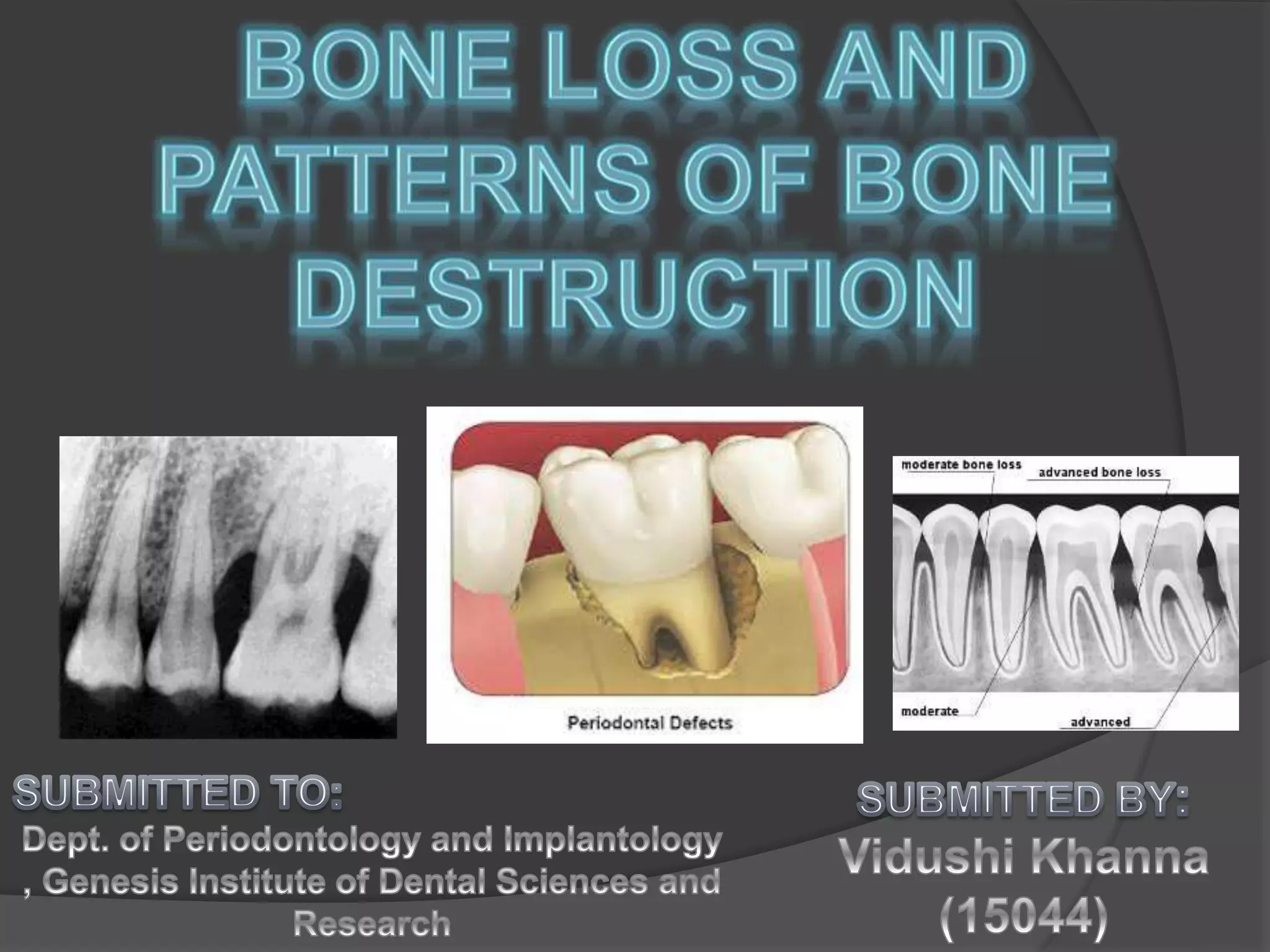
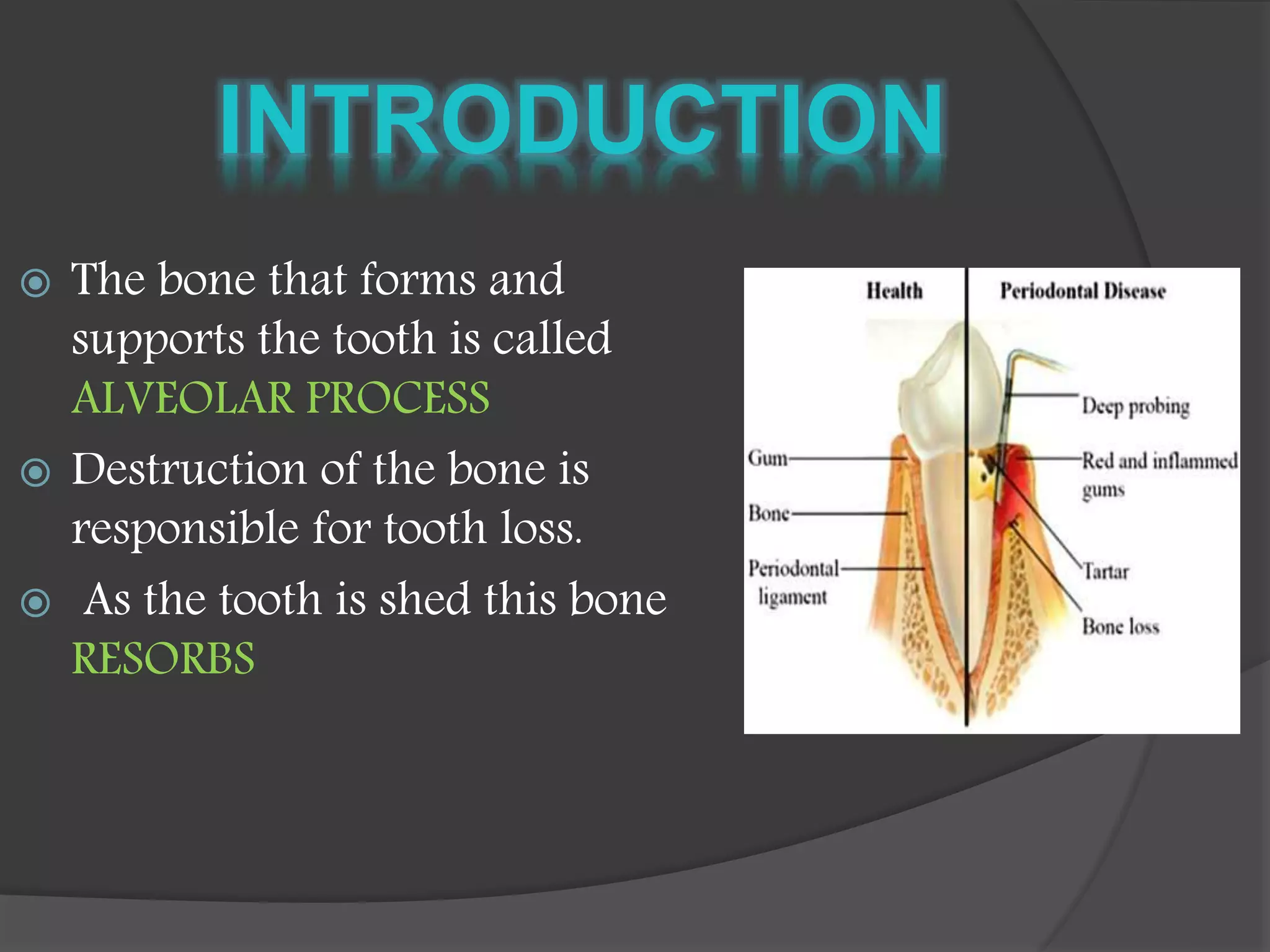
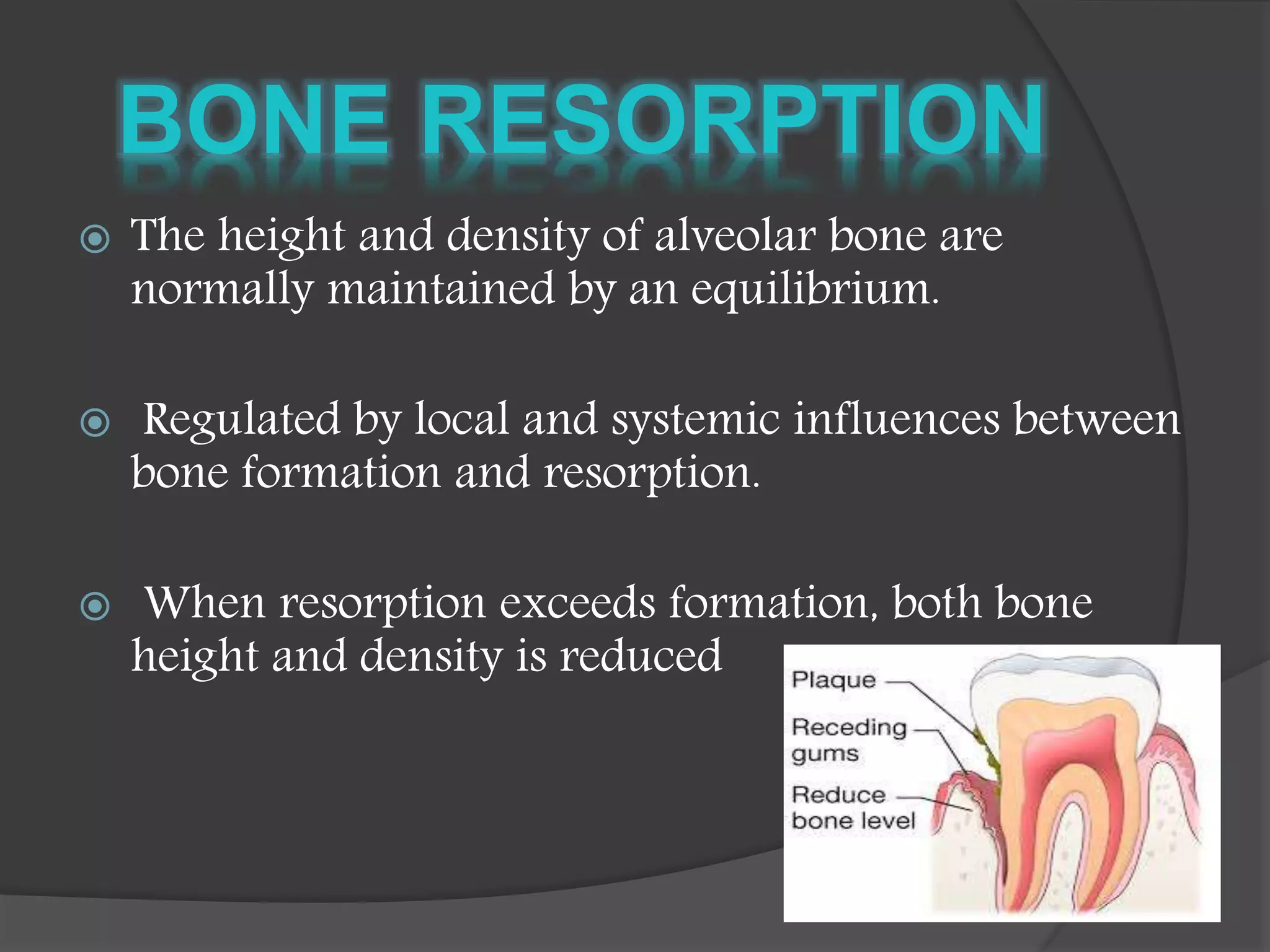
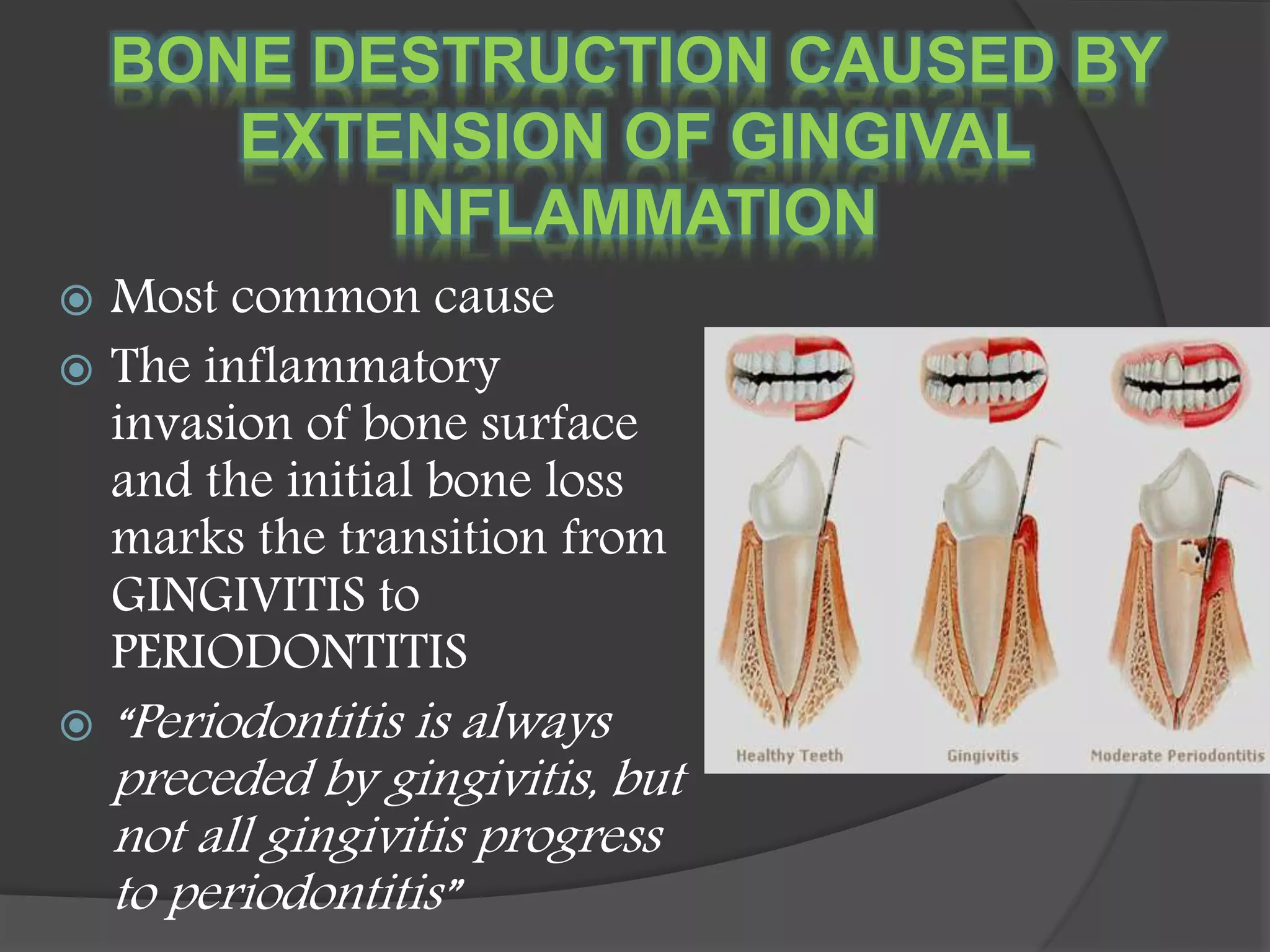
