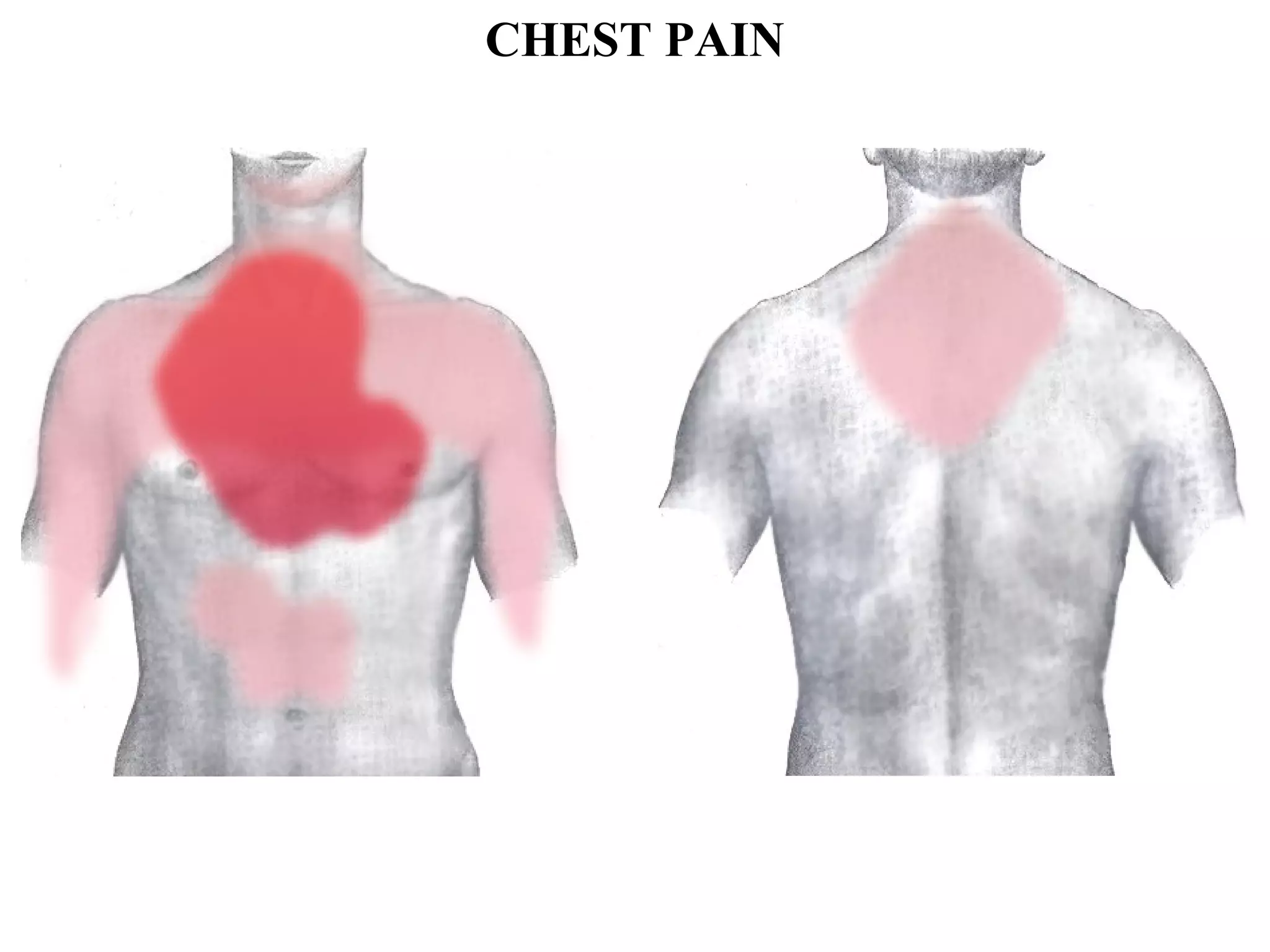
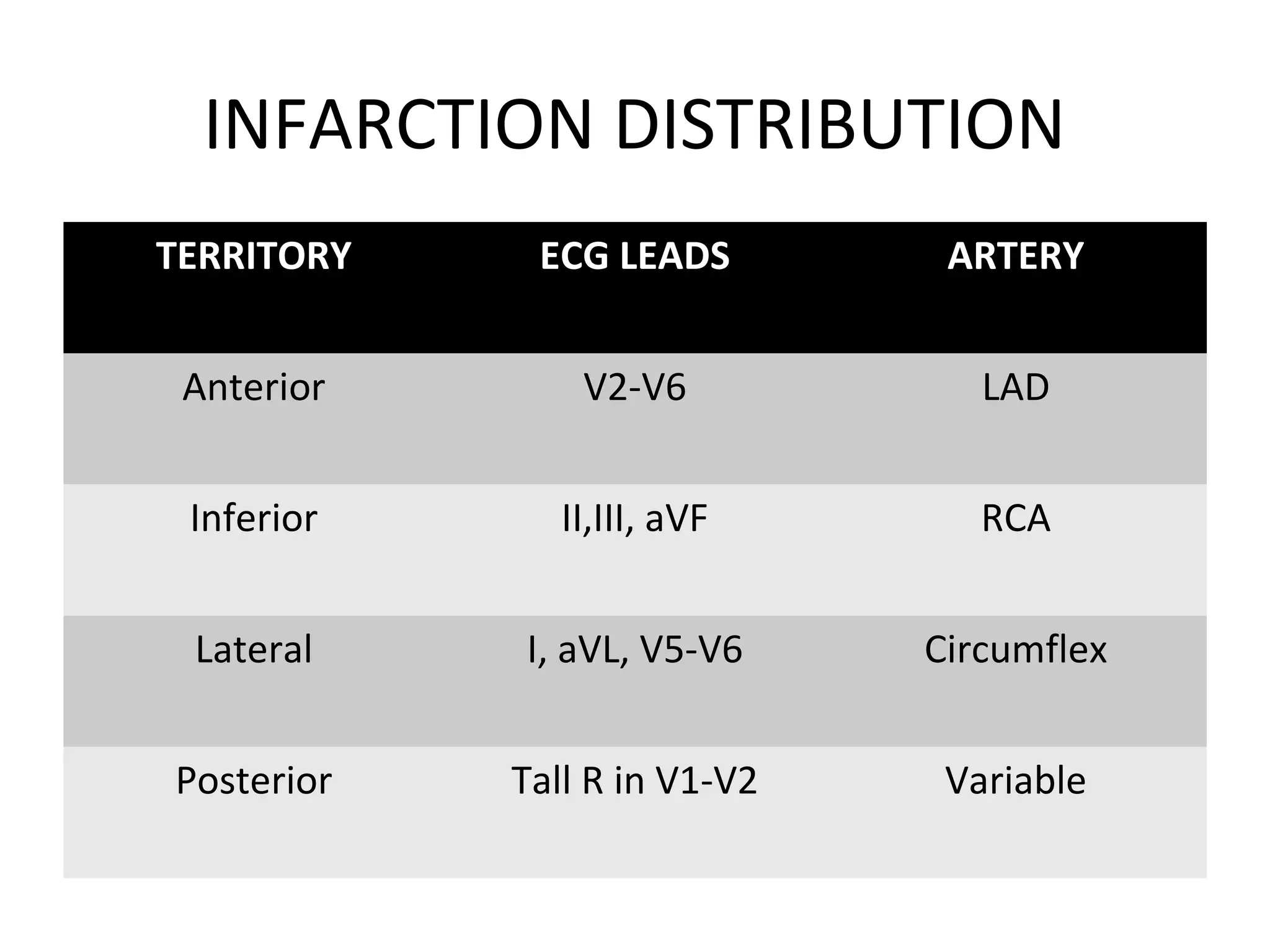
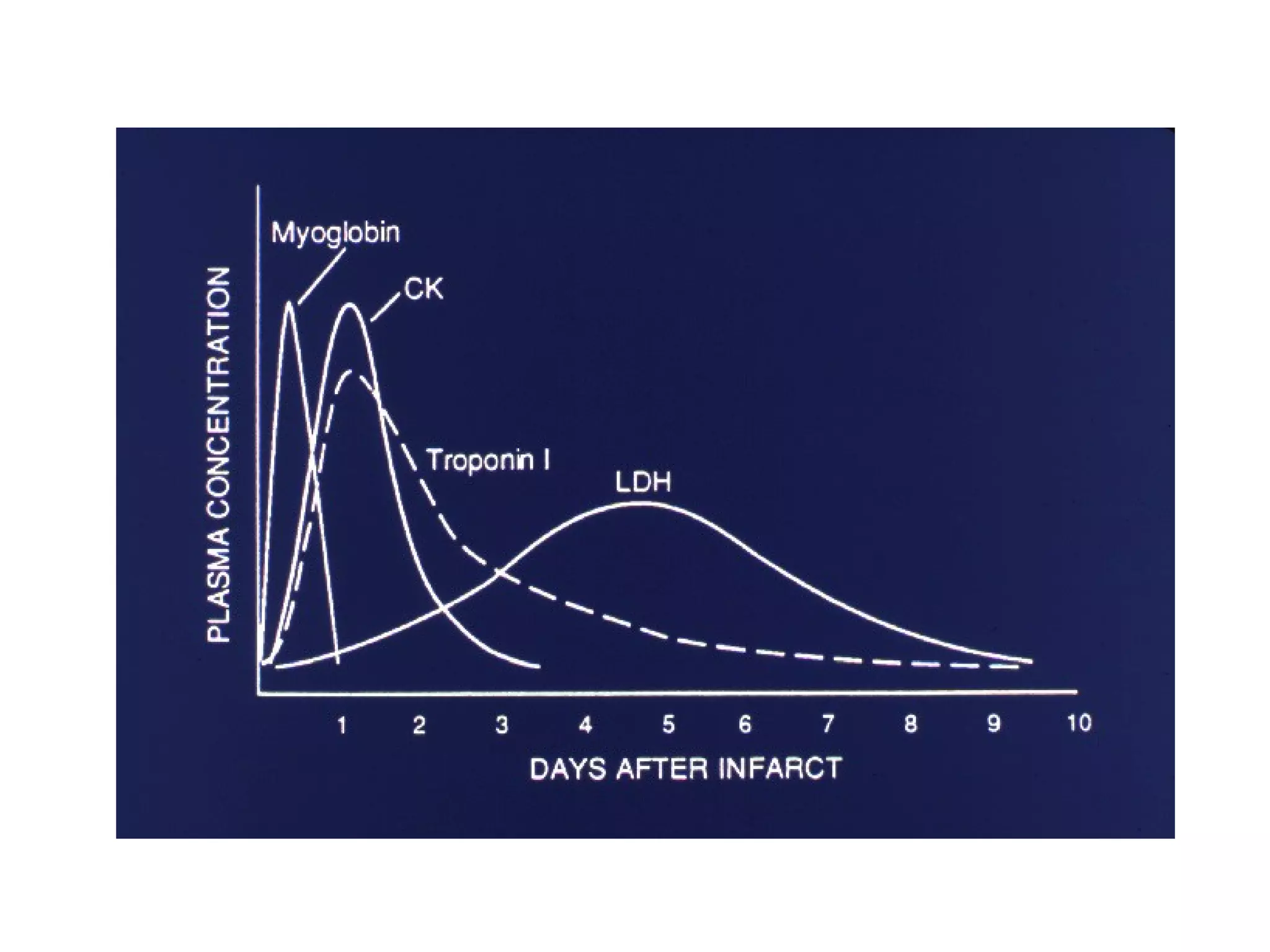
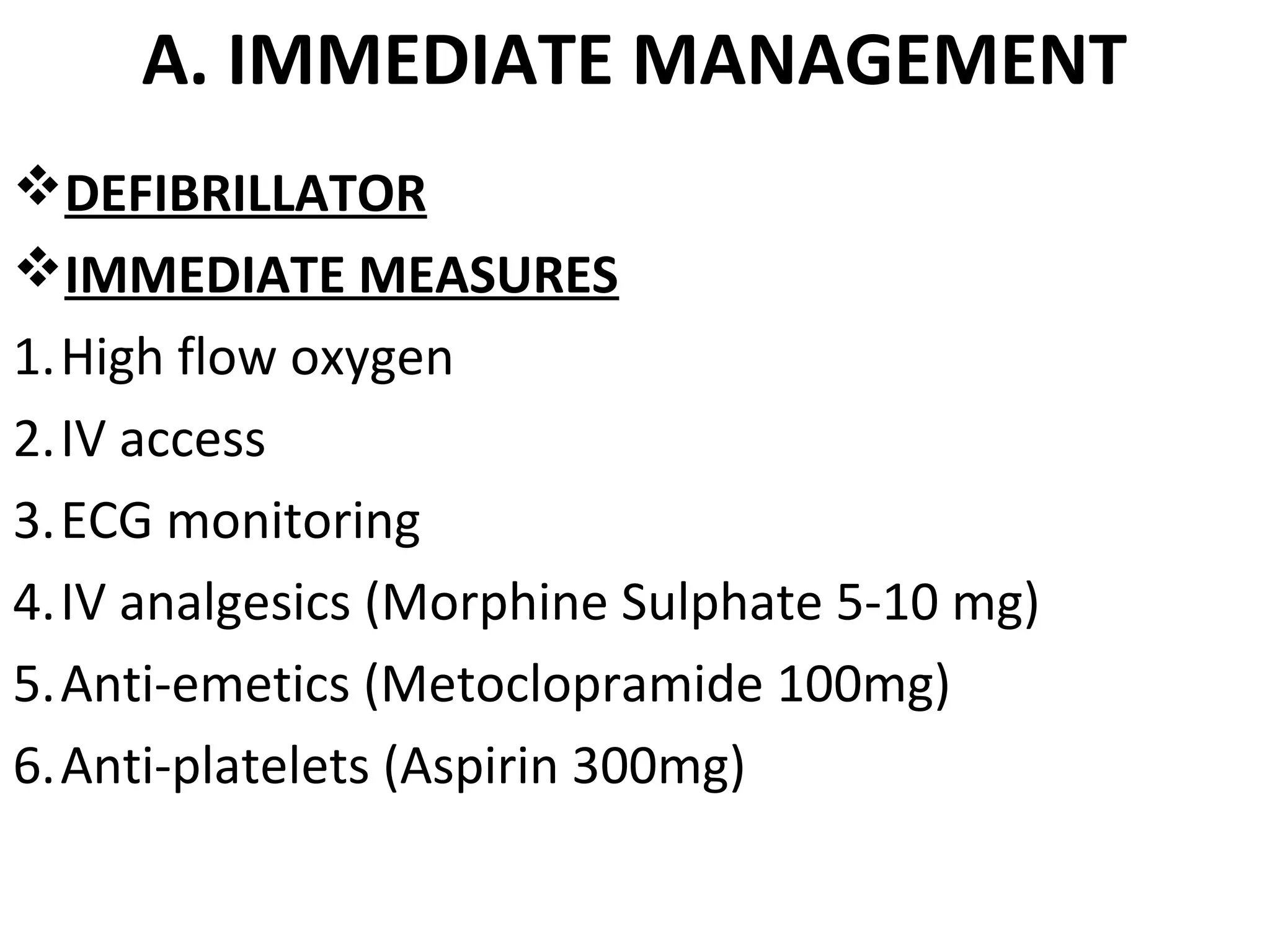
The document provides an extensive overview of coronary arteries and their role in myocardial infarction (MI), including risk factors, symptoms, diagnosis, and management strategies. Key components highlighted include the importance of various cardiac markers for diagnosis, ECG changes, and management protocols such as reperfusion therapy and lifestyle modifications. The prognosis for MI patients is discussed, with statistics on survival rates and factors affecting outcomes.