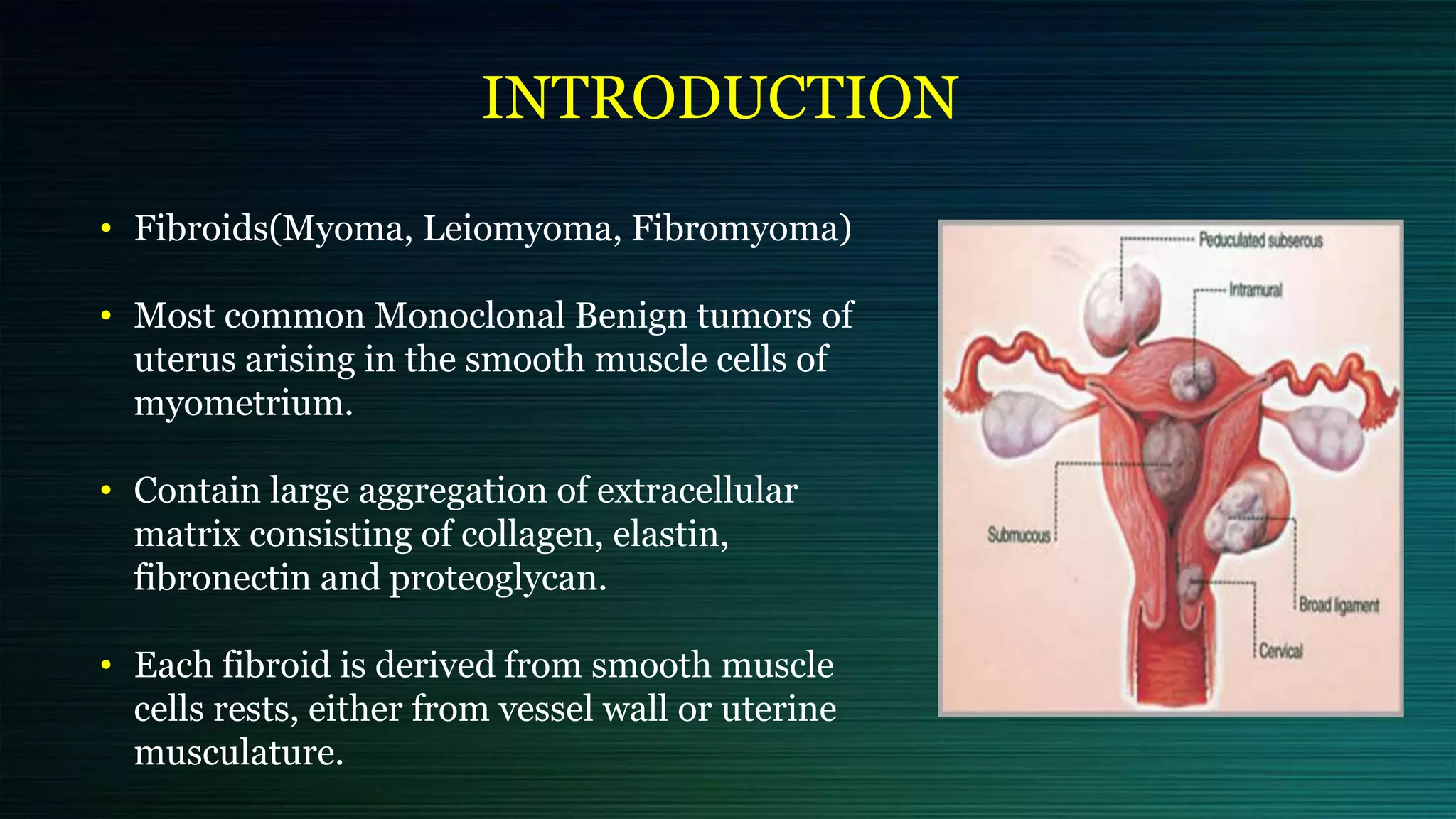
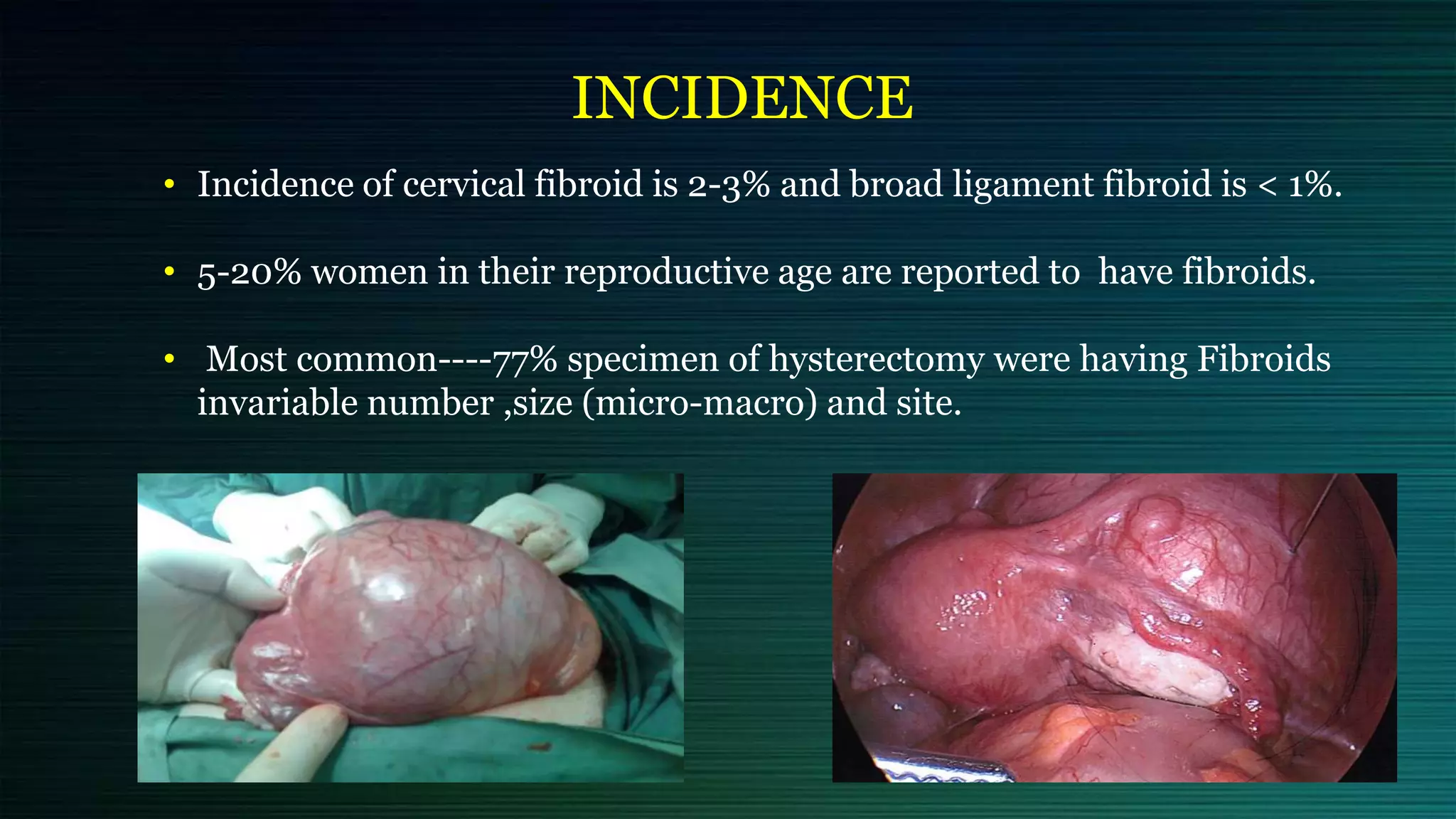
