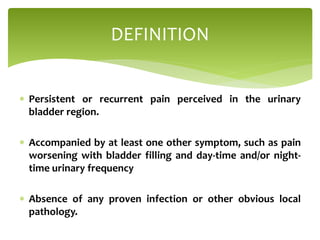
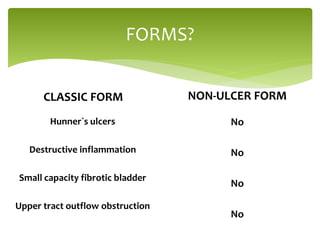
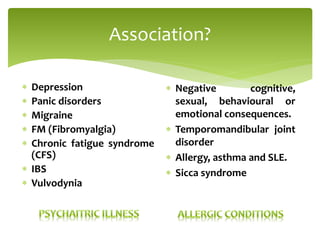
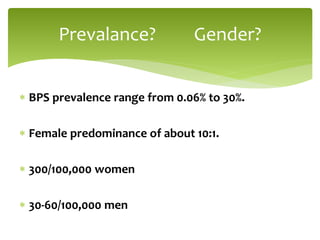
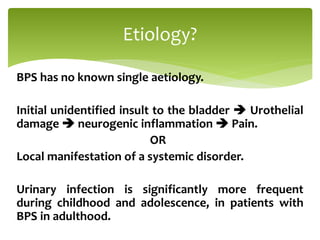
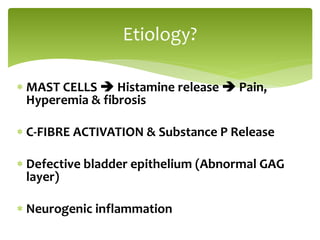
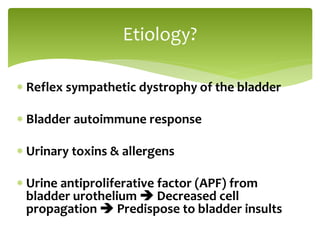
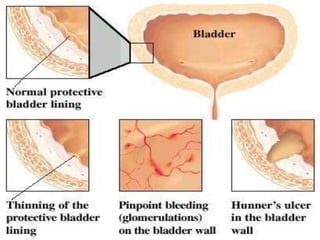
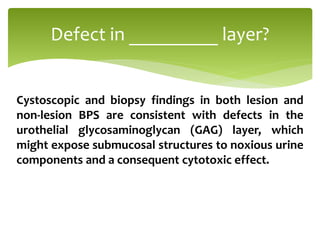
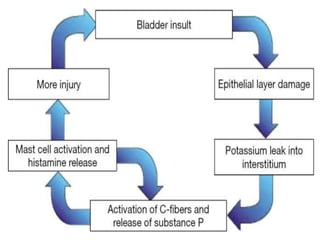
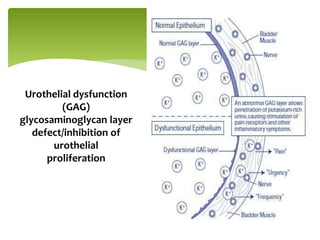
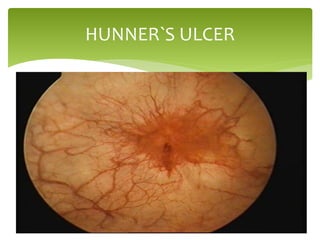
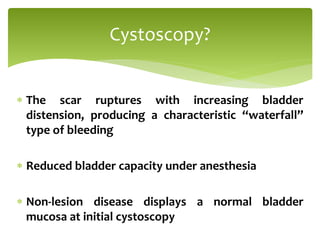
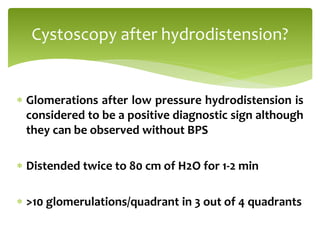
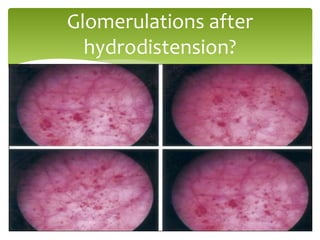
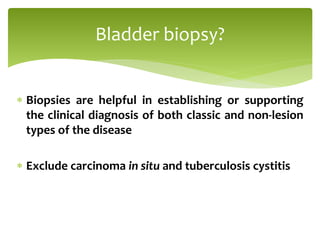
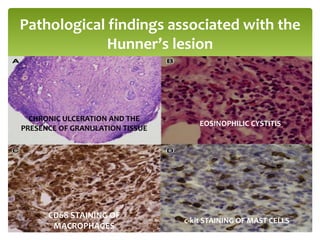
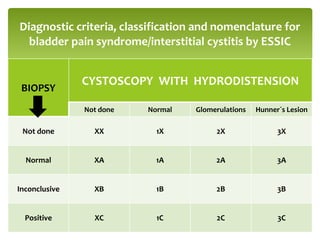
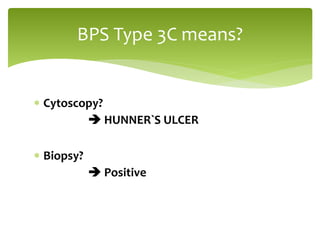
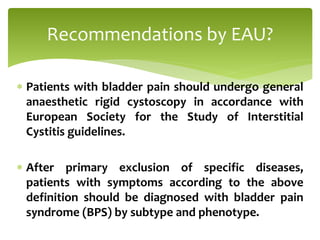
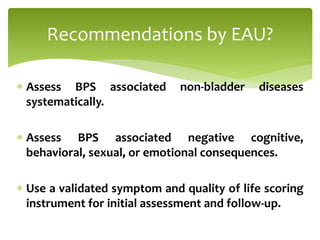