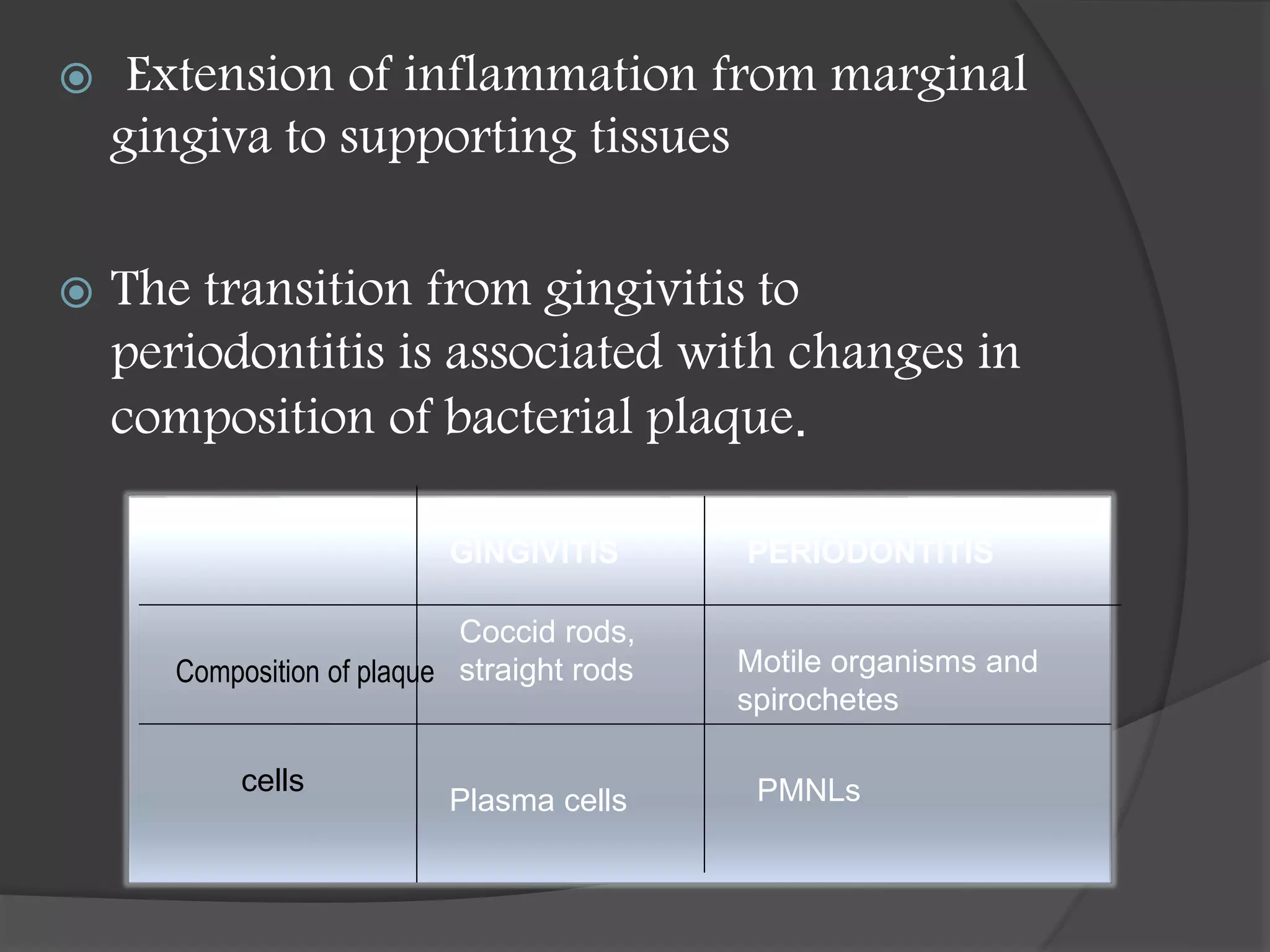
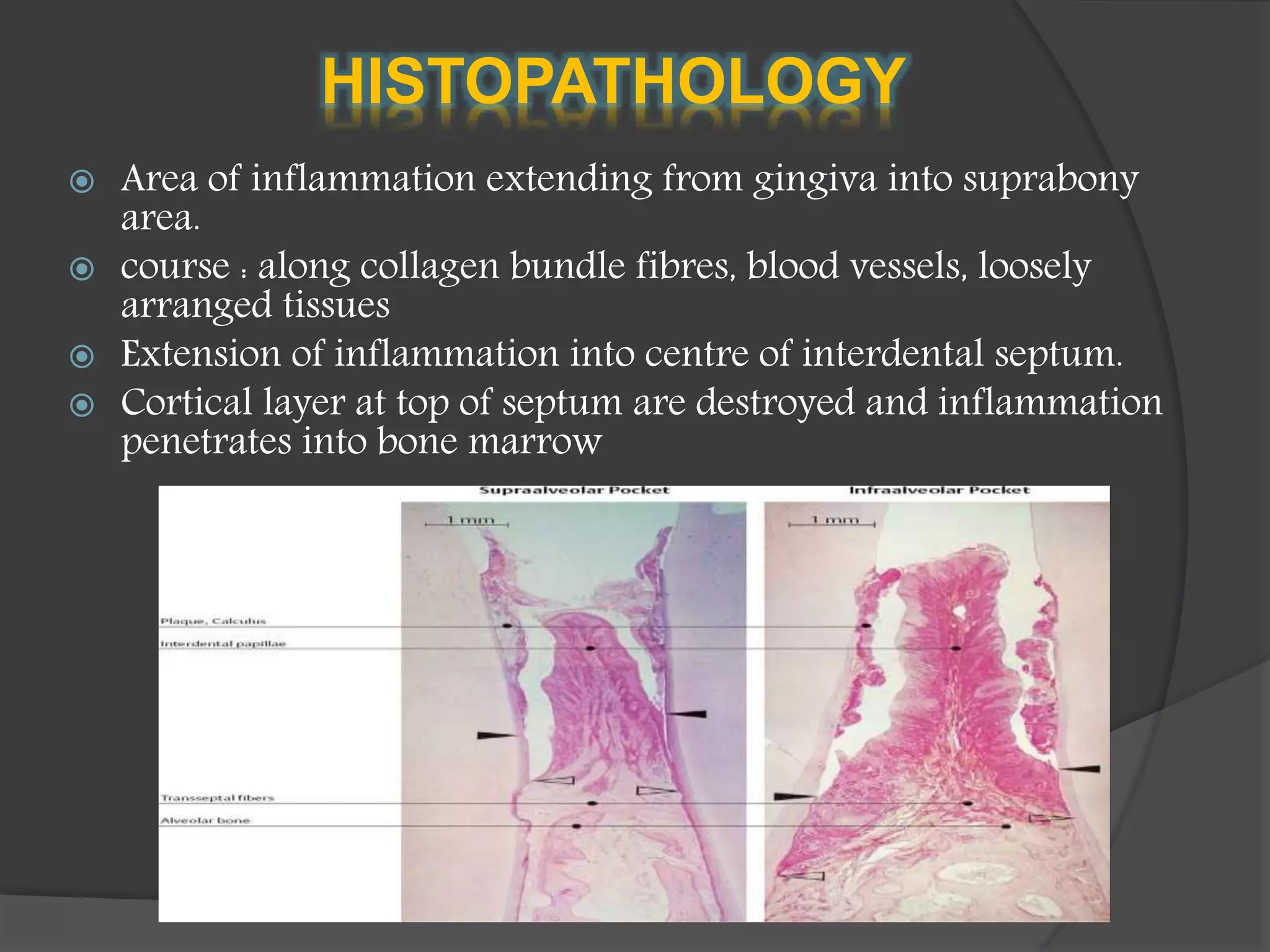
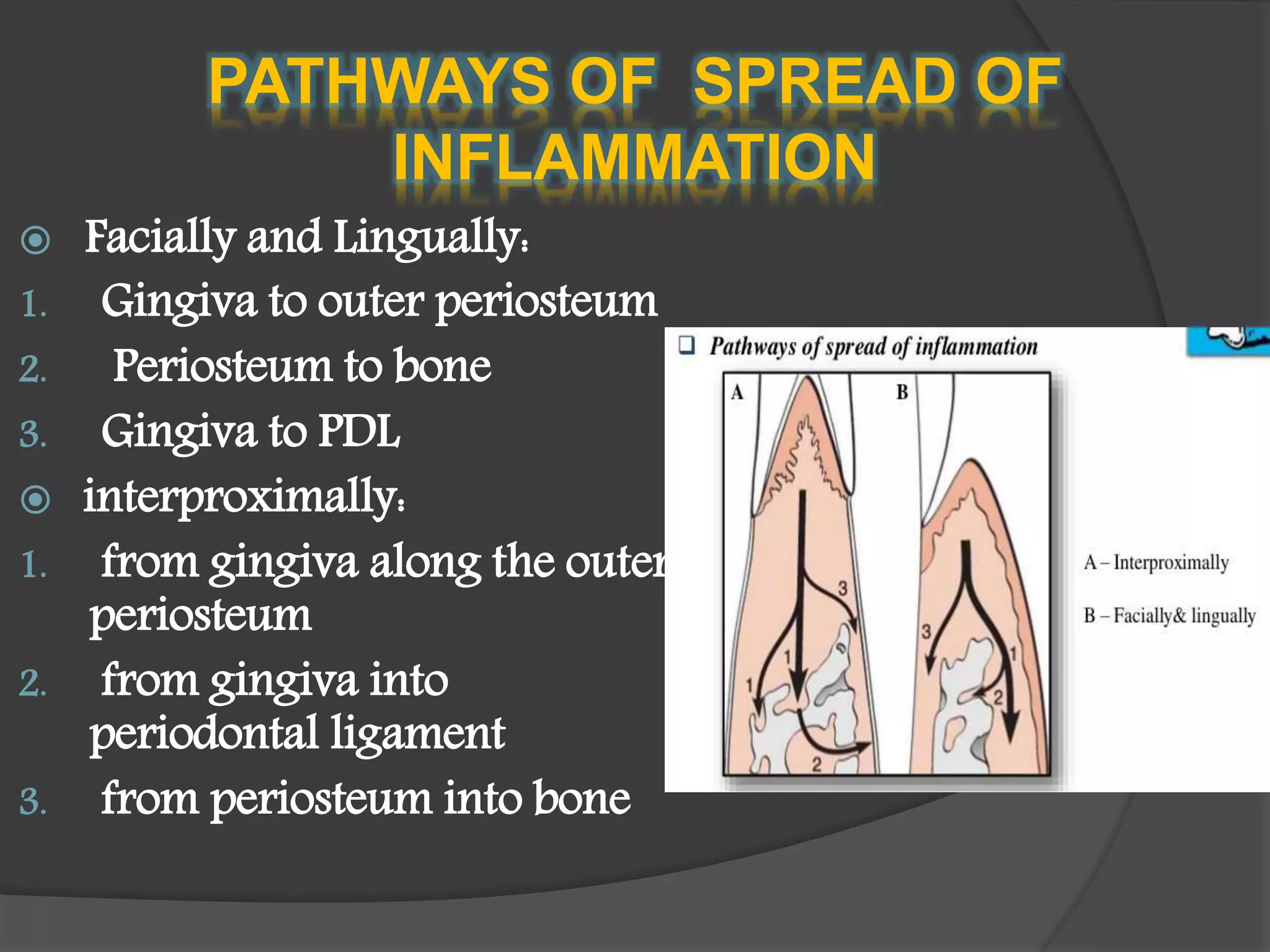
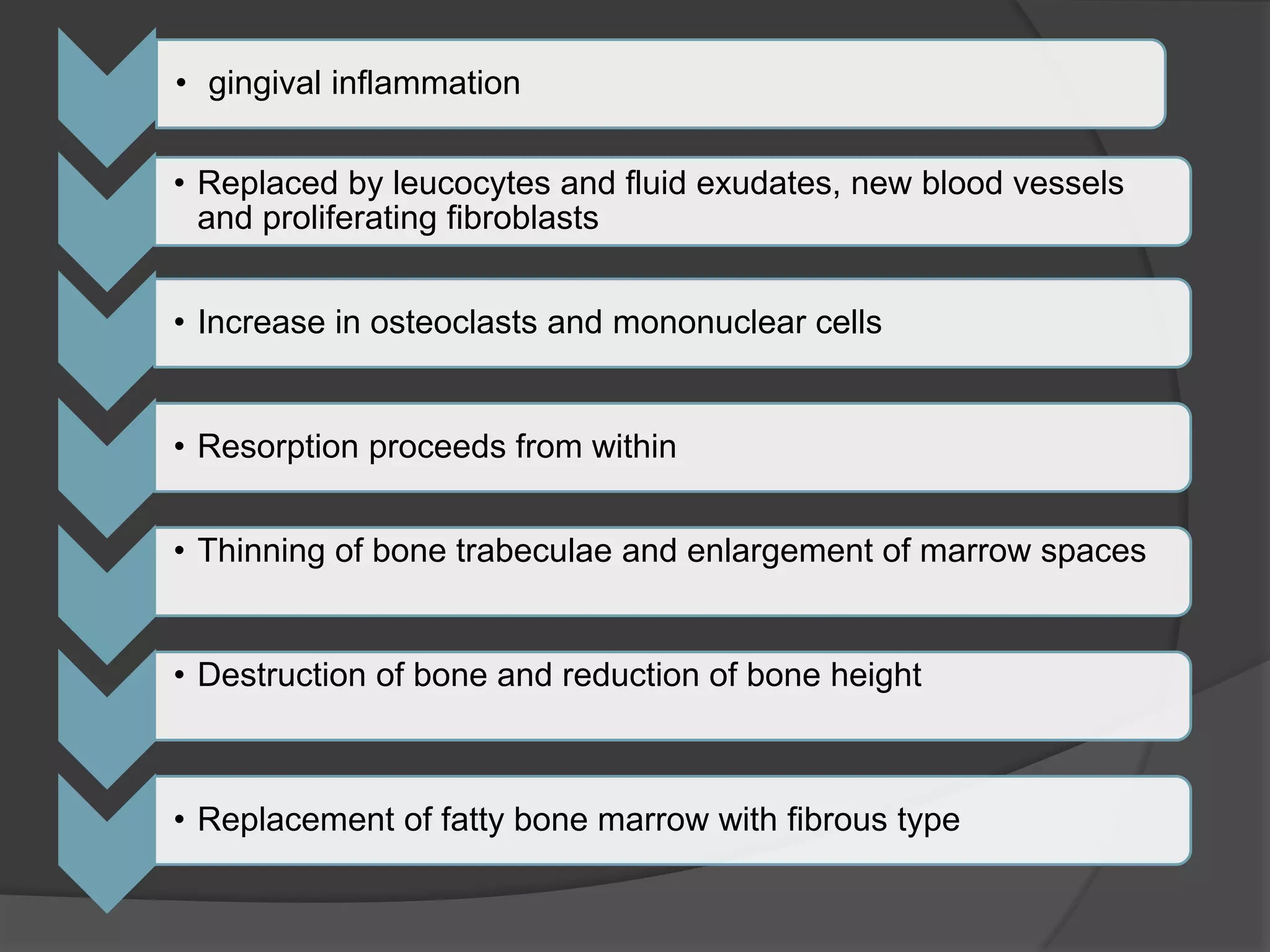
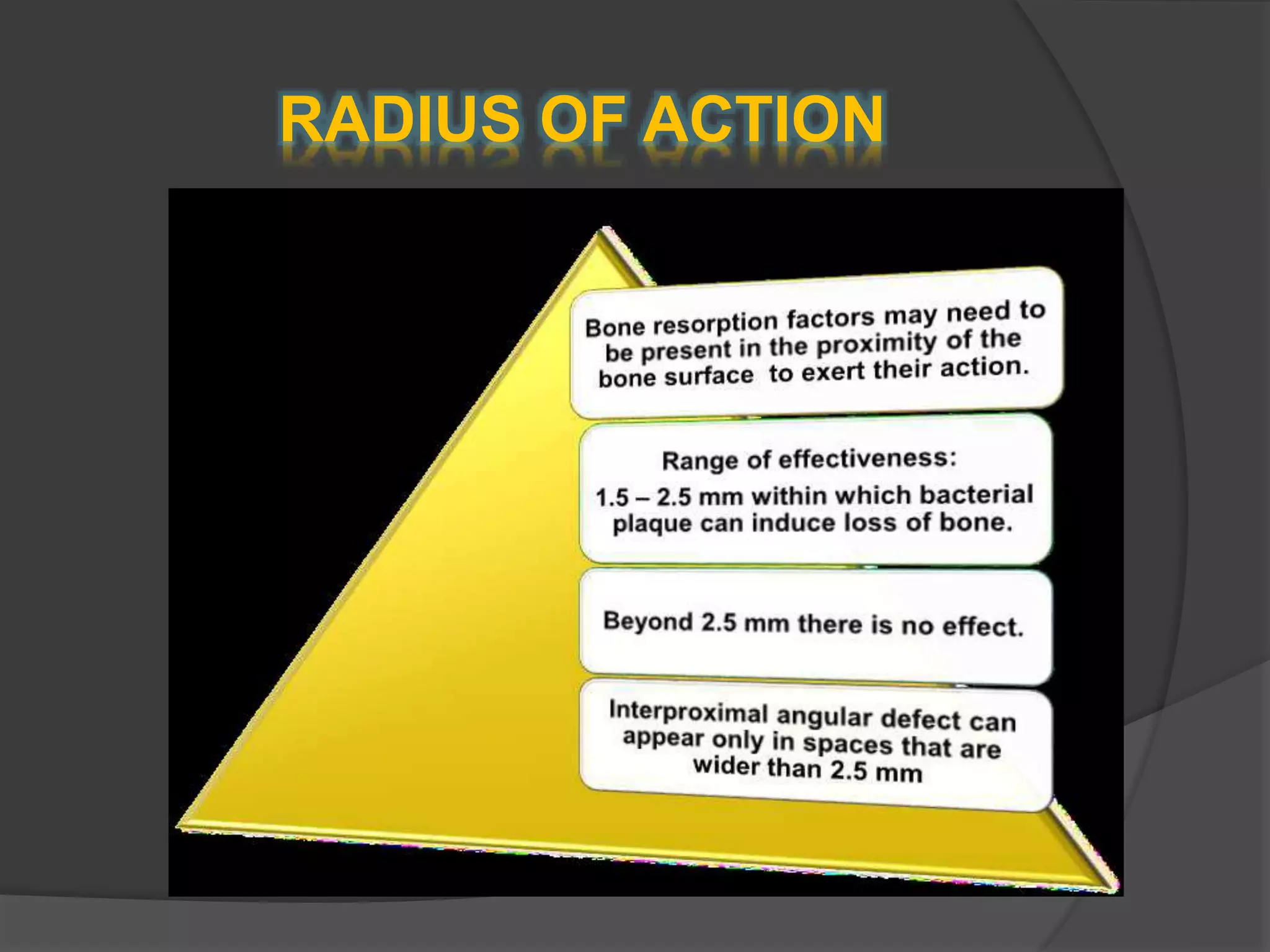