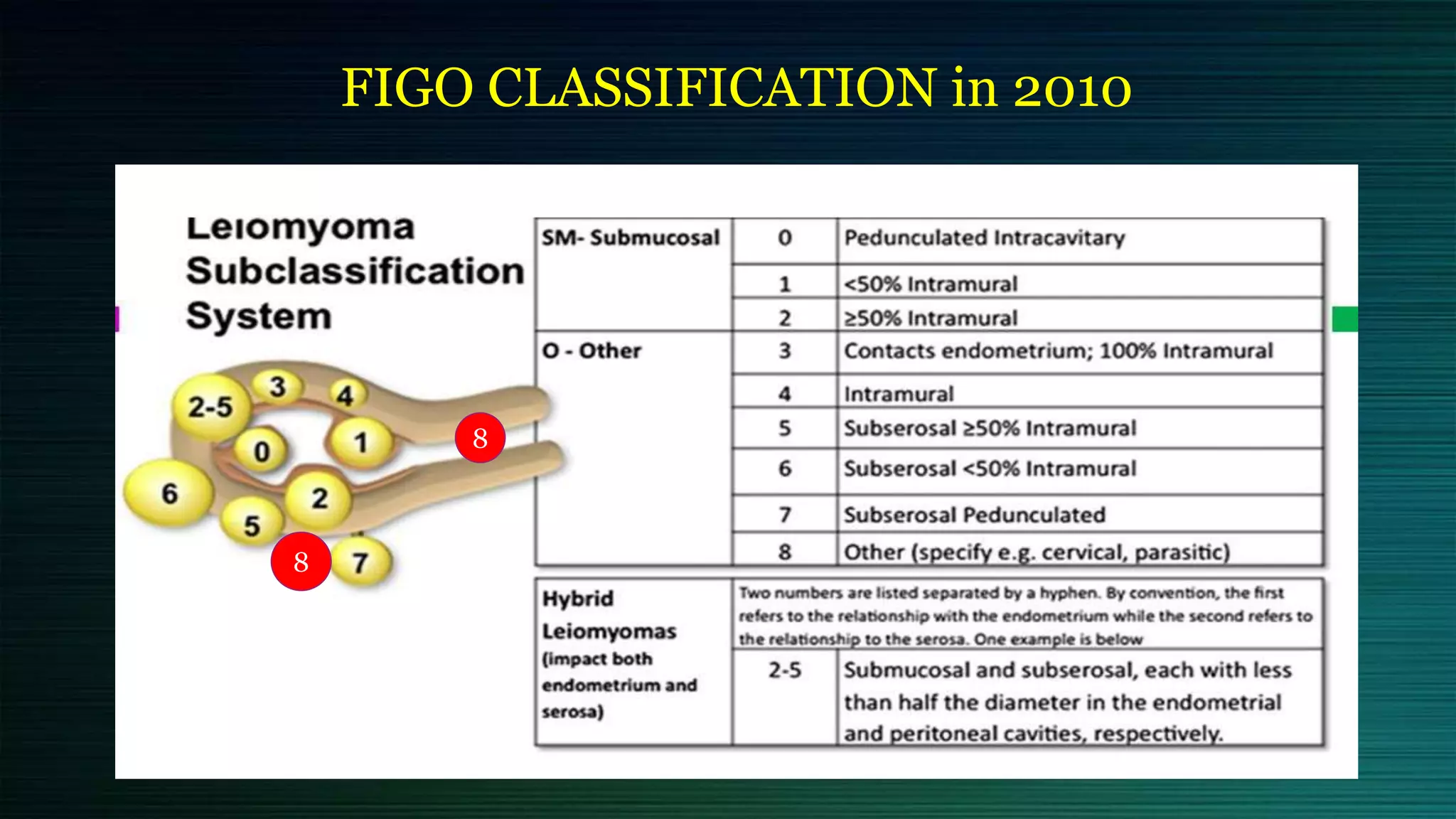
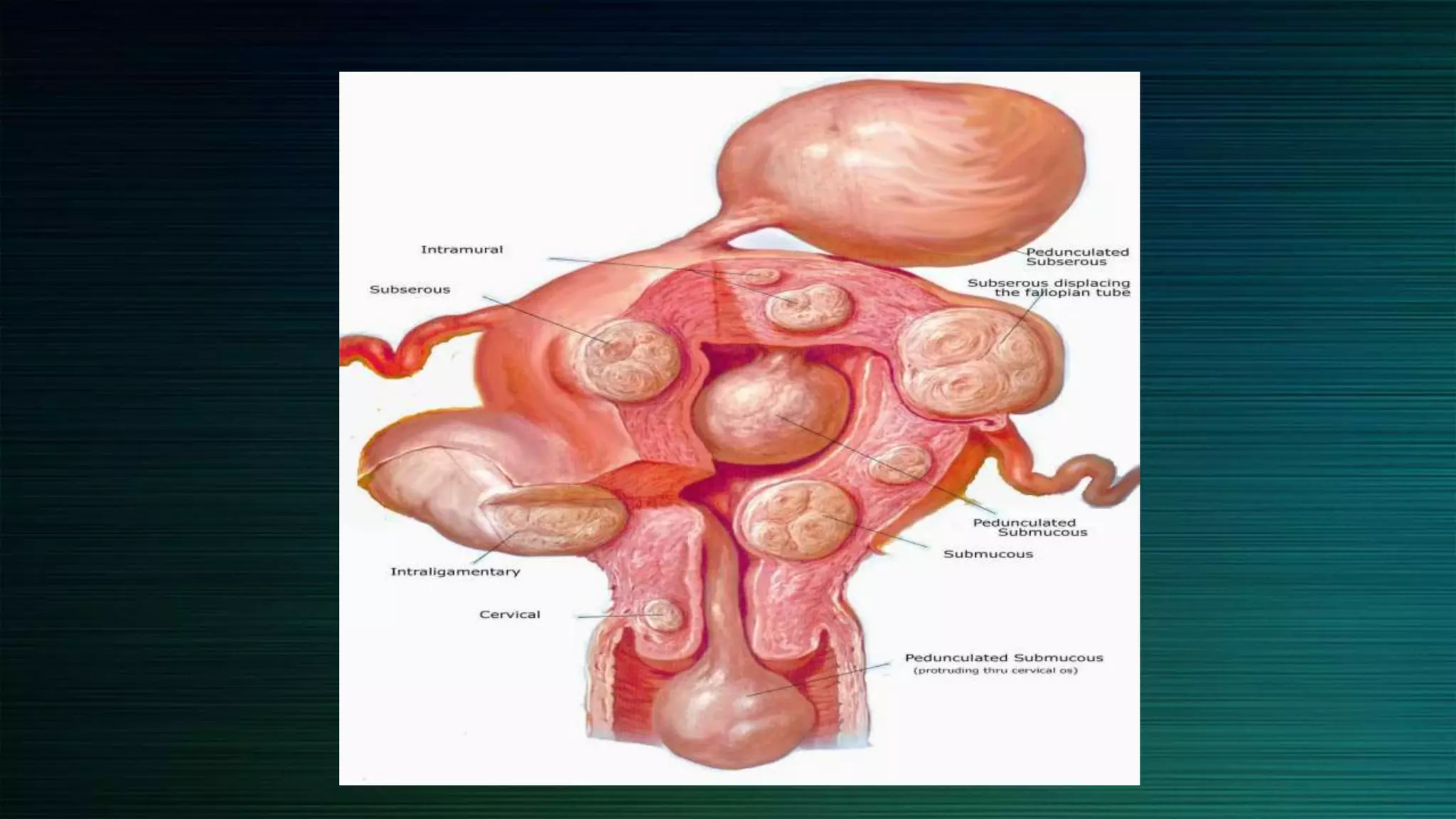
