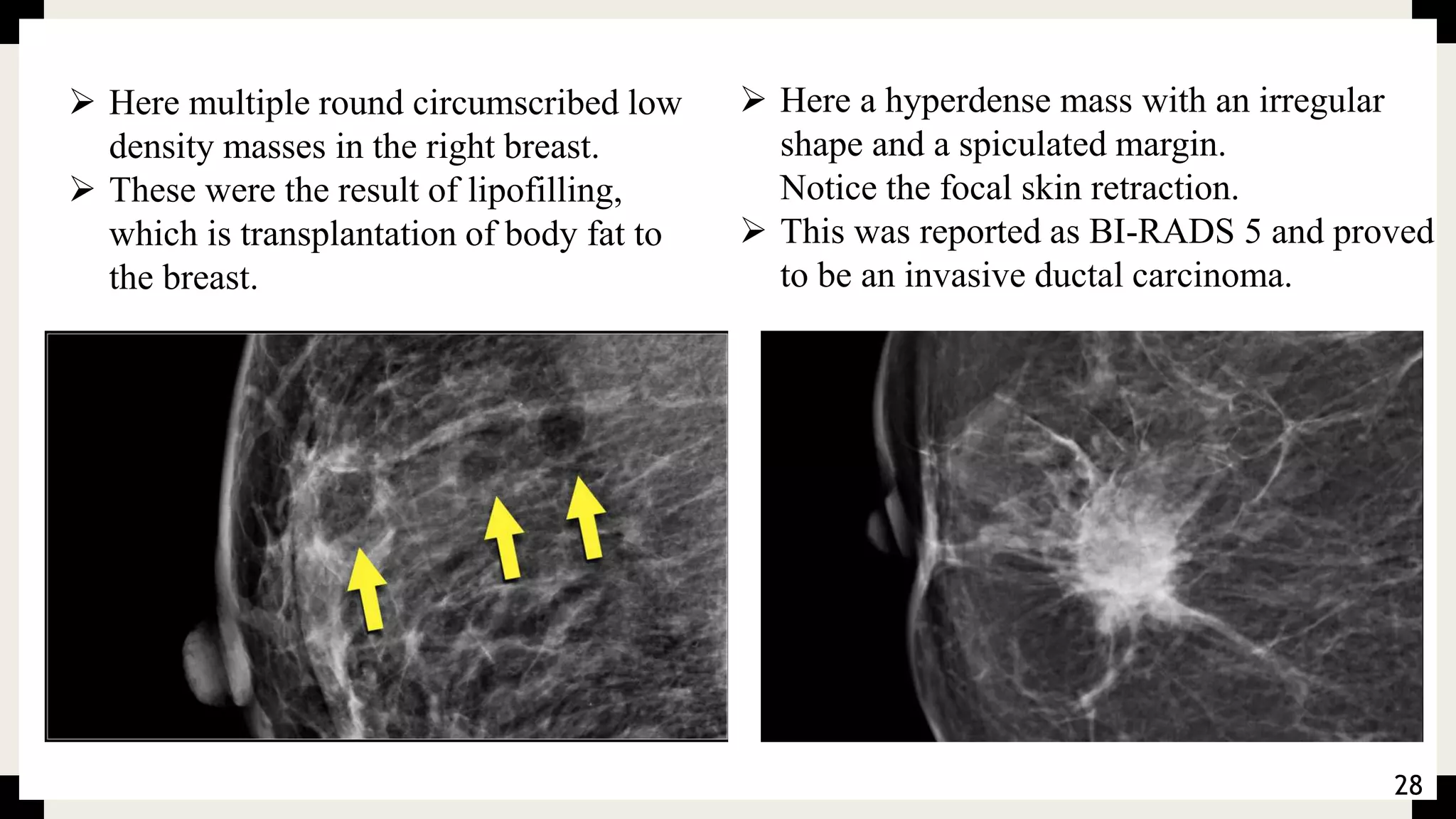
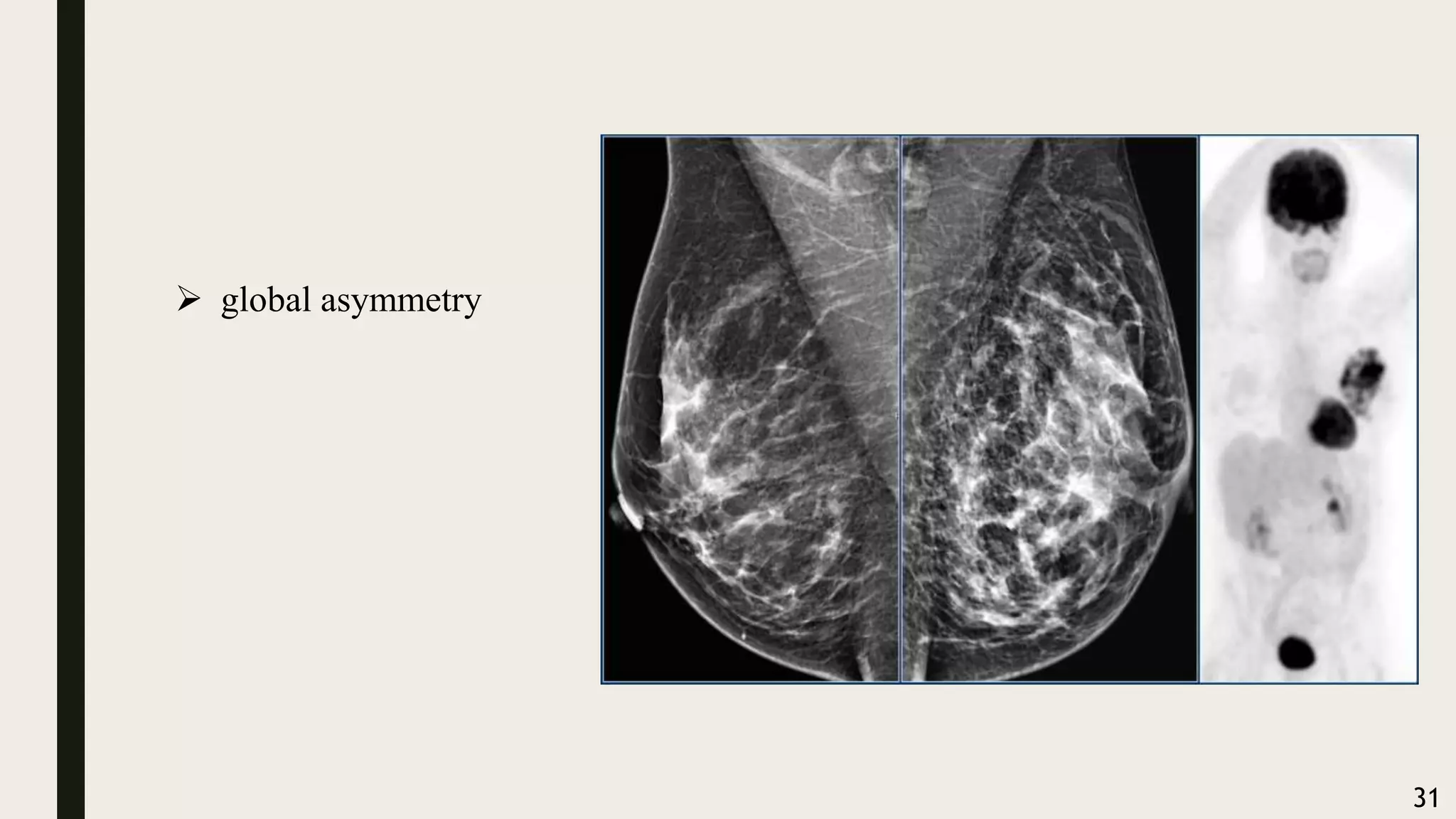
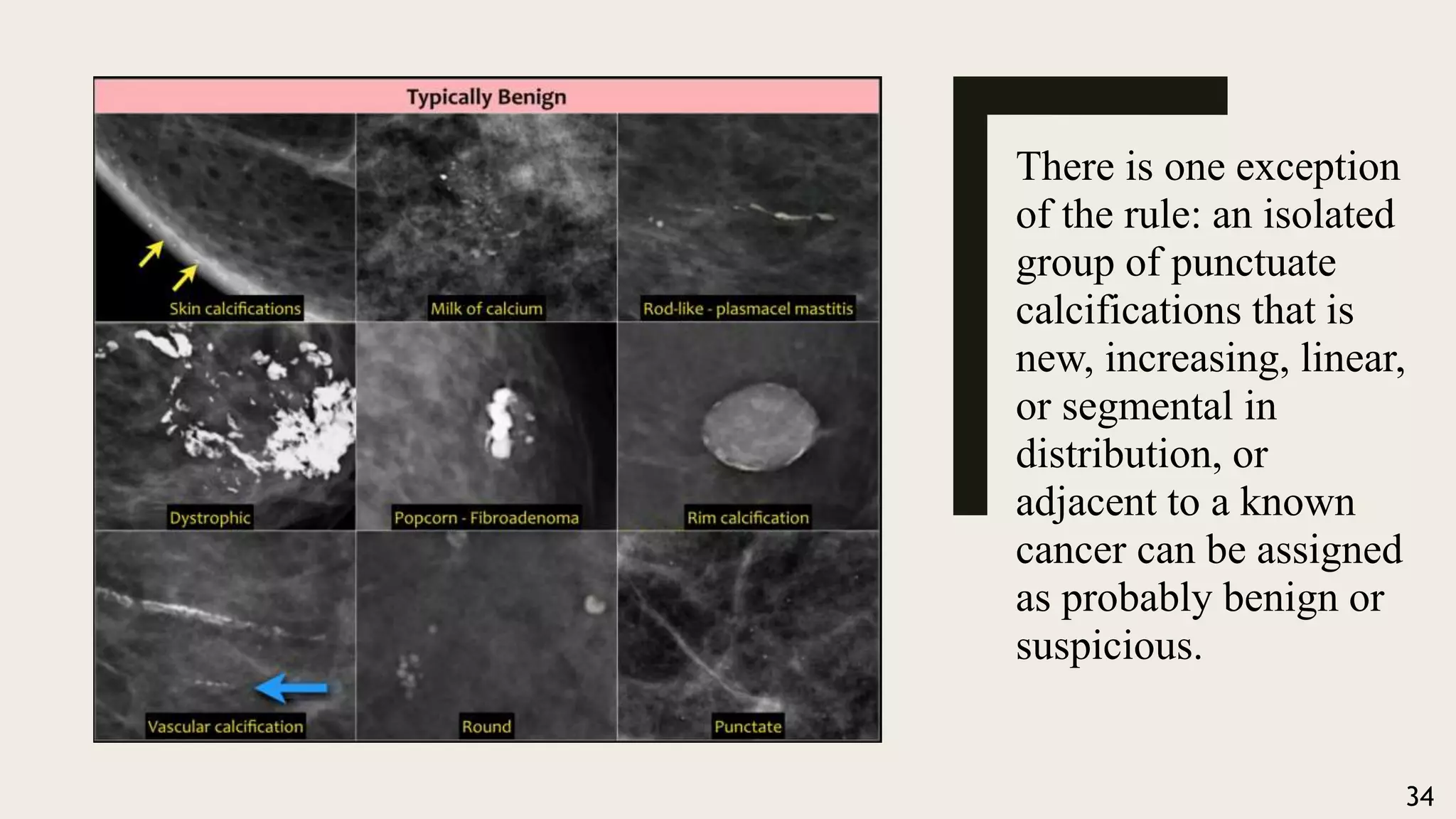
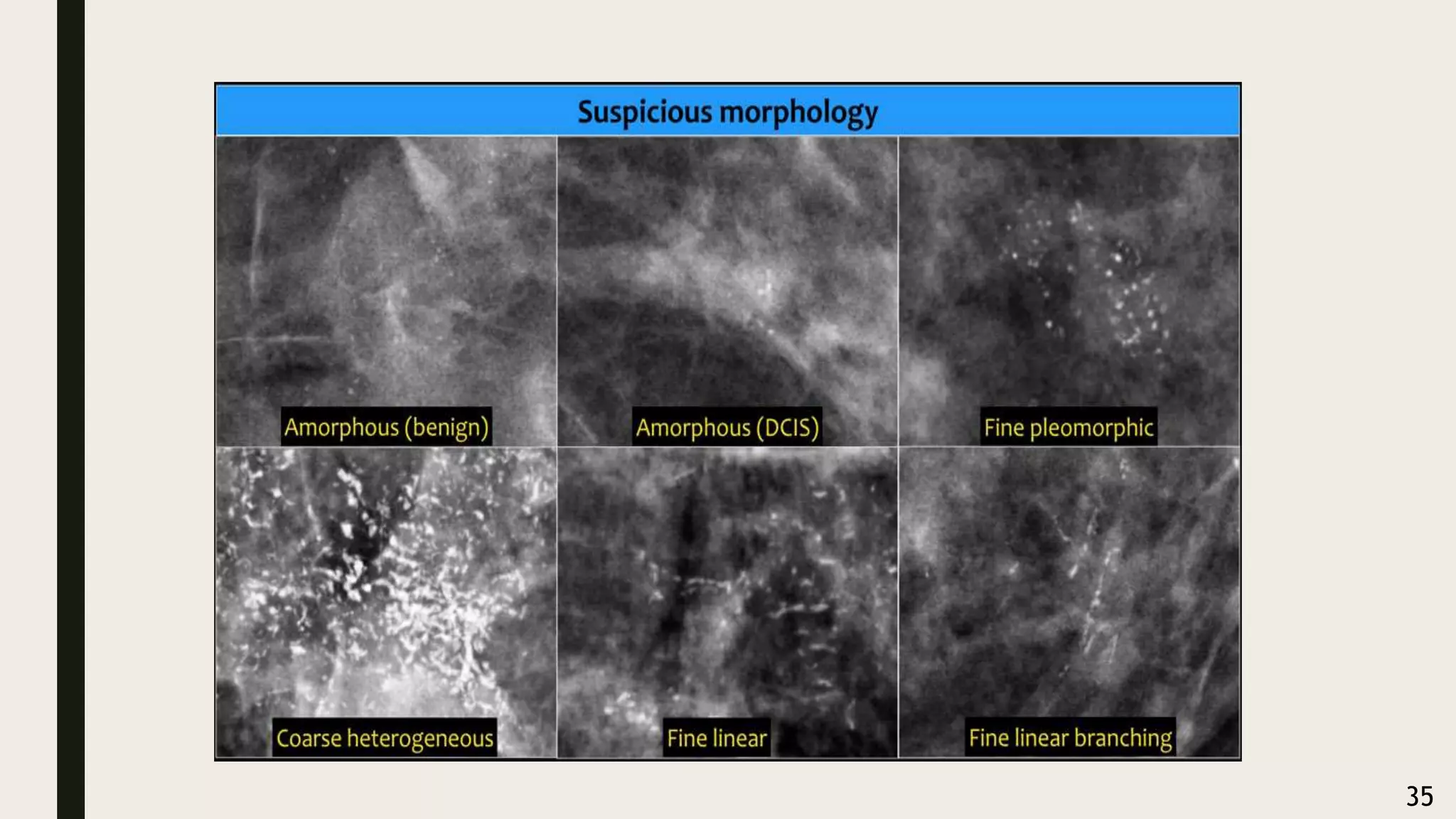