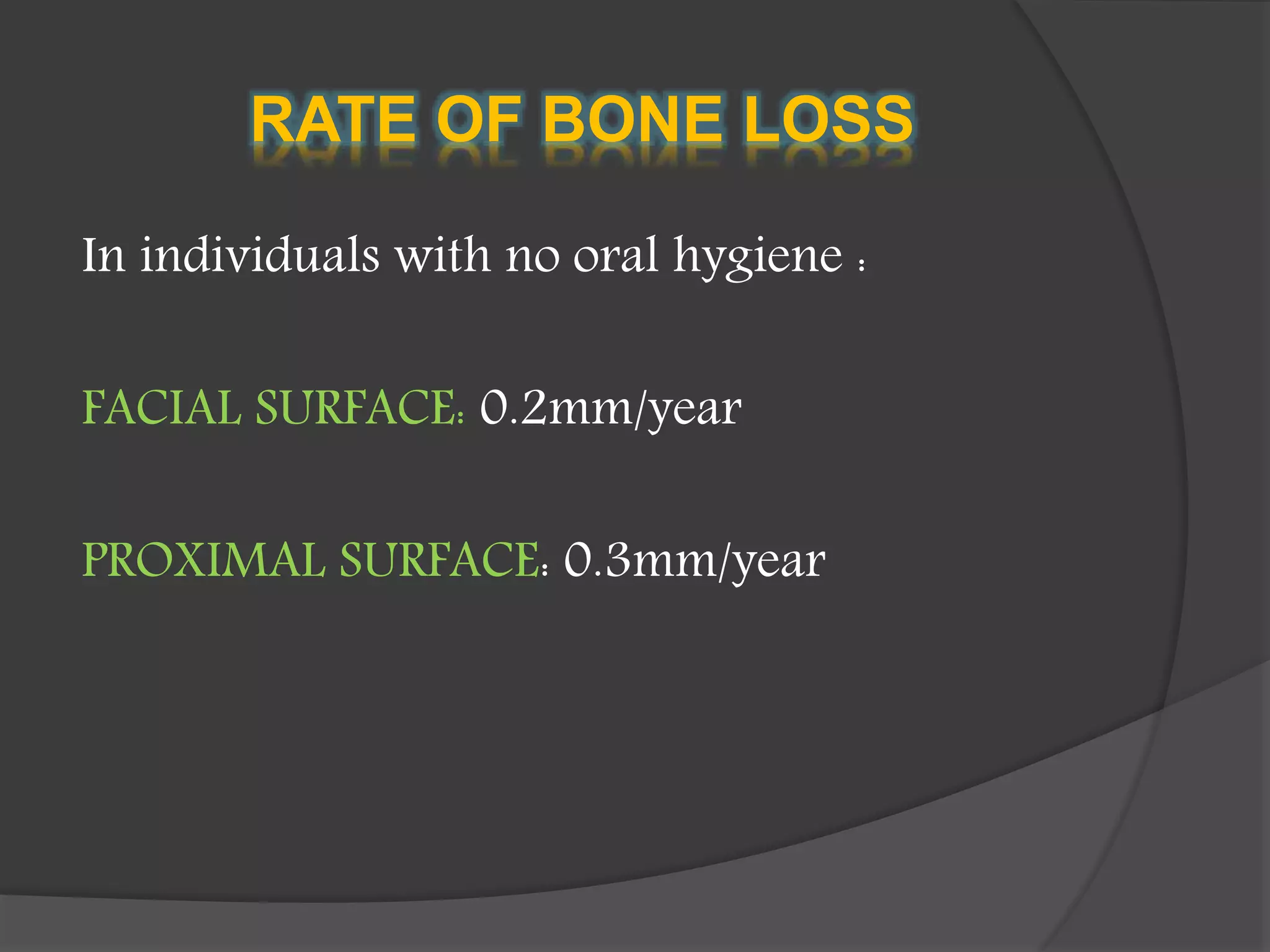
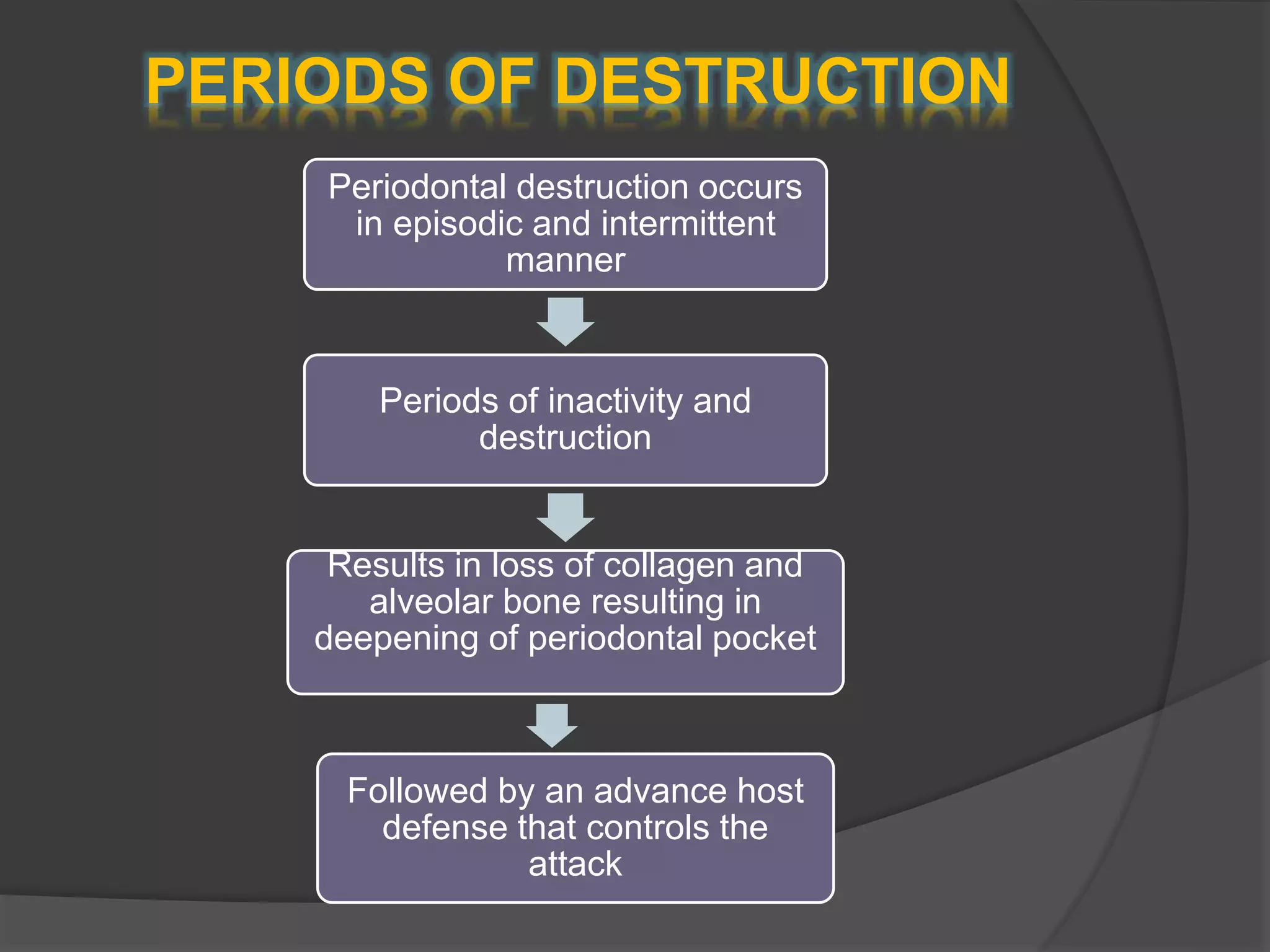
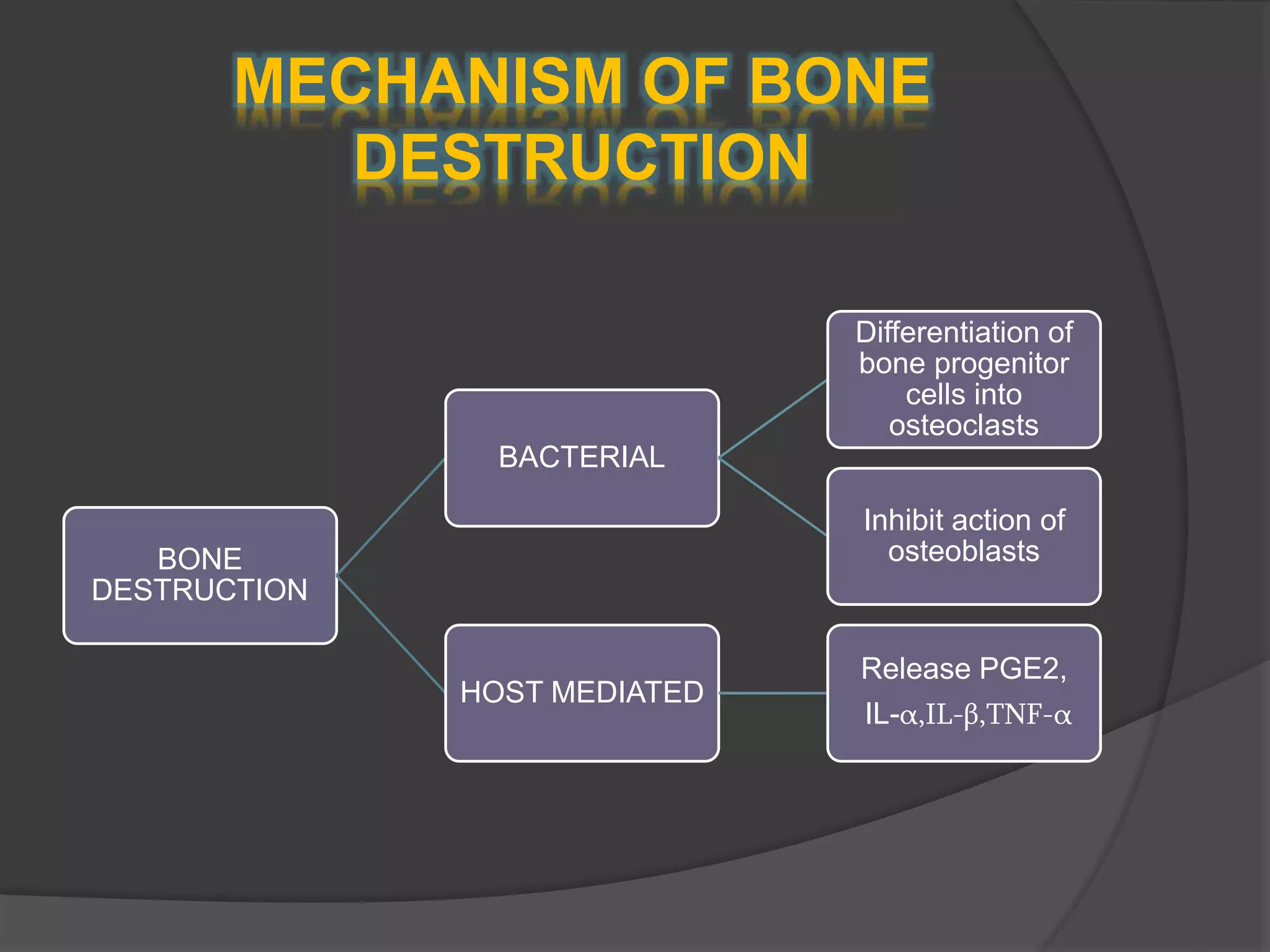
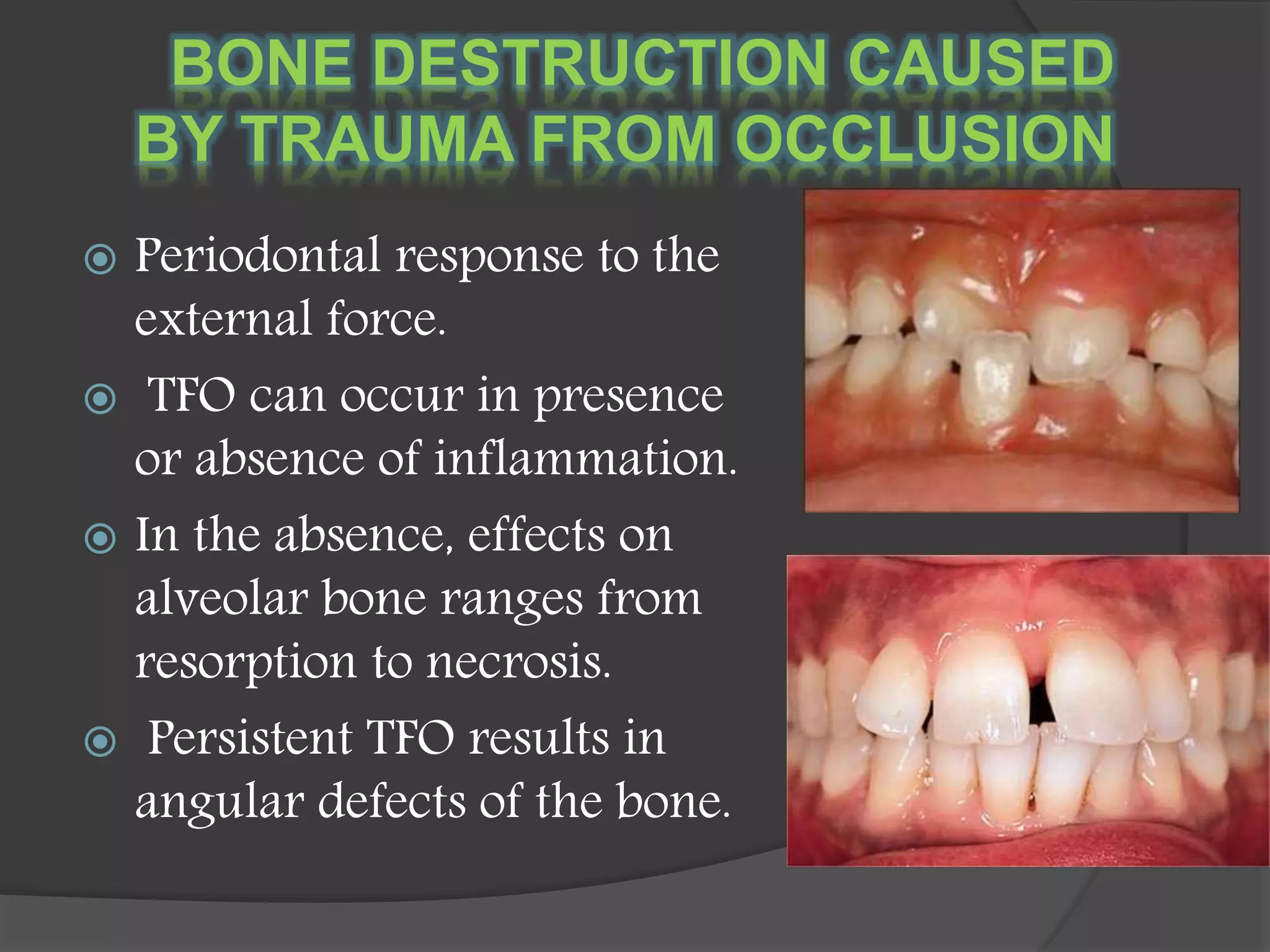