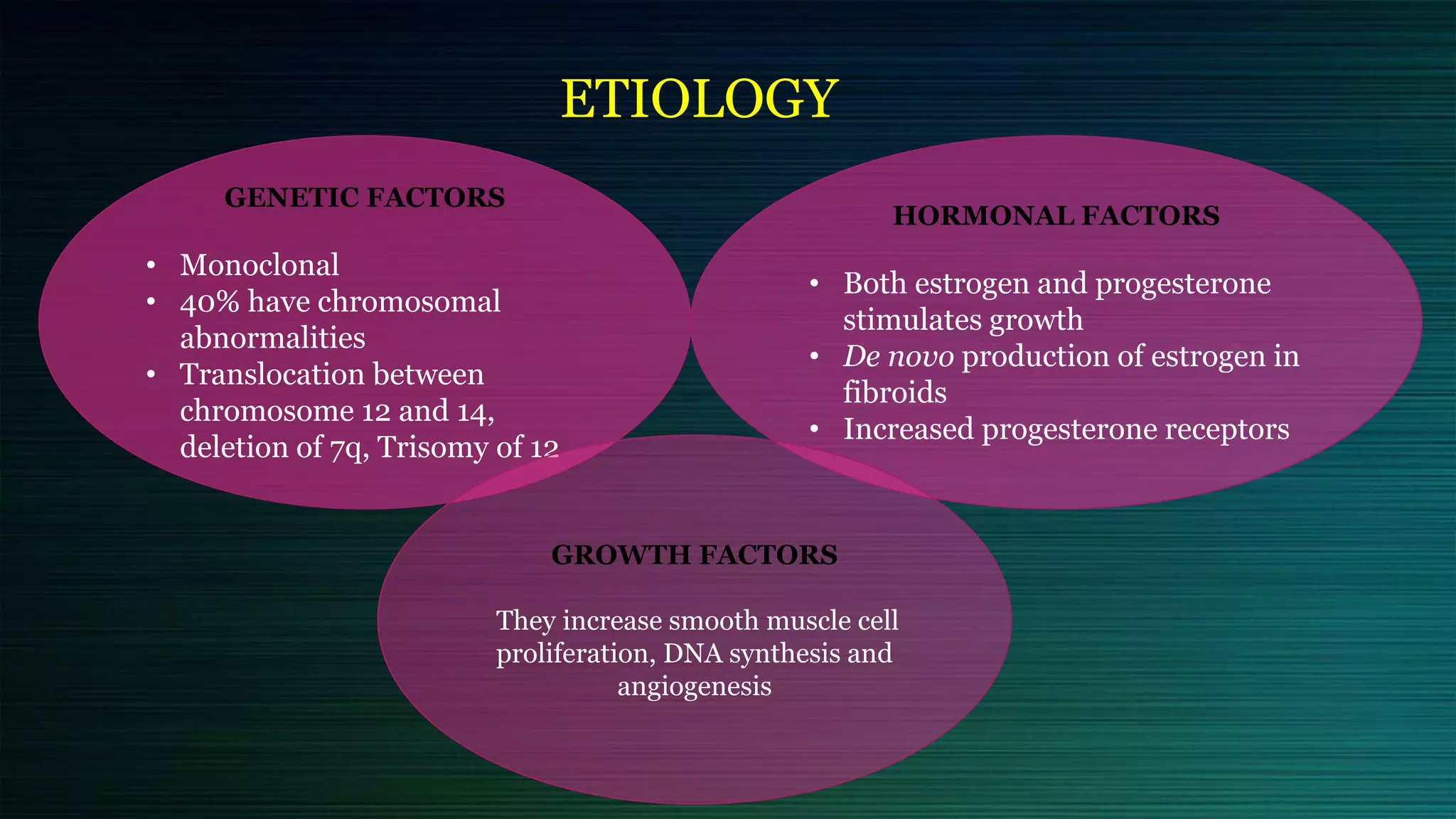
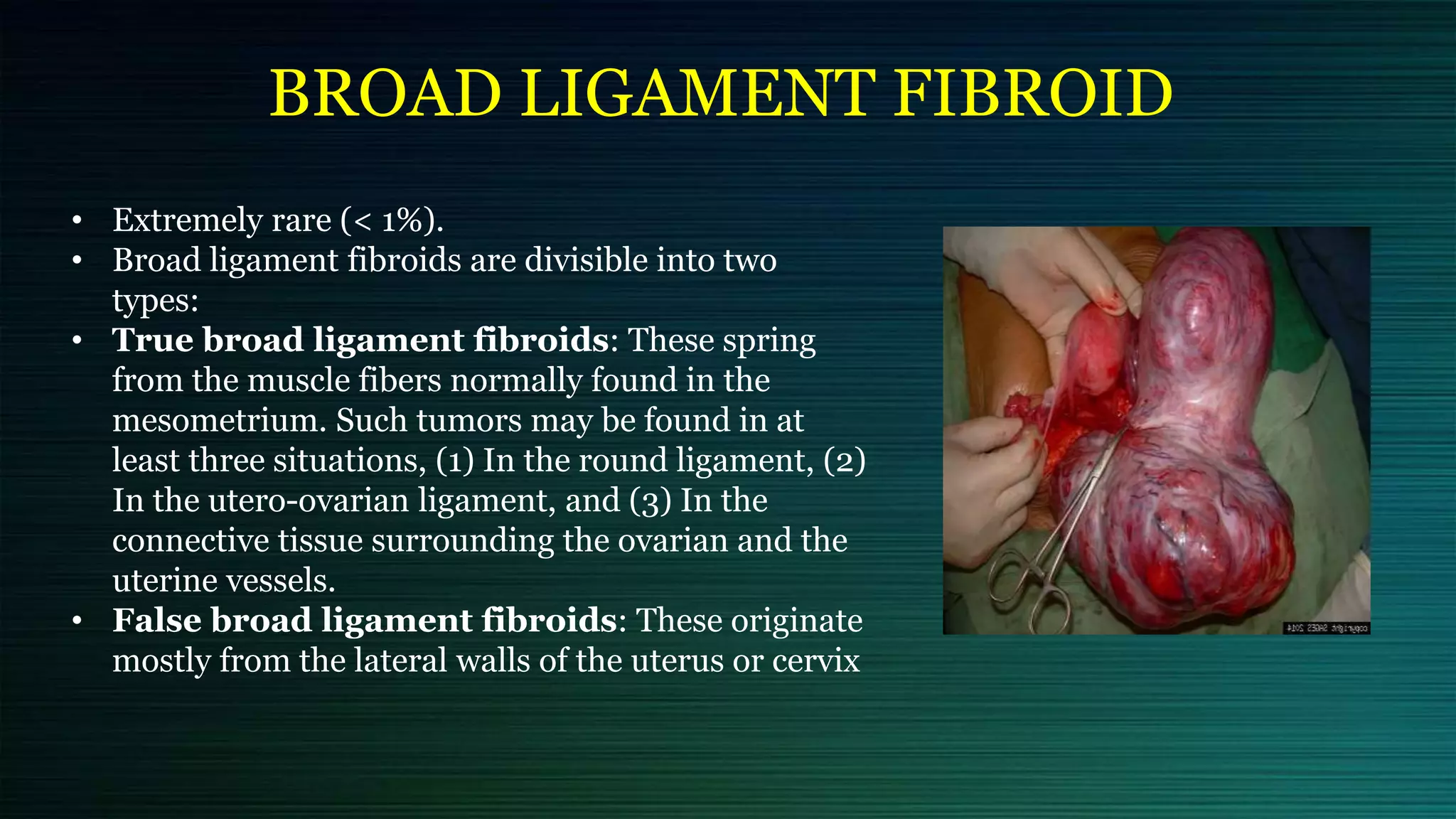
