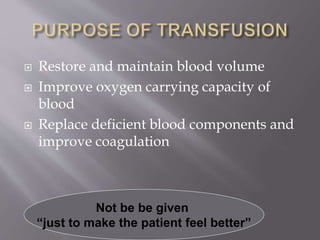
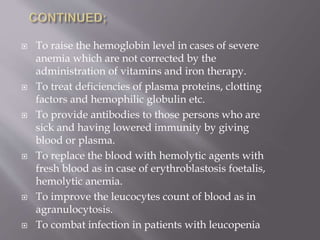
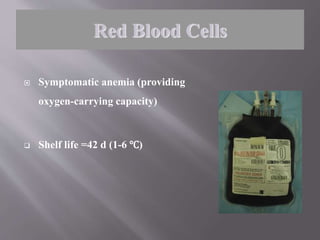
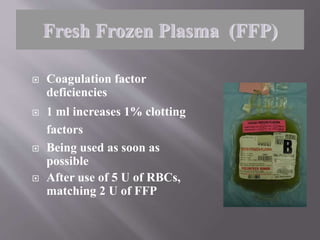
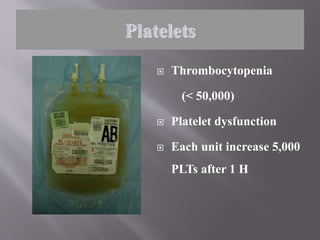
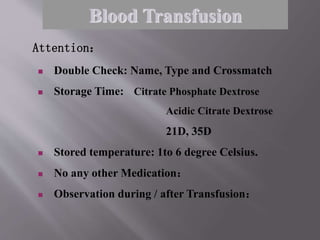
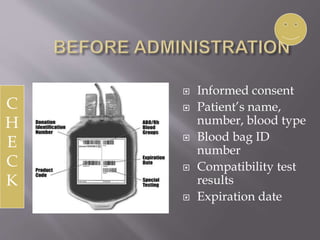
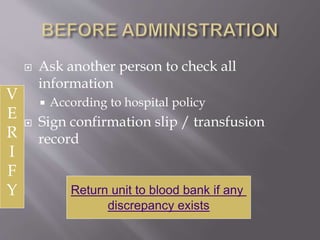
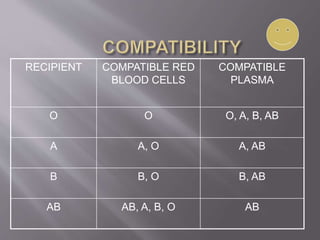
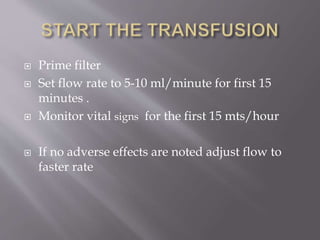
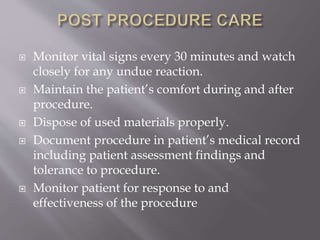
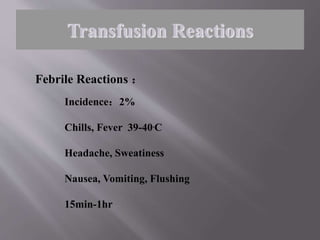
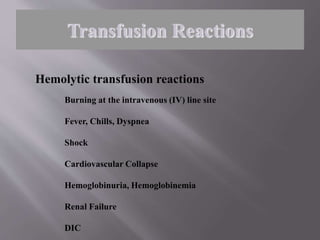
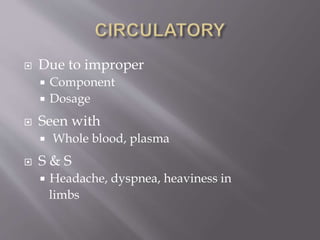
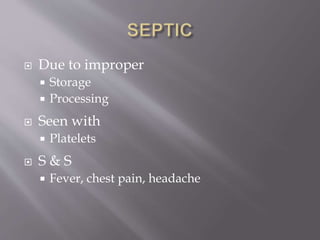
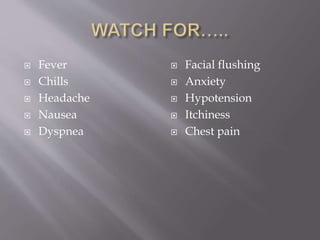
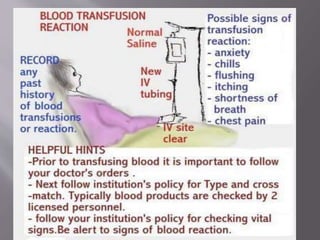
Blood transfusion involves transferring blood or blood products from a donor into the recipient's circulatory system. It can be a life-saving procedure used to treat massive blood loss, anemia, or replace deficient blood components. The main components transfused are red blood cells, plasma, platelets, and cryoprecipitate. Careful checking and monitoring is required during and after a transfusion to watch for any adverse reactions and ensure the health and safety of the patient.