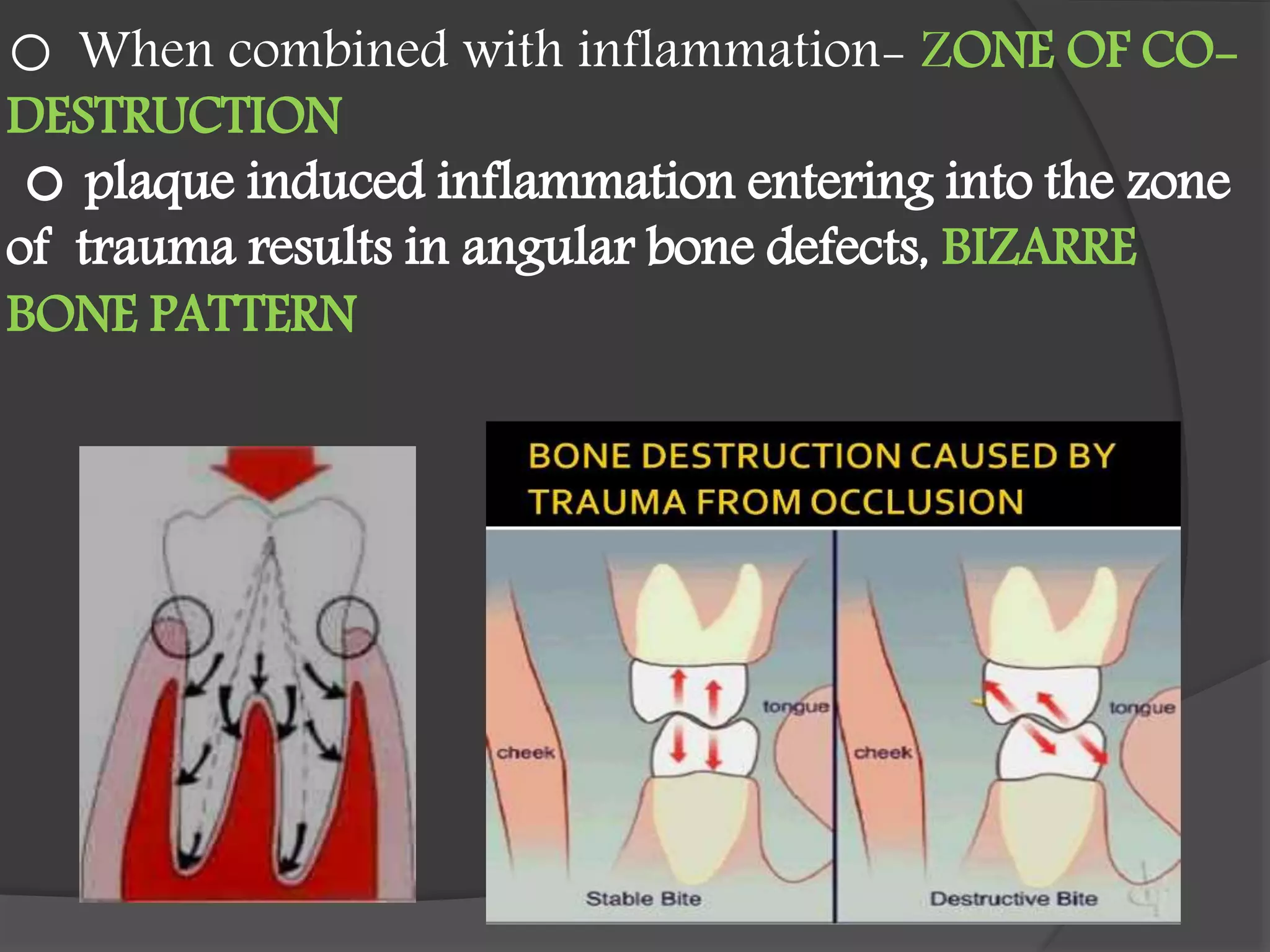
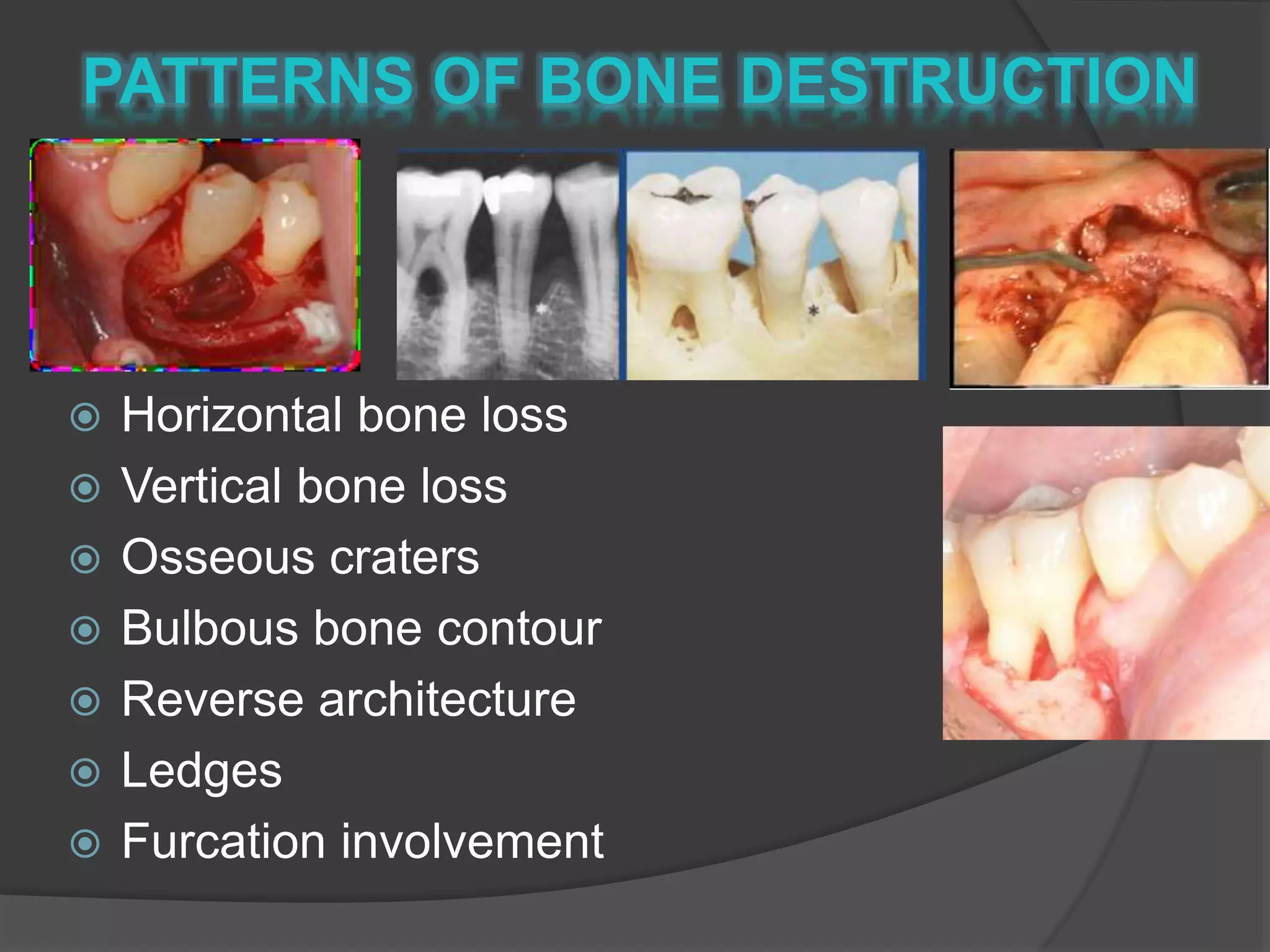
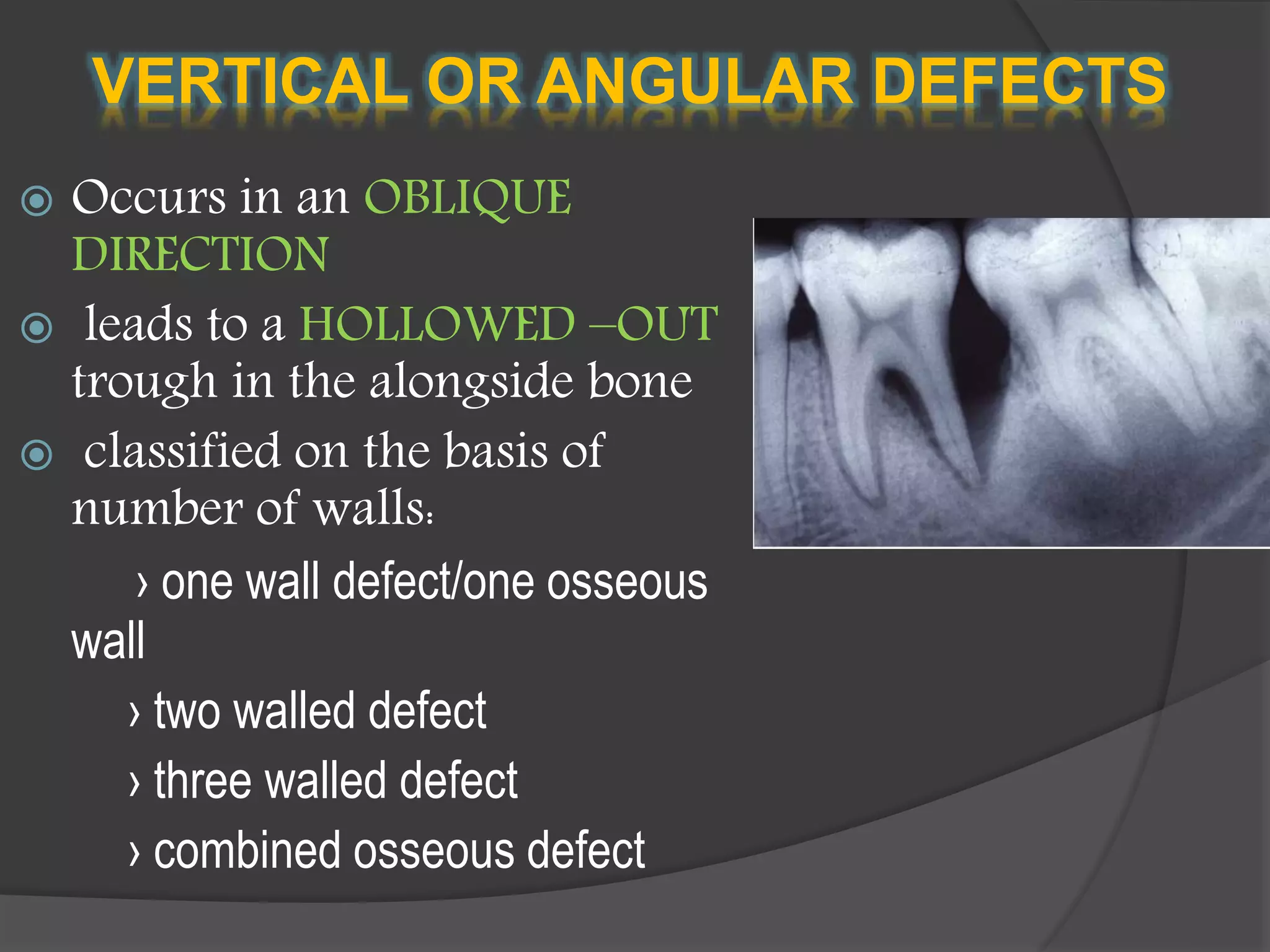
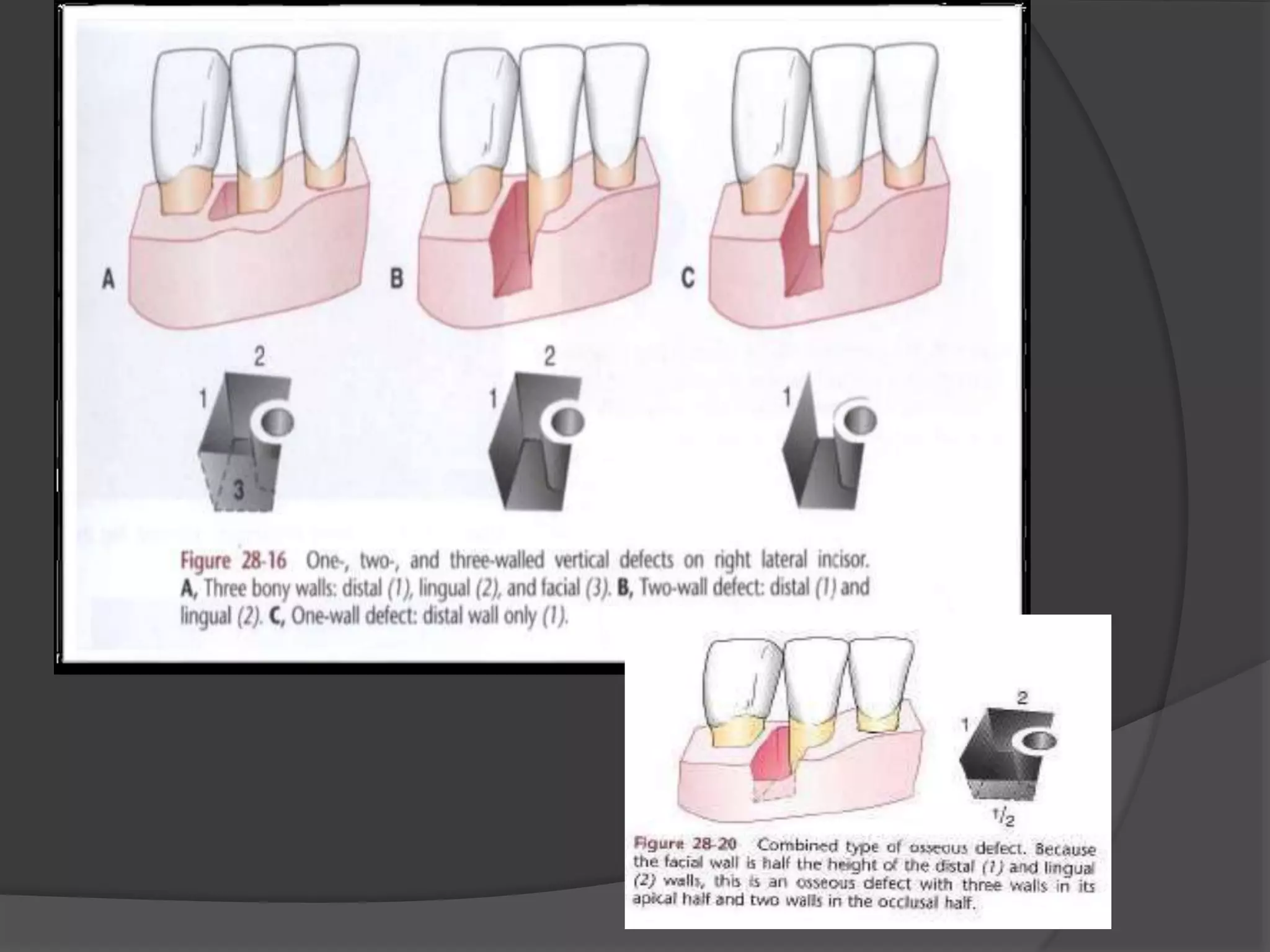
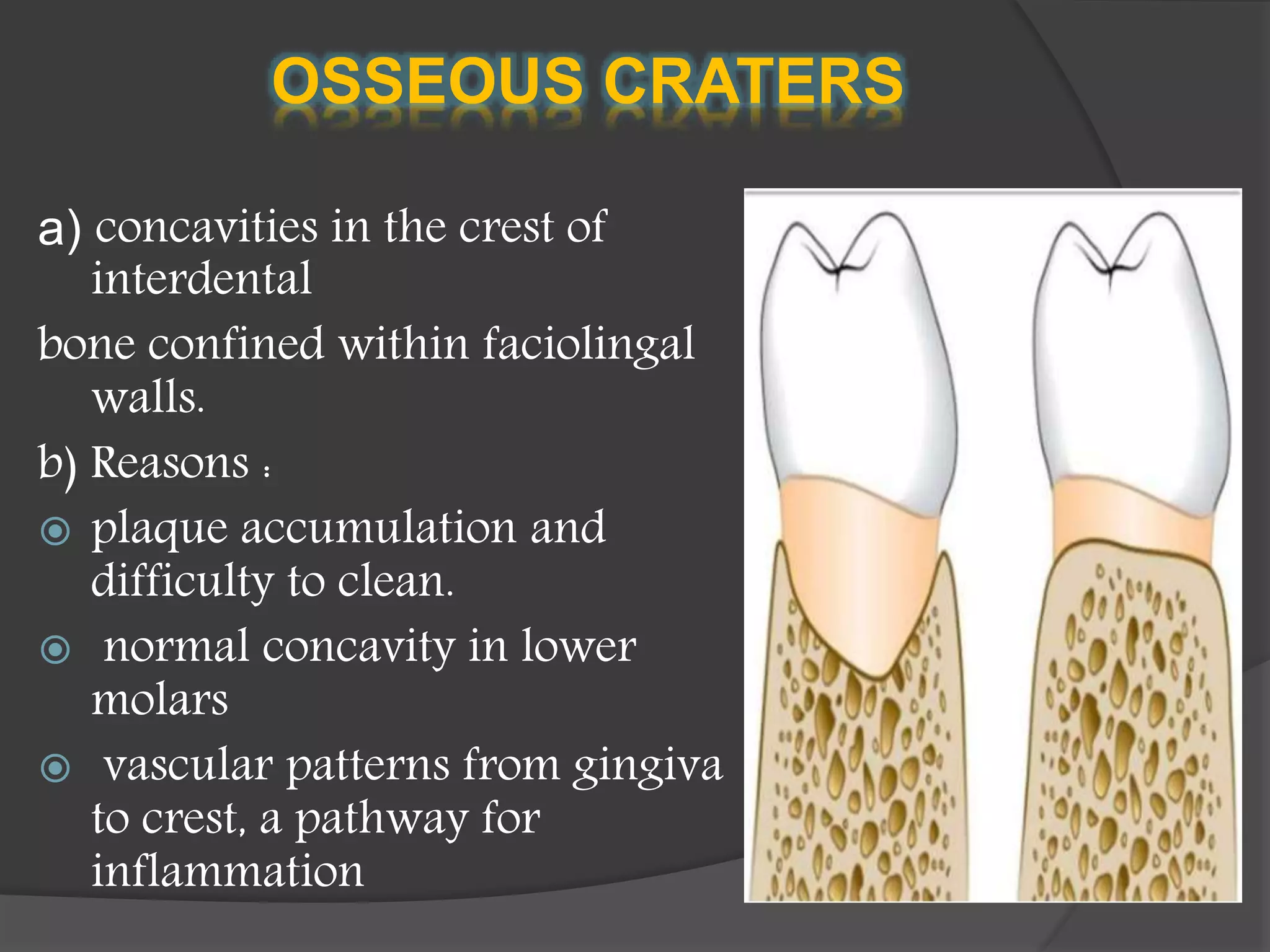