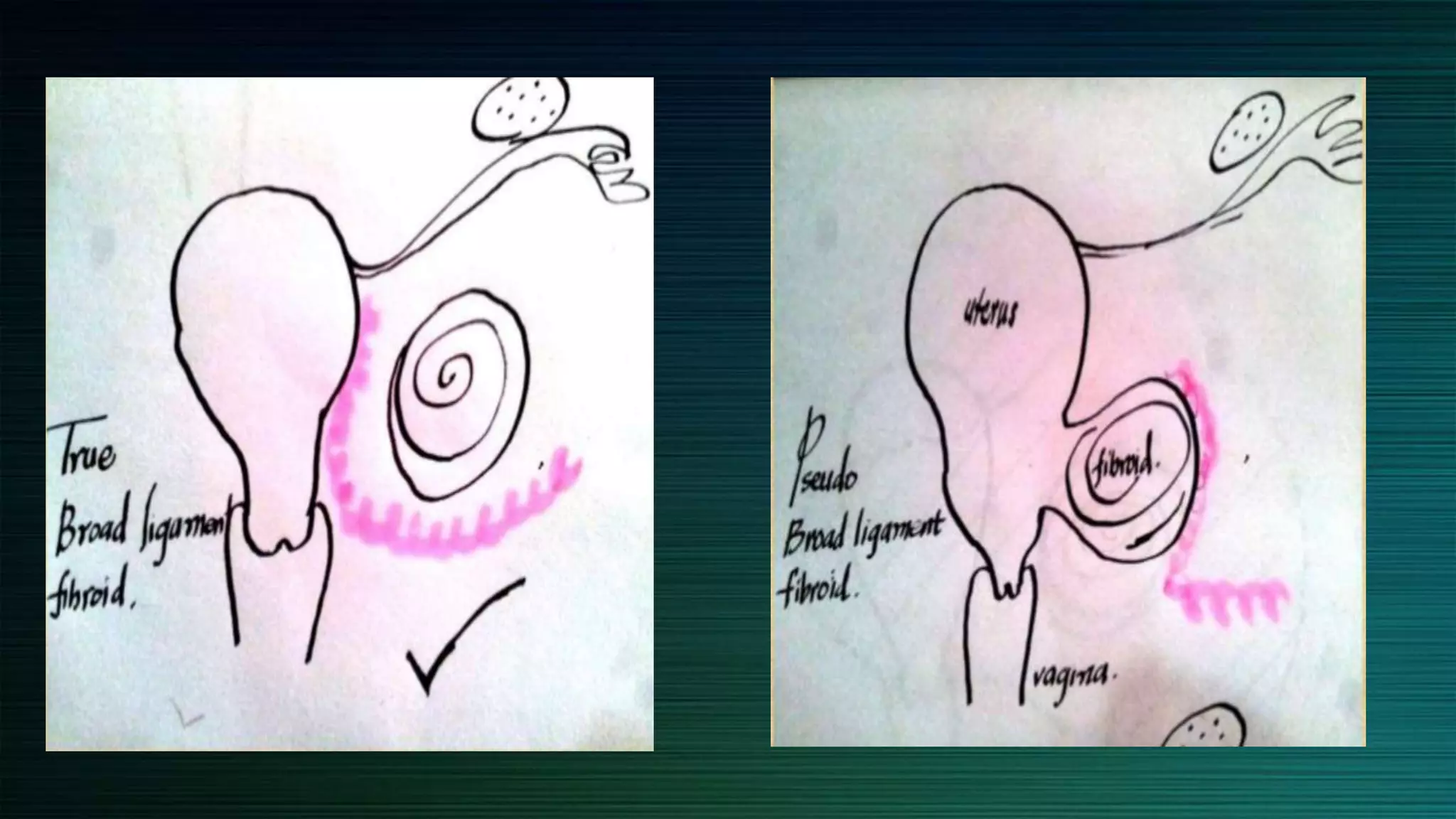
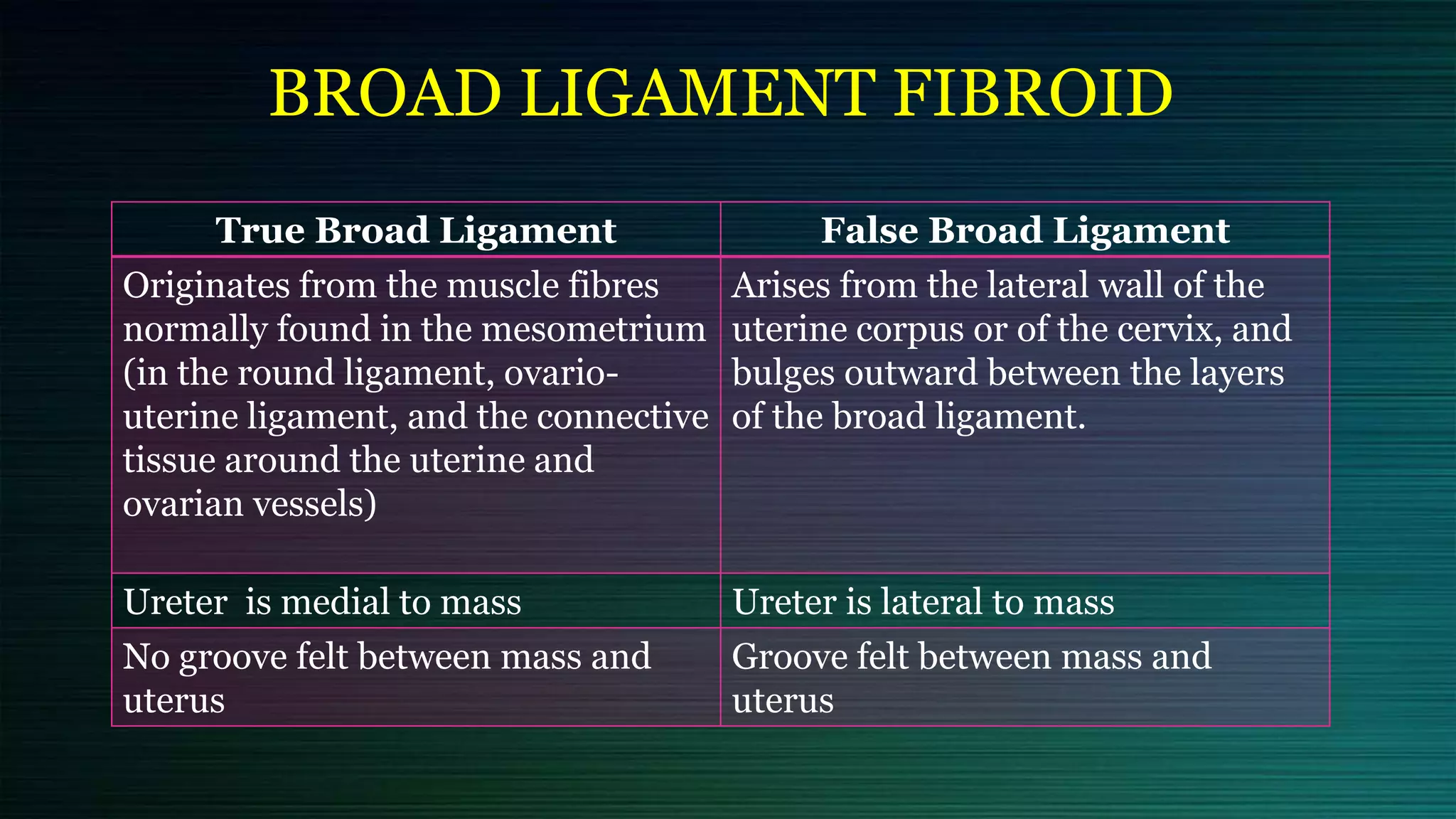