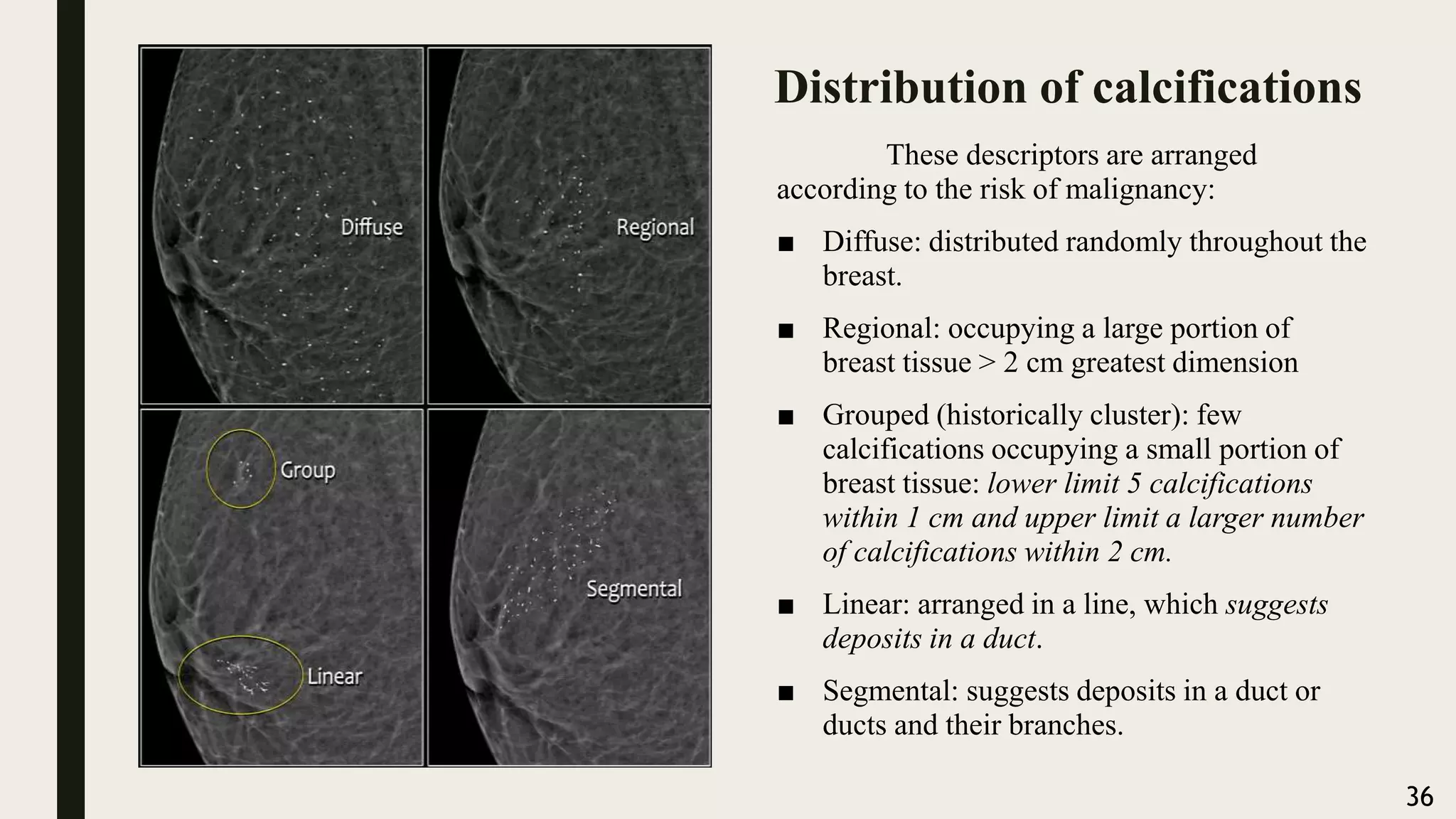
This document provides an overview of mammography, including definitions, indications, equipment, technique, findings, and assessment categories. It defines mammography as an x-ray examination of the breast to detect changes. Key indications include focal signs in women aged 40 or older and screening for high-risk women. Equipment has advanced from film-screen to digital mammography and tomosynthesis. Standard views are mediolateral oblique and craniocaudal. Findings can include masses, asymmetries, distortions, and calcifications, which are categorized based on characteristics like shape, margin, density, and distribution.