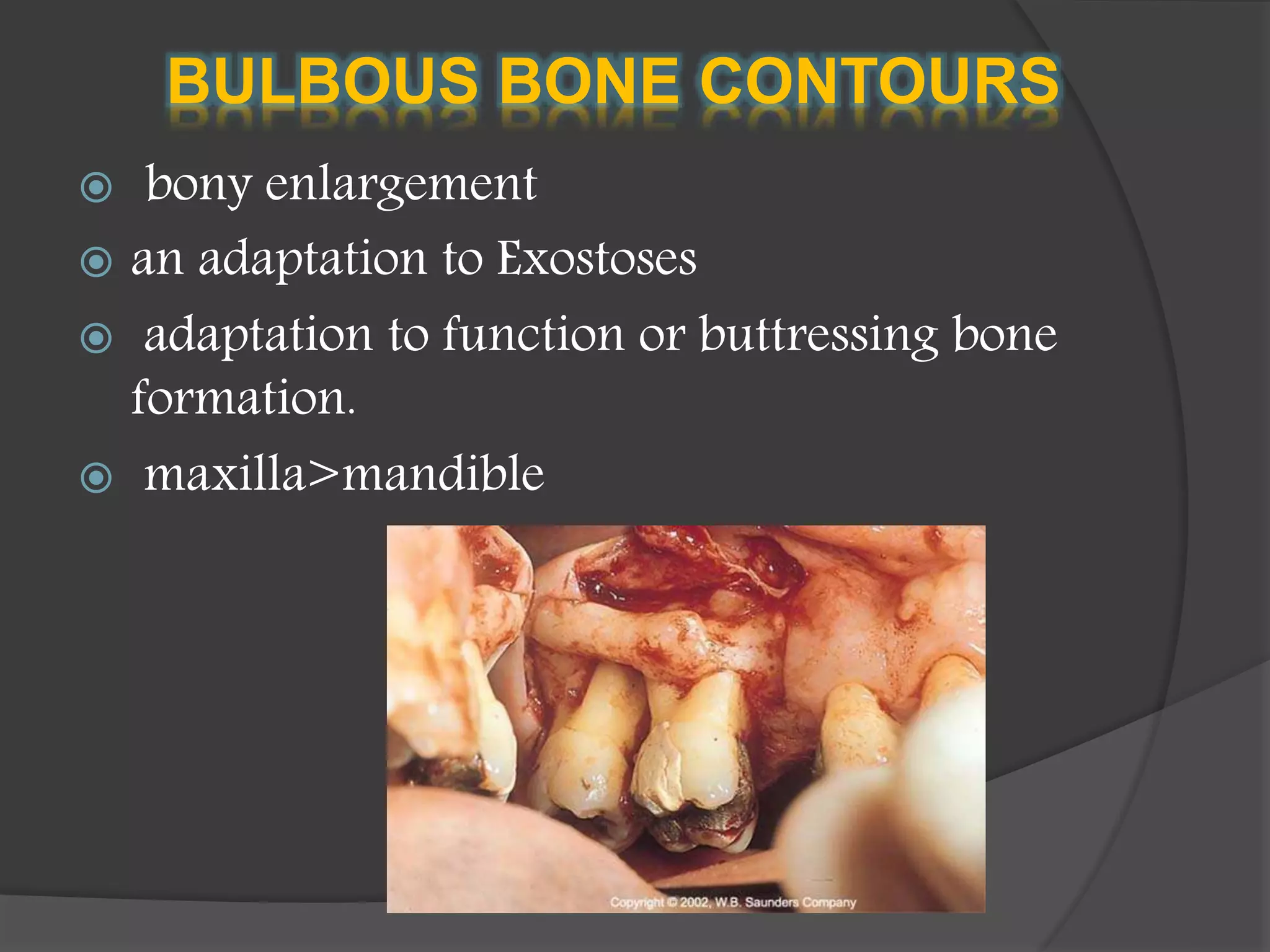
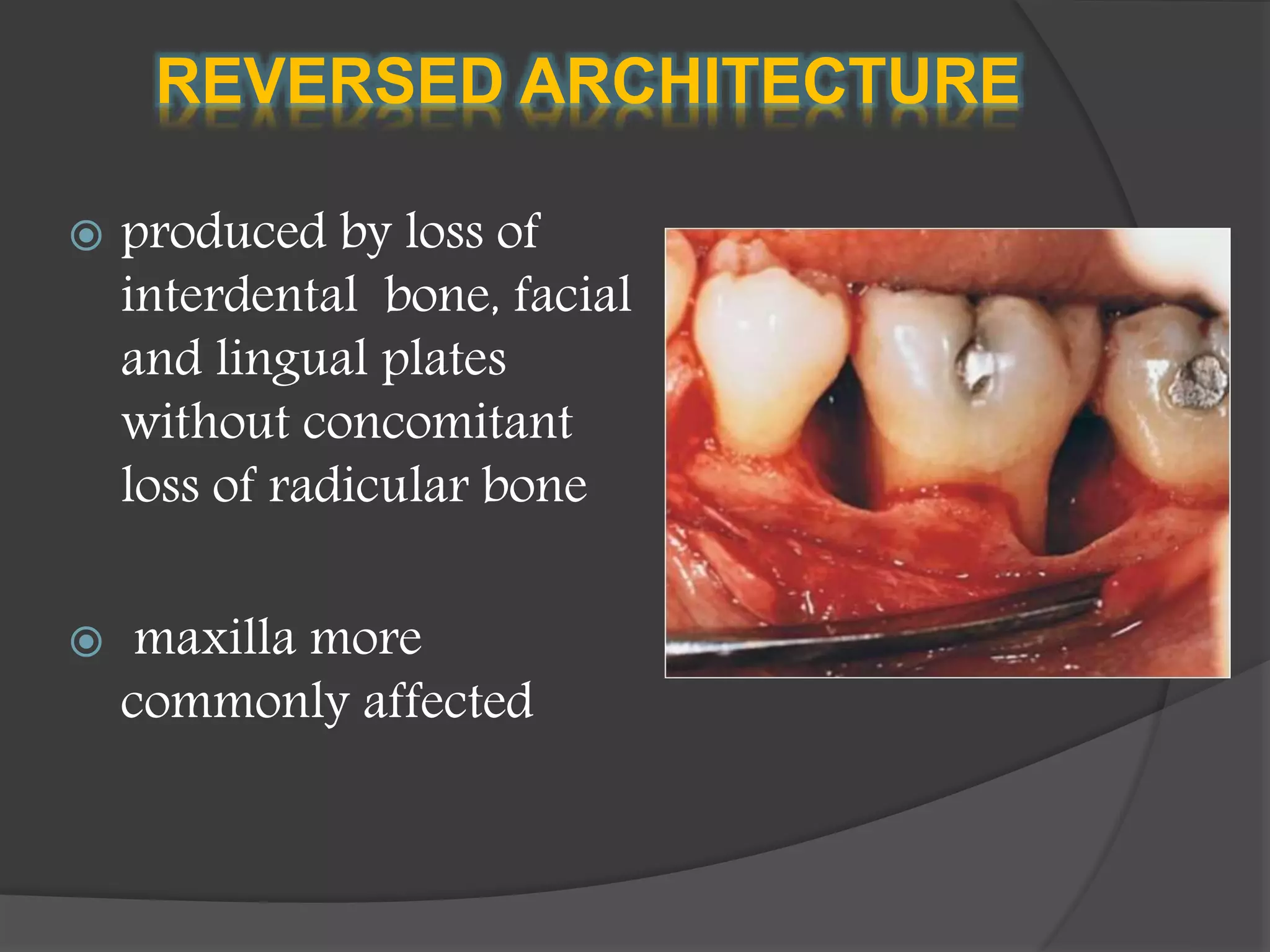
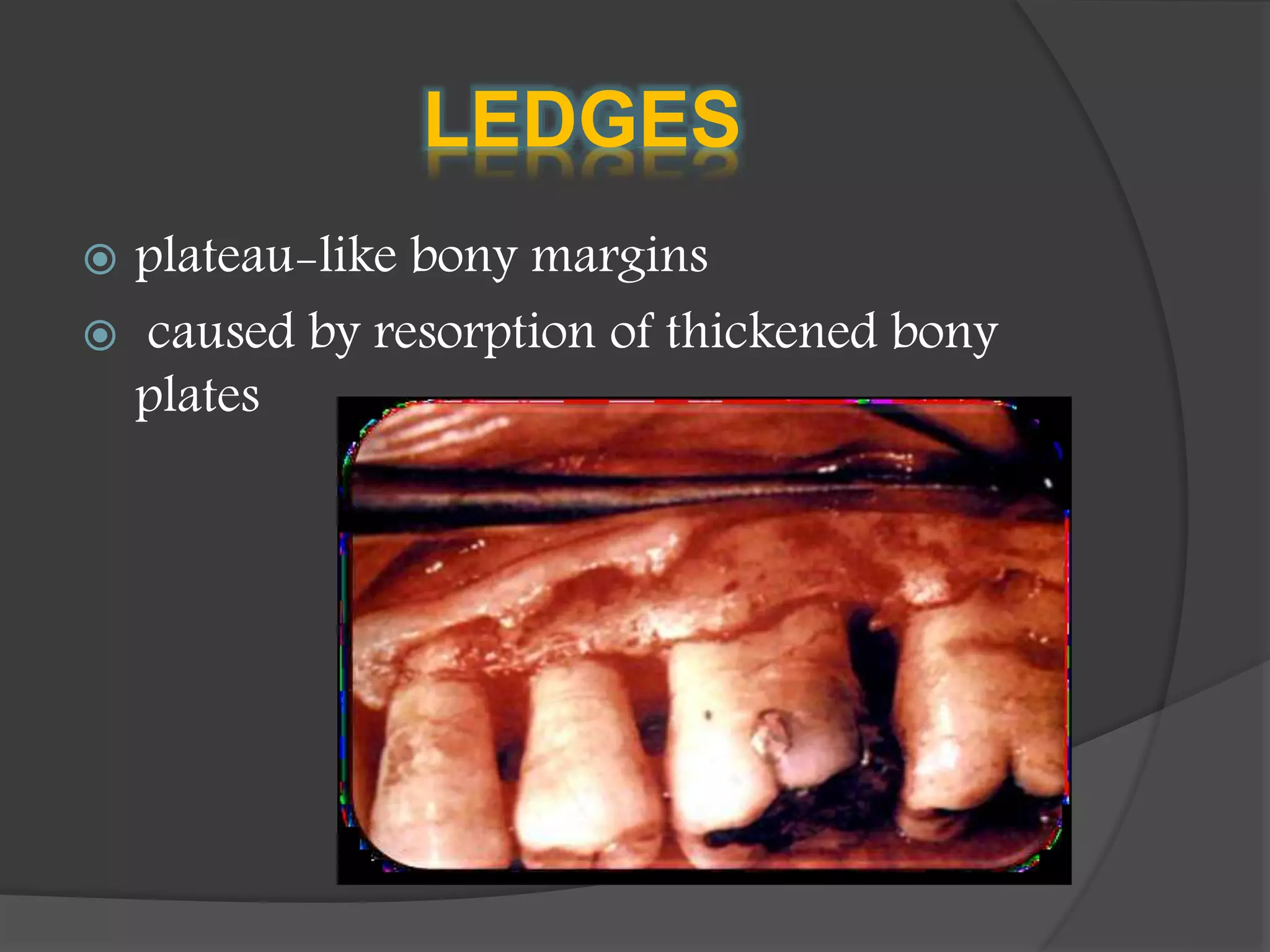
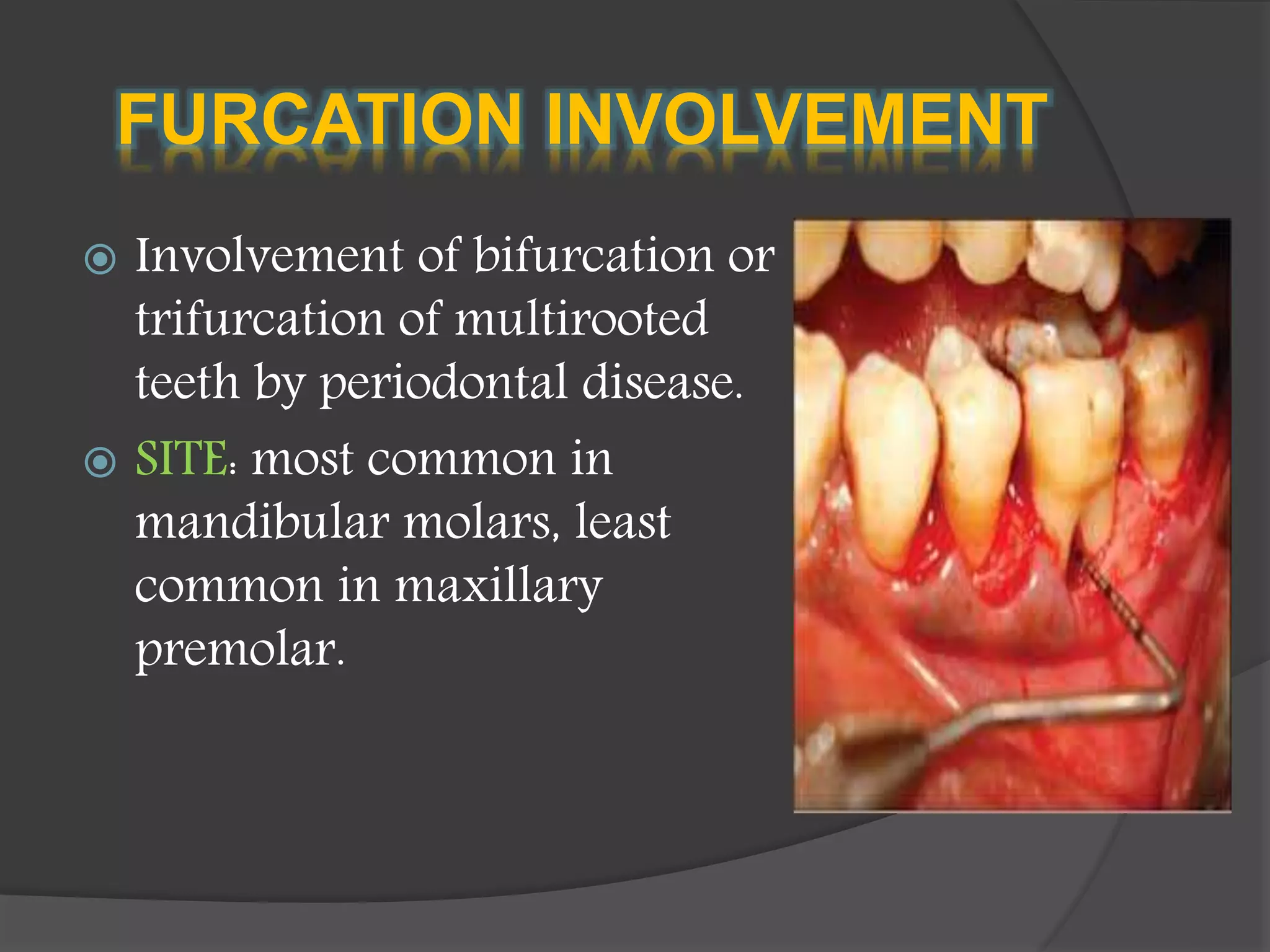