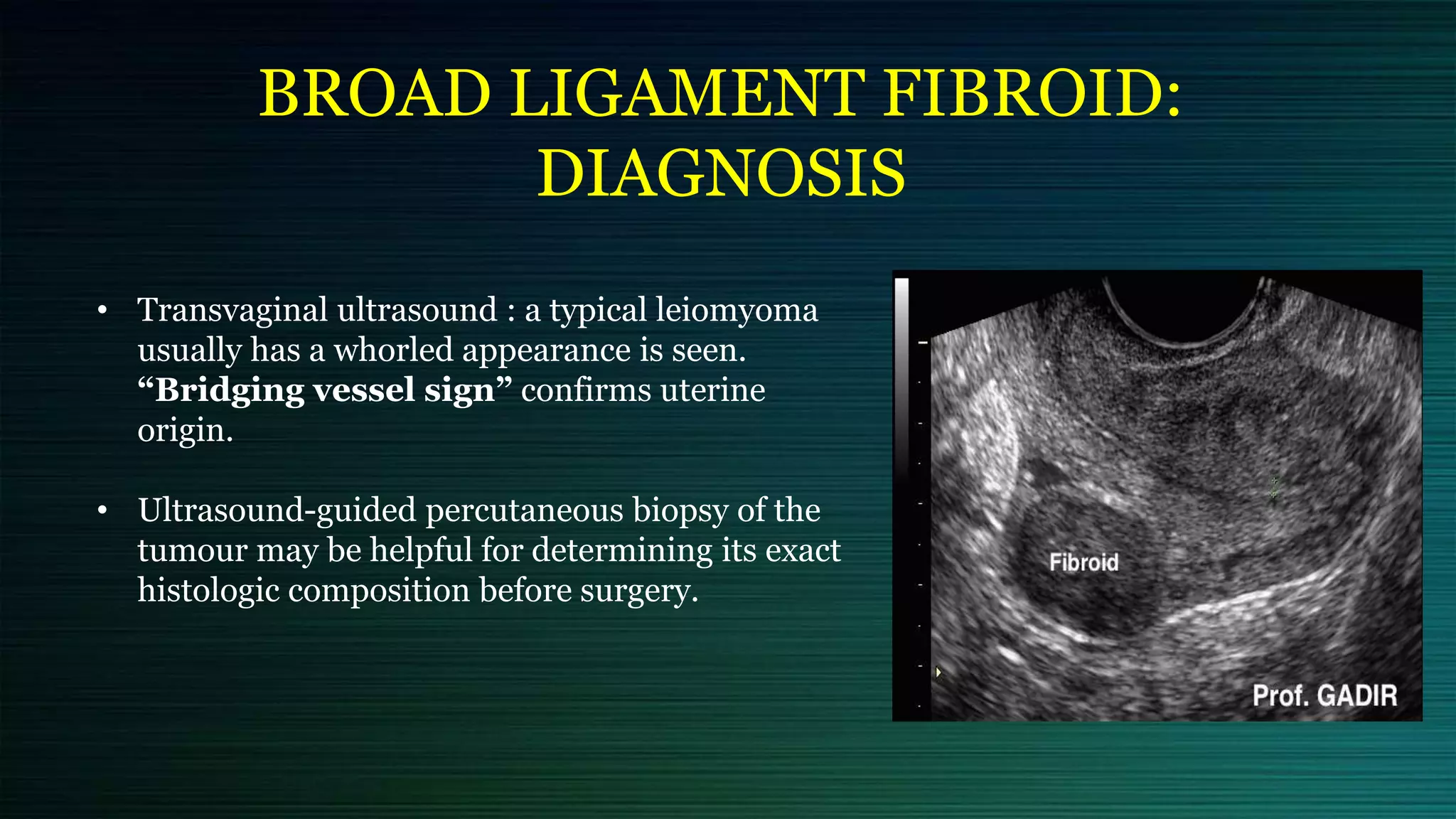
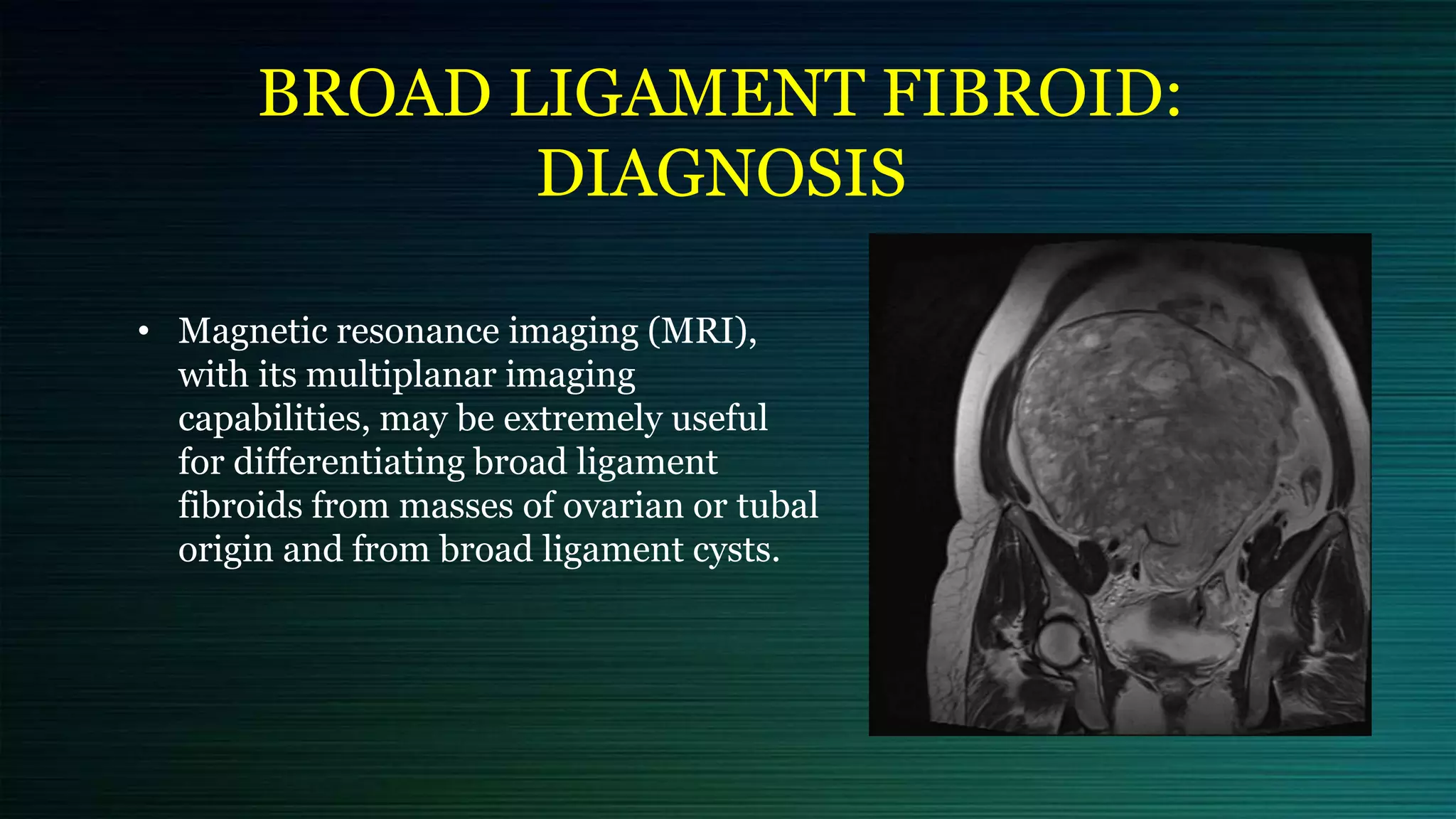
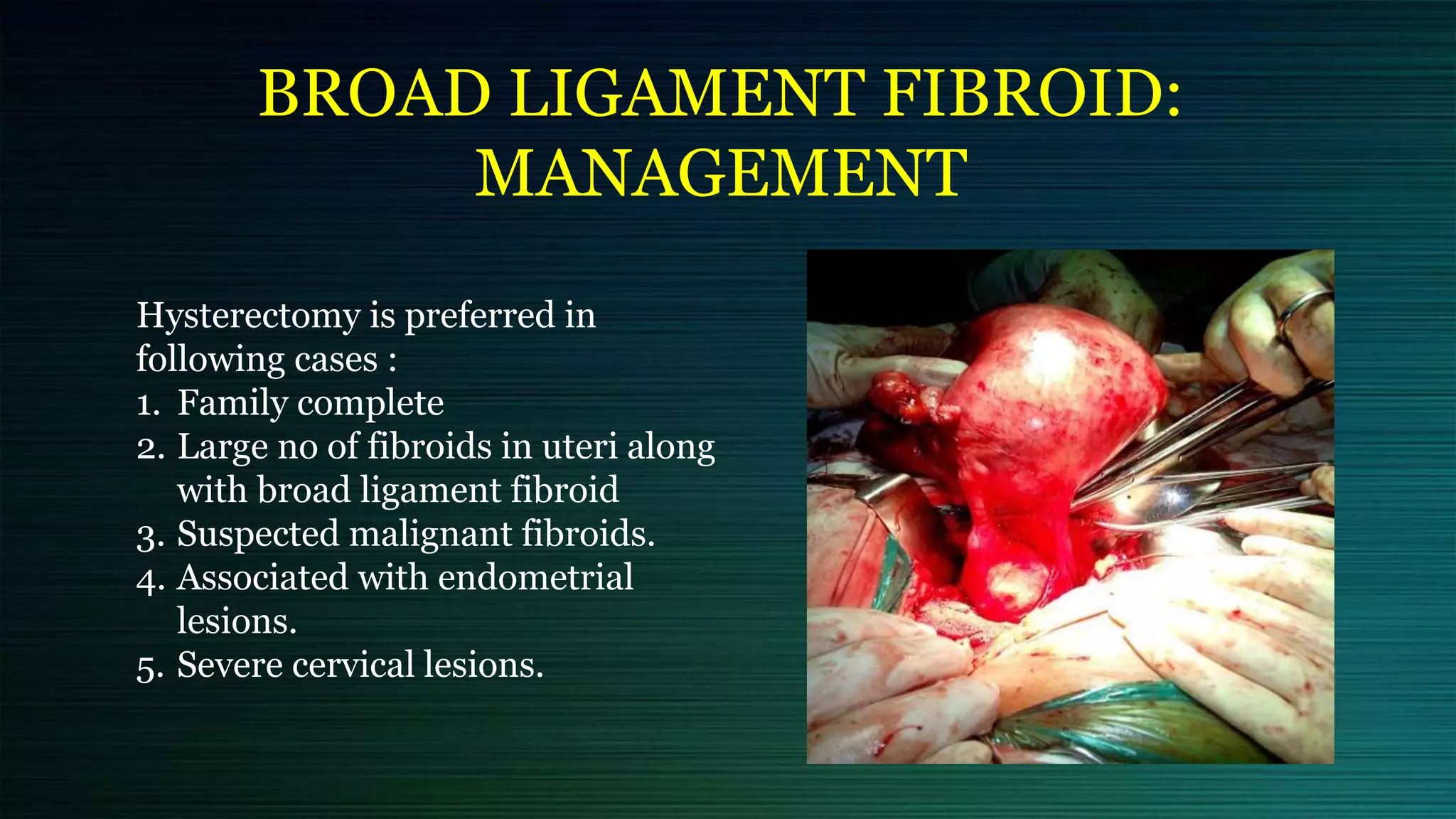