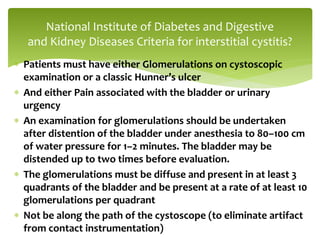
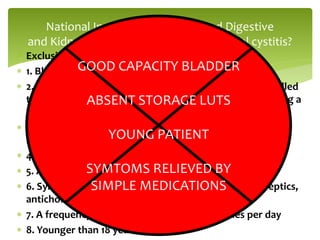
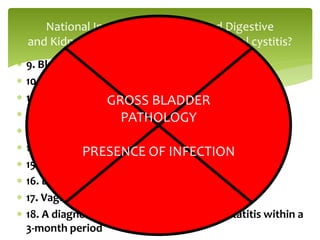
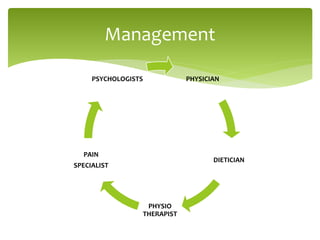
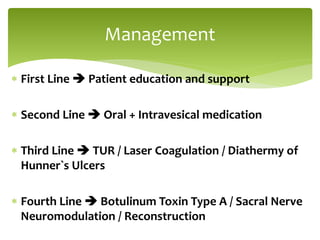
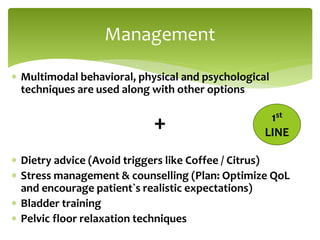
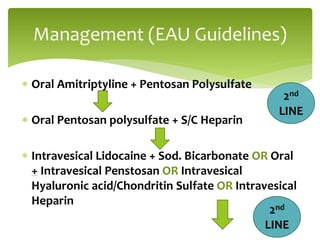
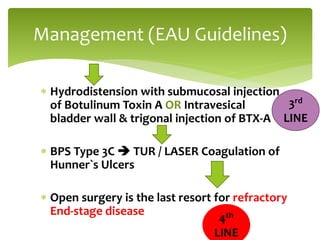
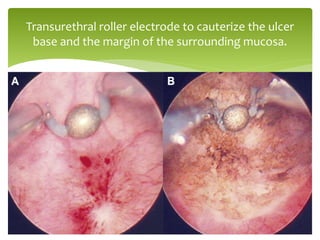
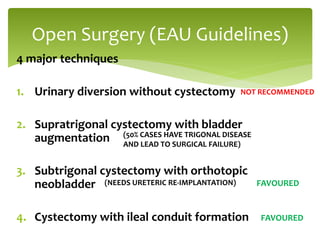
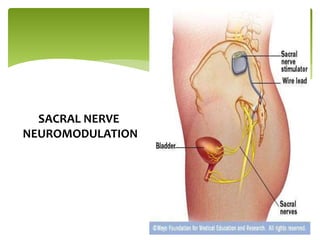
Bladder Pain Syndrome (BPS) is characterized by persistent bladder region pain along with additional symptoms like urinary frequency, without any proven infection. It may exist in classic forms with Hunner's ulcers or non-ulcer forms, with a prevalence range of 0.06% to 30% and a notable female predominance. Management includes education, medications, hydrodistension, and potential surgeries, tailored based on subtype and patient response.