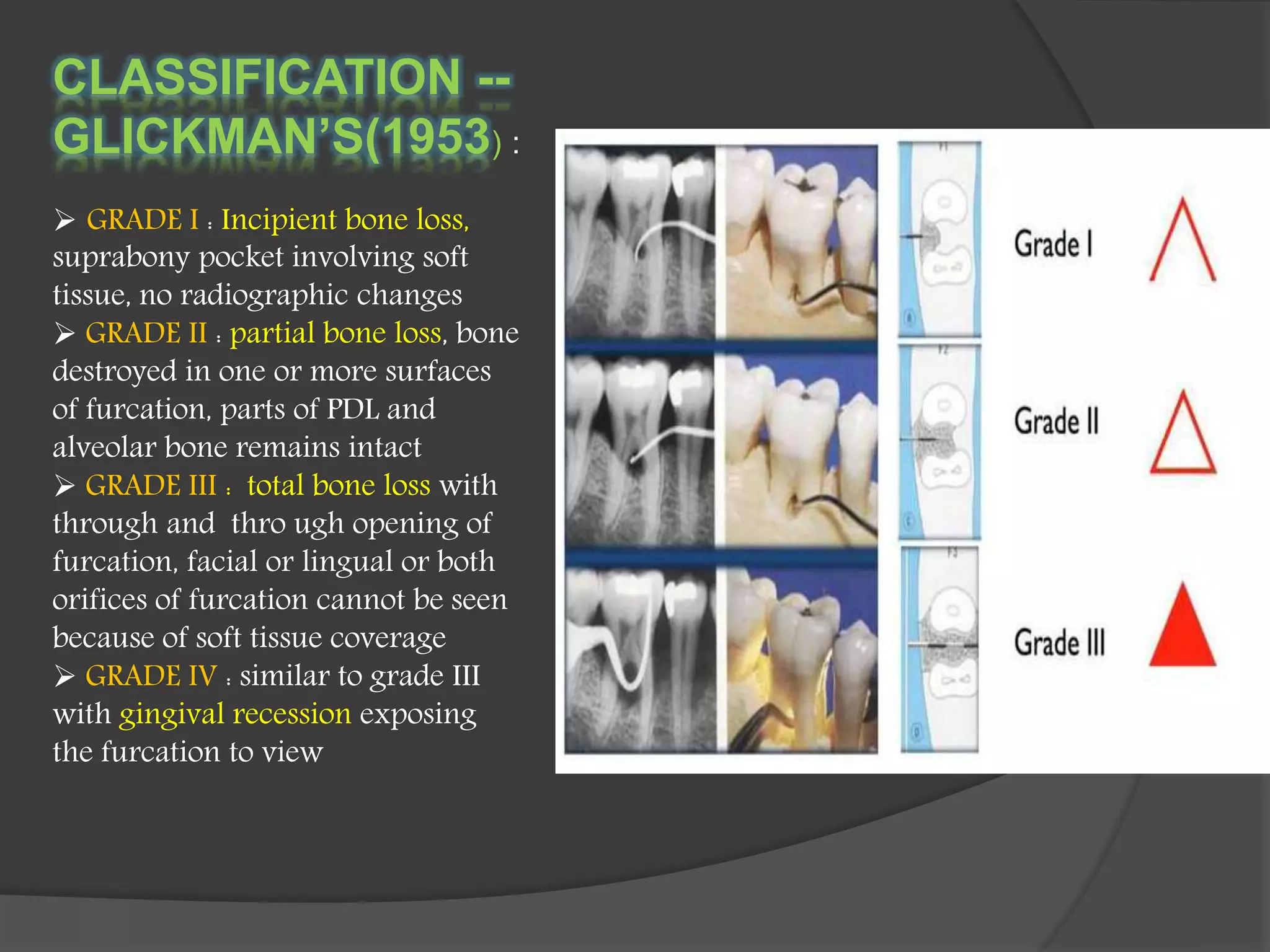
The document discusses the role of the alveolar process in tooth support and the consequences of bone resorption leading to tooth loss, primarily due to gingival inflammation transitioning to periodontitis. It details how systemic factors, trauma from occlusion, and various forms of bone loss contribute to periodontal disease, emphasizing different pathological conditions and classifications of bone loss patterns. Management strategies for periodontal disease are contingent on the specific type of bone loss exhibited.