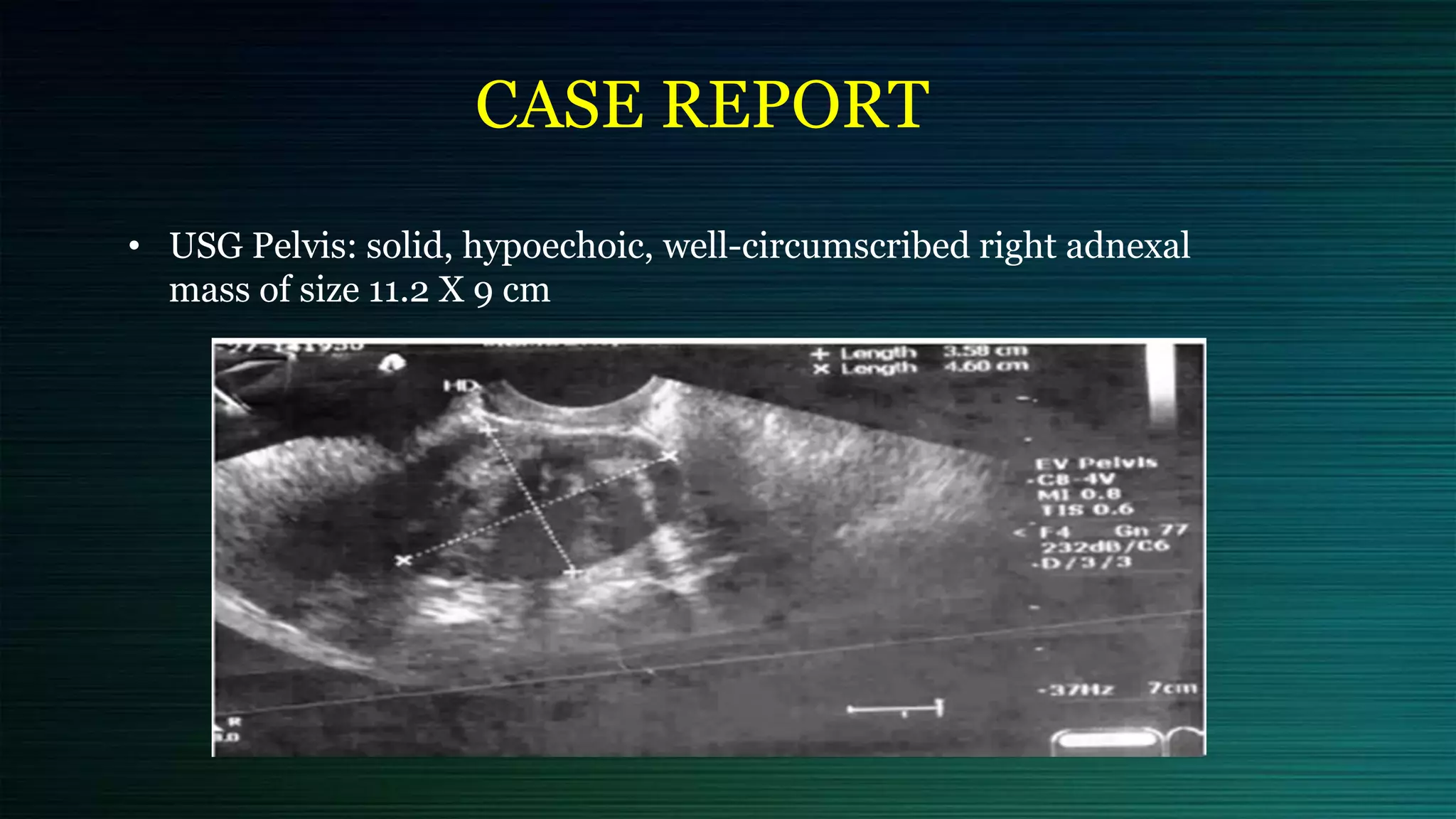
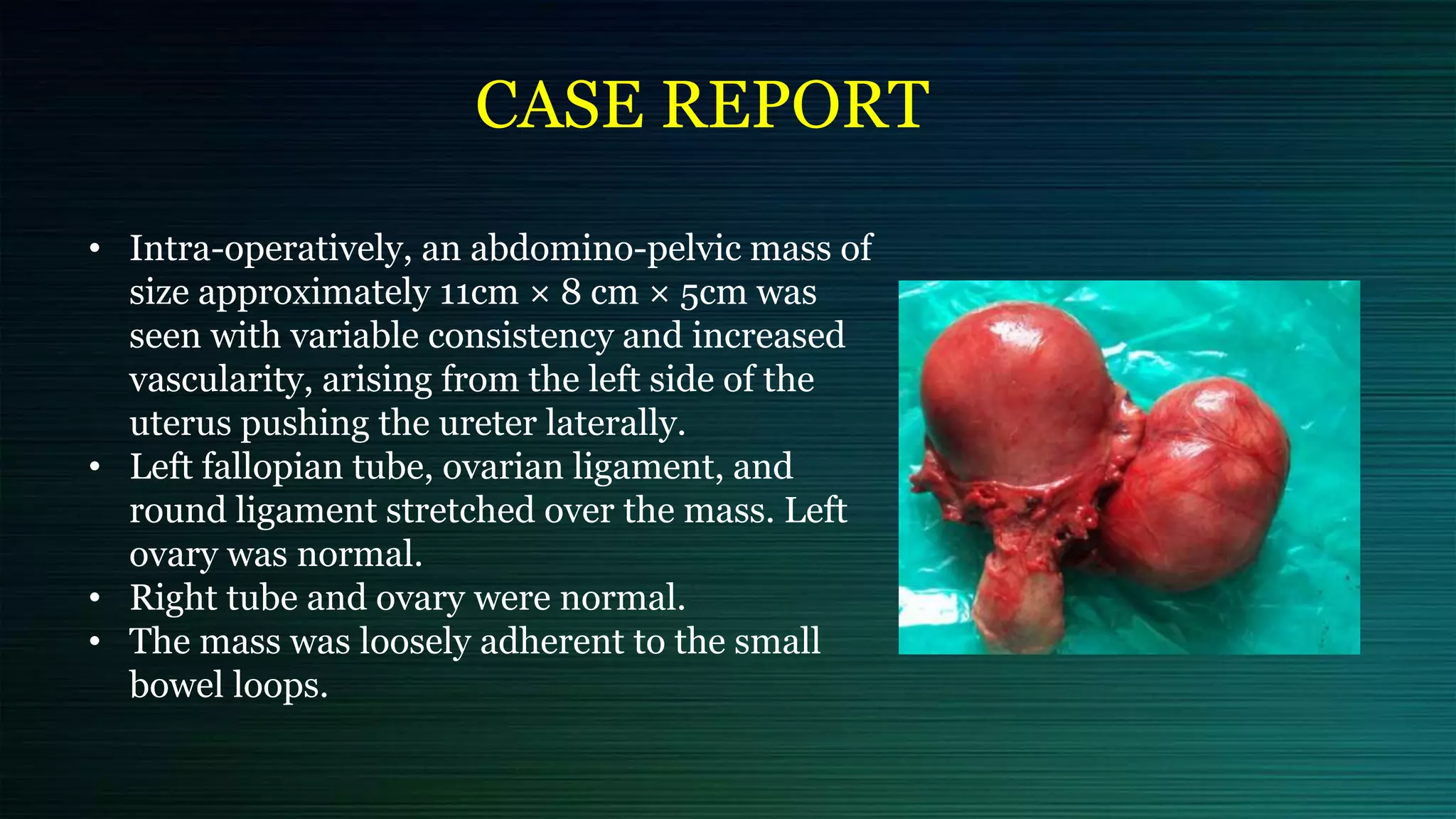
