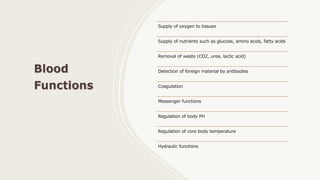
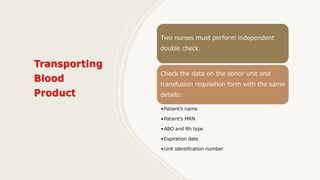
The document provides information on blood and blood products safety. It discusses types of blood products, the safe transfusion process including proper storage, collection, transportation and administration. It outlines the nurse's role in verifying transfusion orders and consent, collecting samples, transporting blood products, administering transfusions and monitoring for transfusion reactions. It also addresses donor eligibility criteria, deferrals due to medical history, immunizations or illnesses.