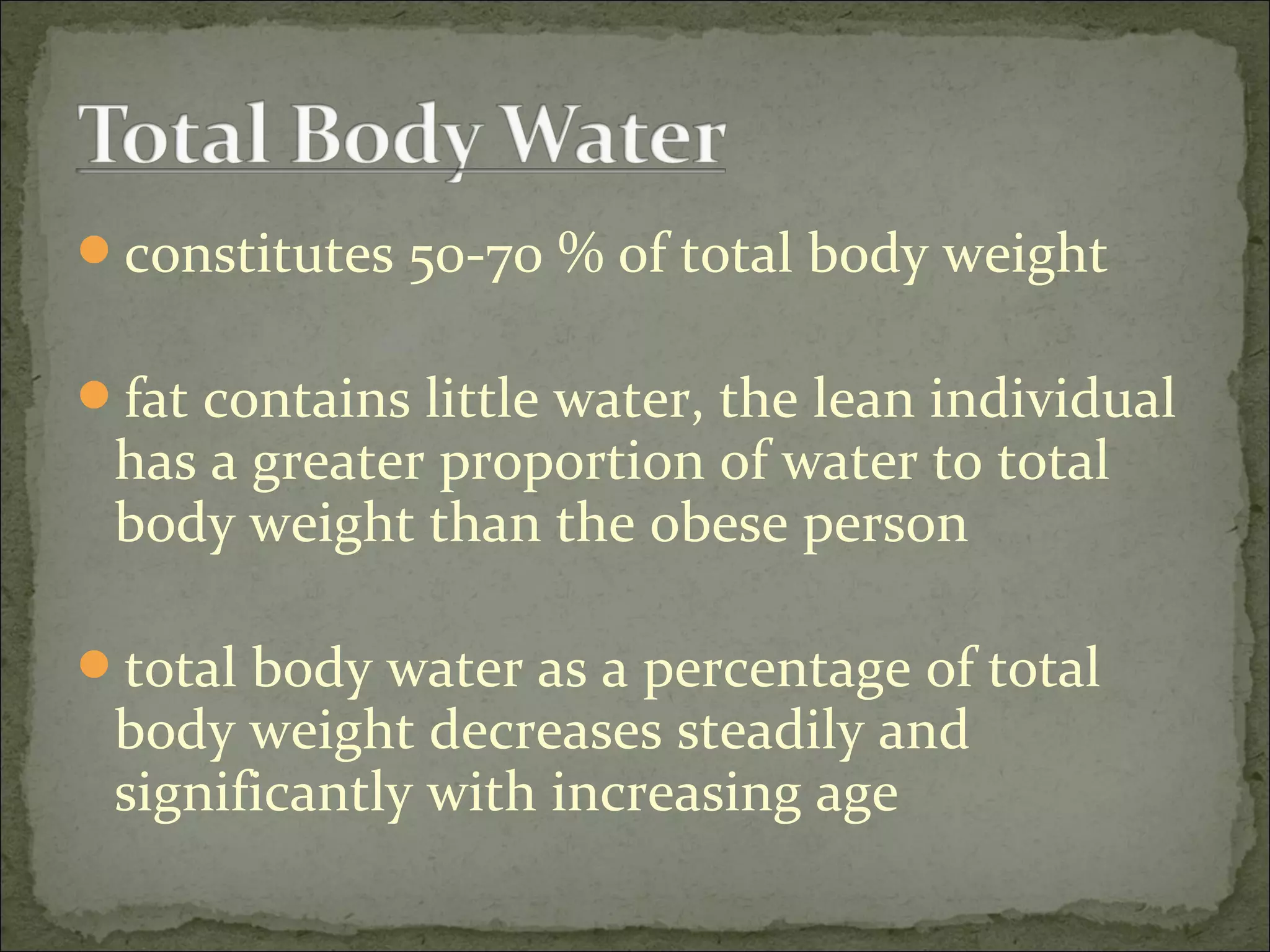
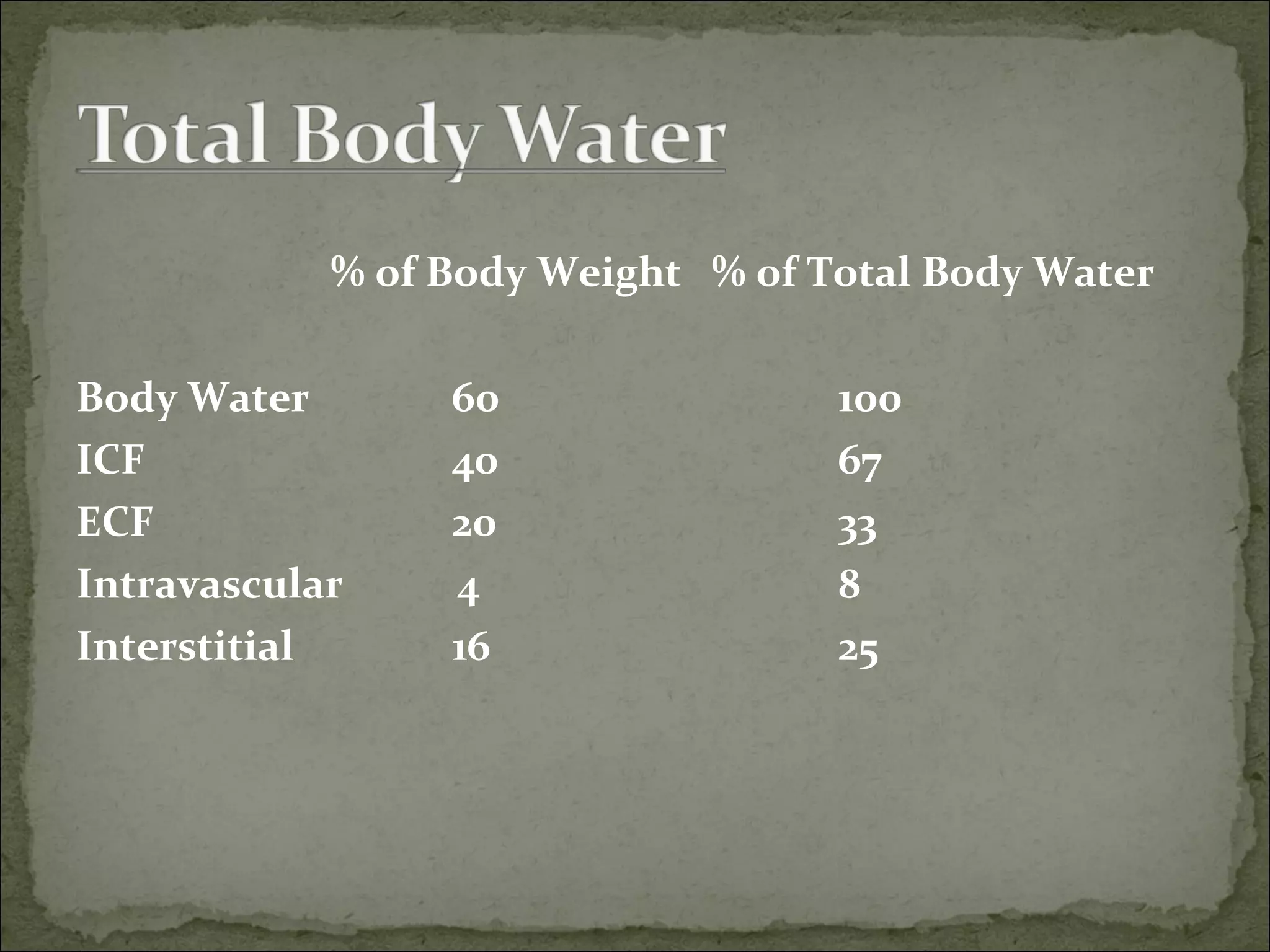
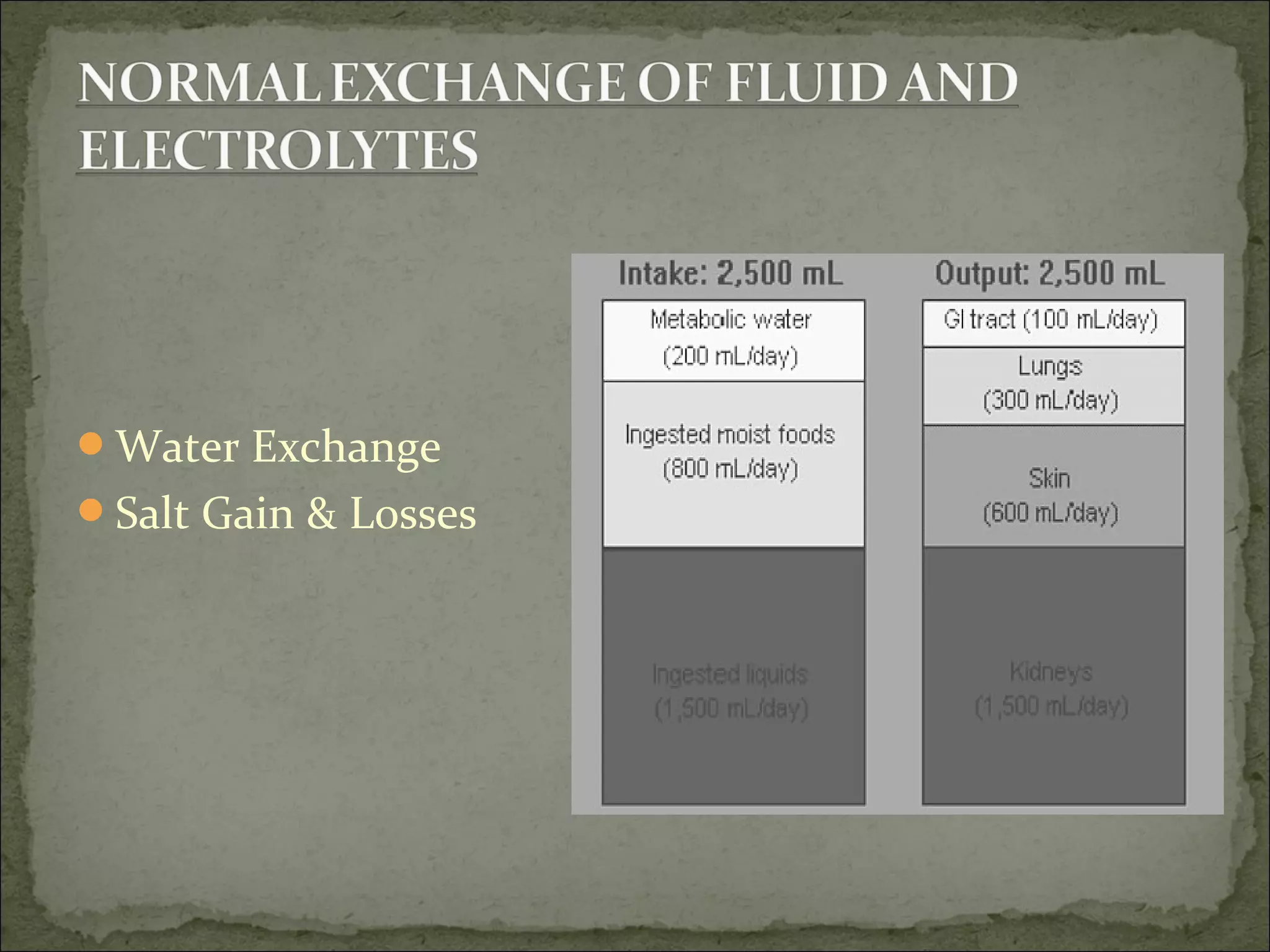
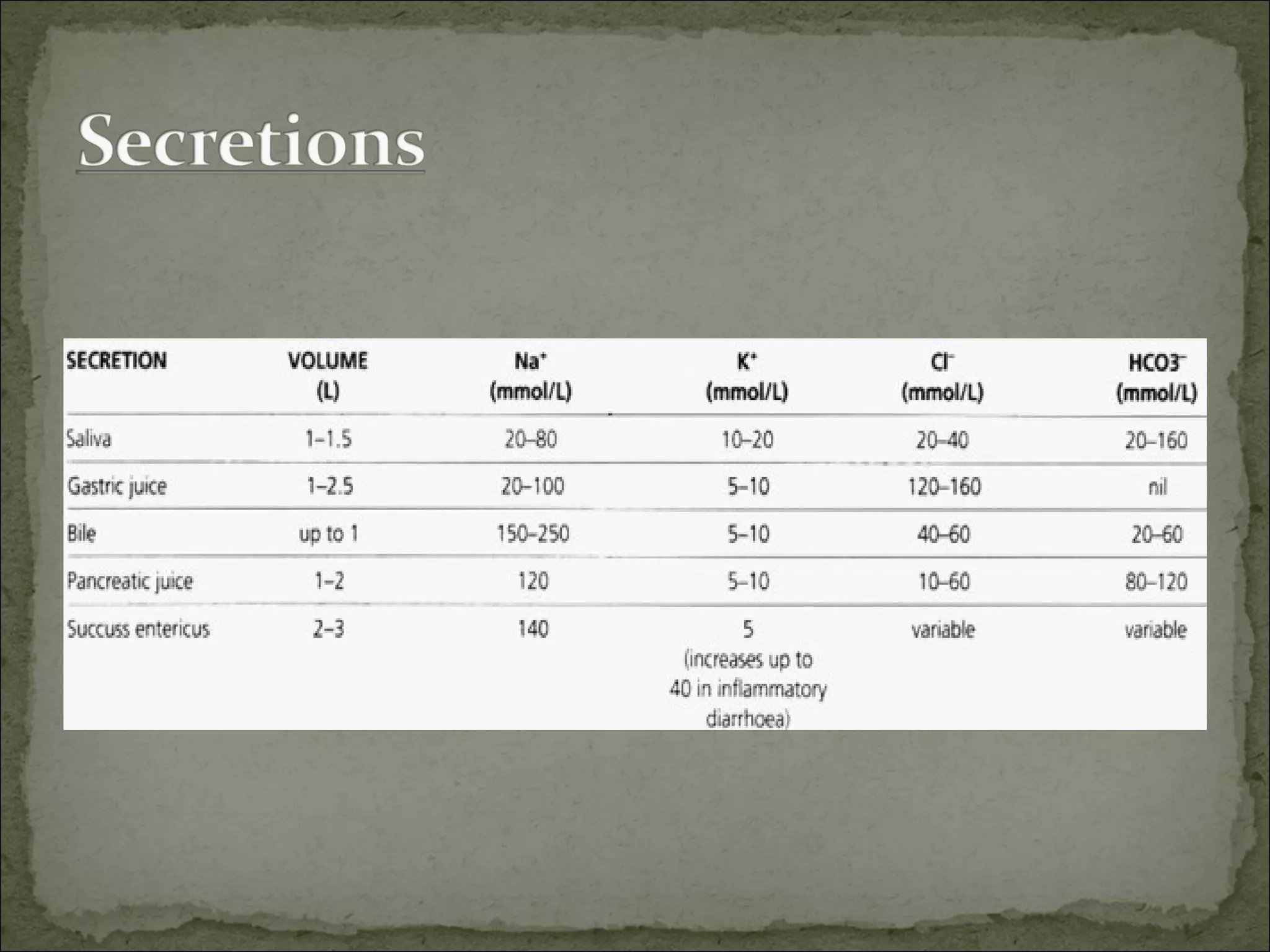
The document provides a comprehensive overview of body water composition, fluid balance, and electrolyte management in clinical settings. It discusses the significance of total body water, the role of various cations and anions, and details daily water intake and losses. Additionally, it outlines the clinical implications of fluid volume deficits and excesses, alongside signs and symptoms associated with imbalances in electrolytes like sodium, potassium, calcium, and magnesium.