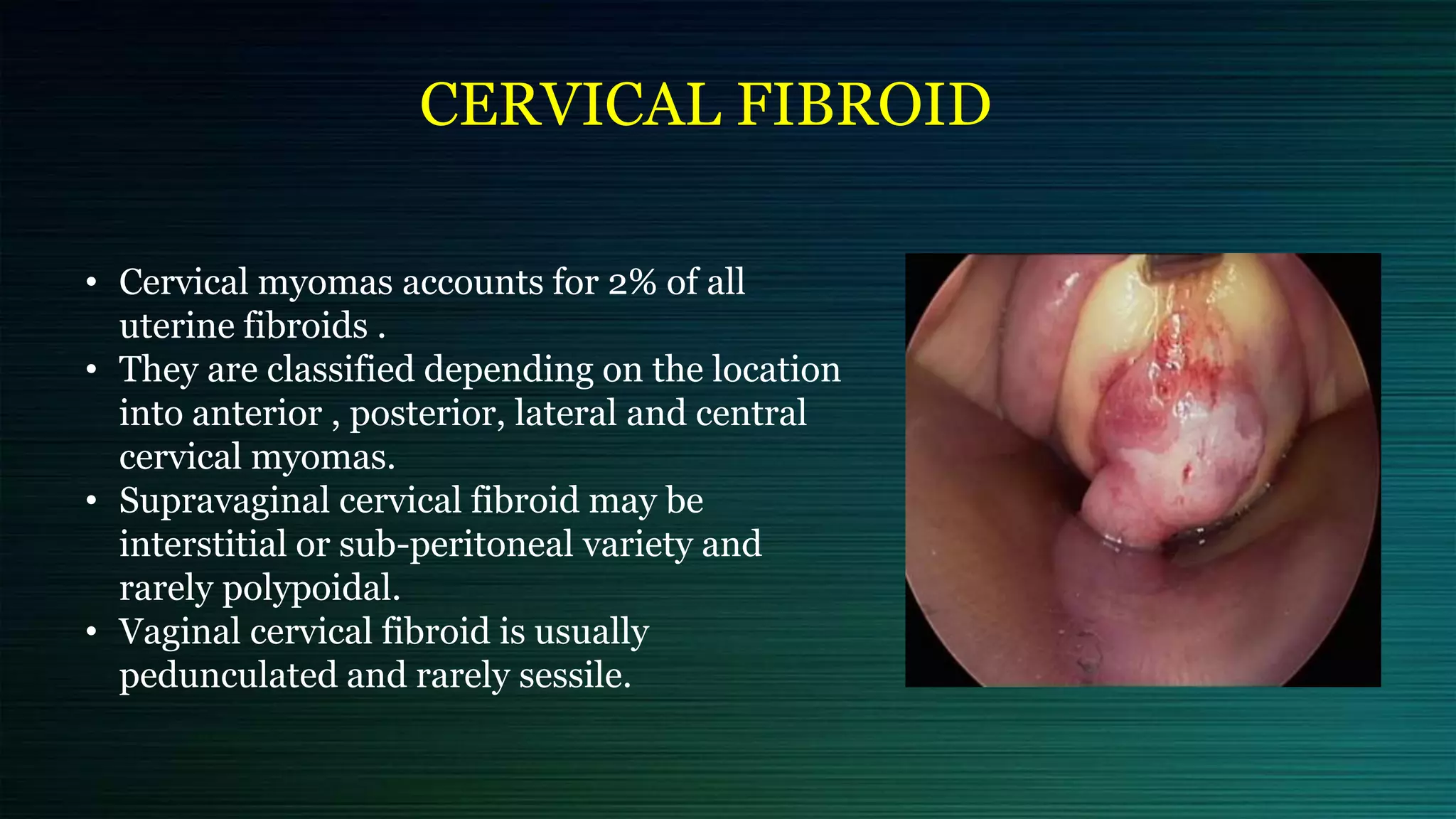
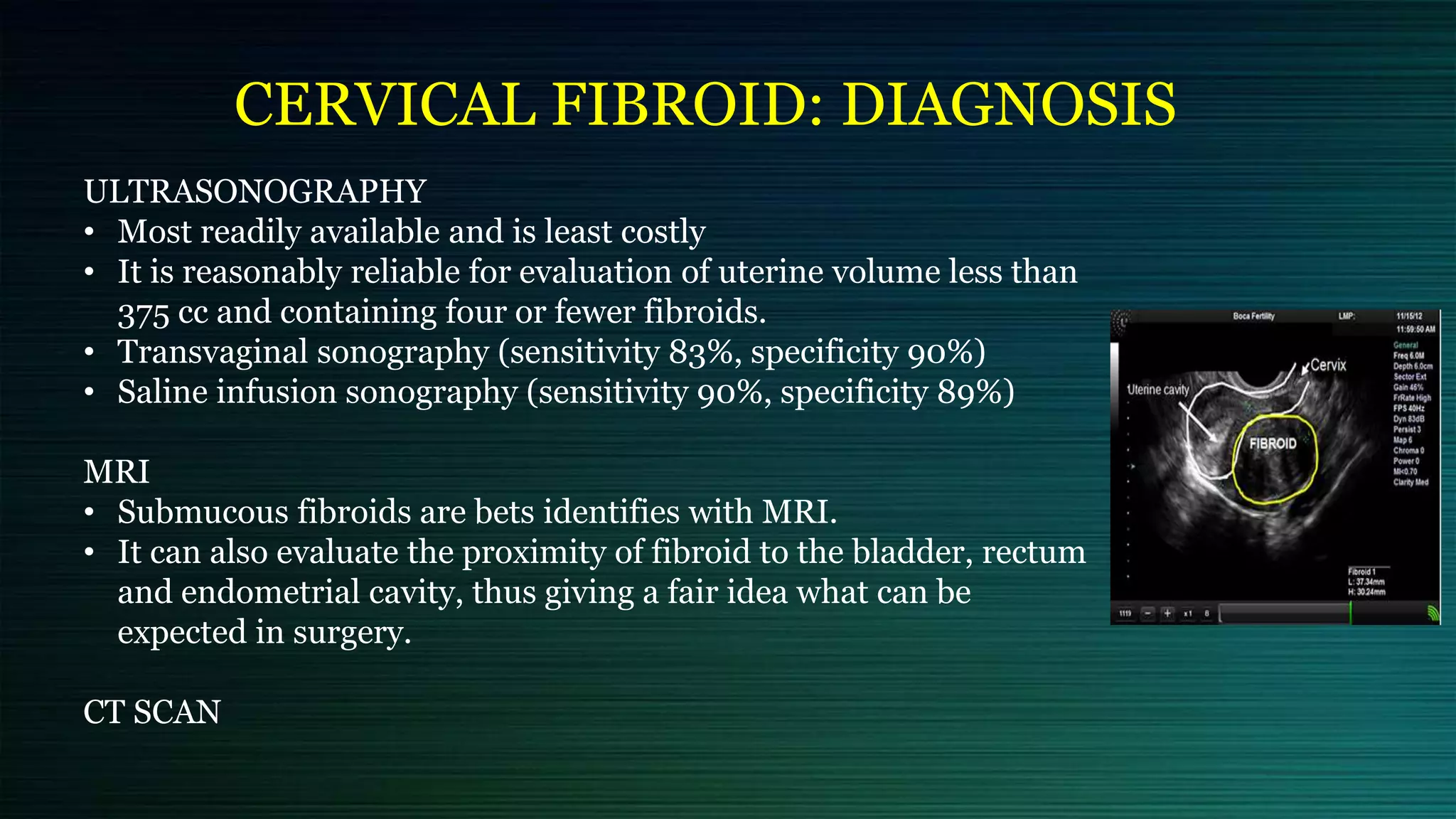
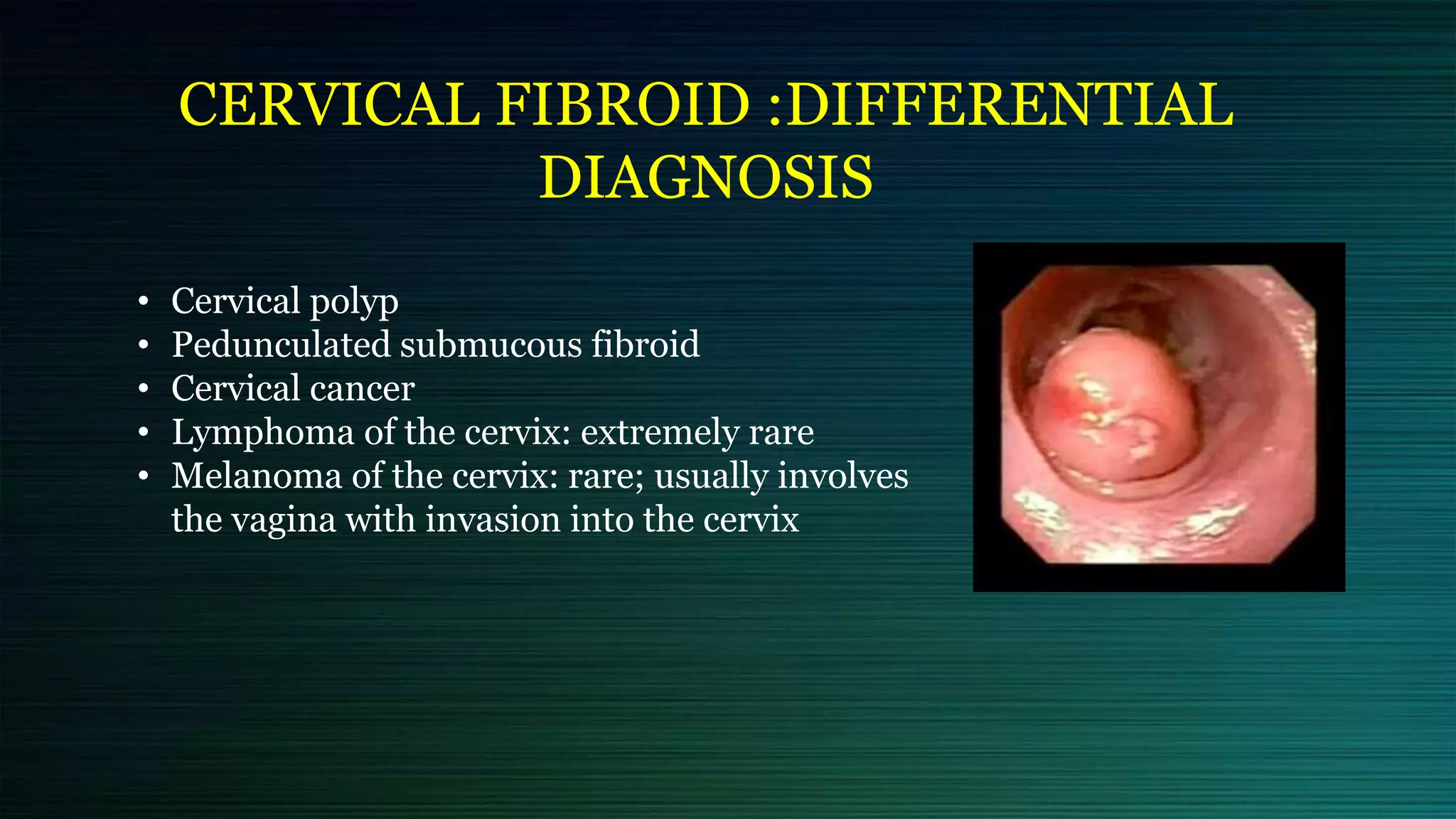
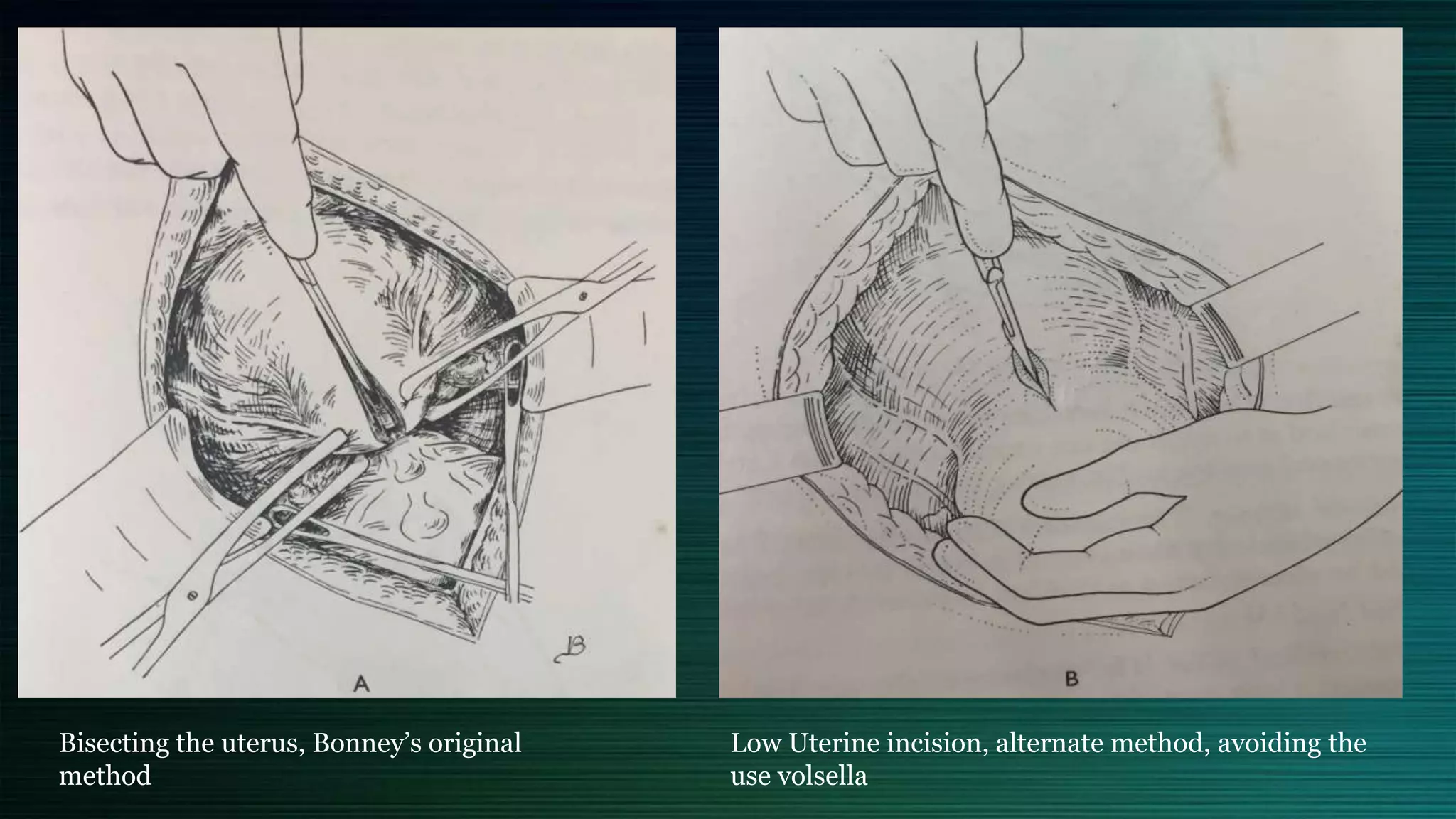
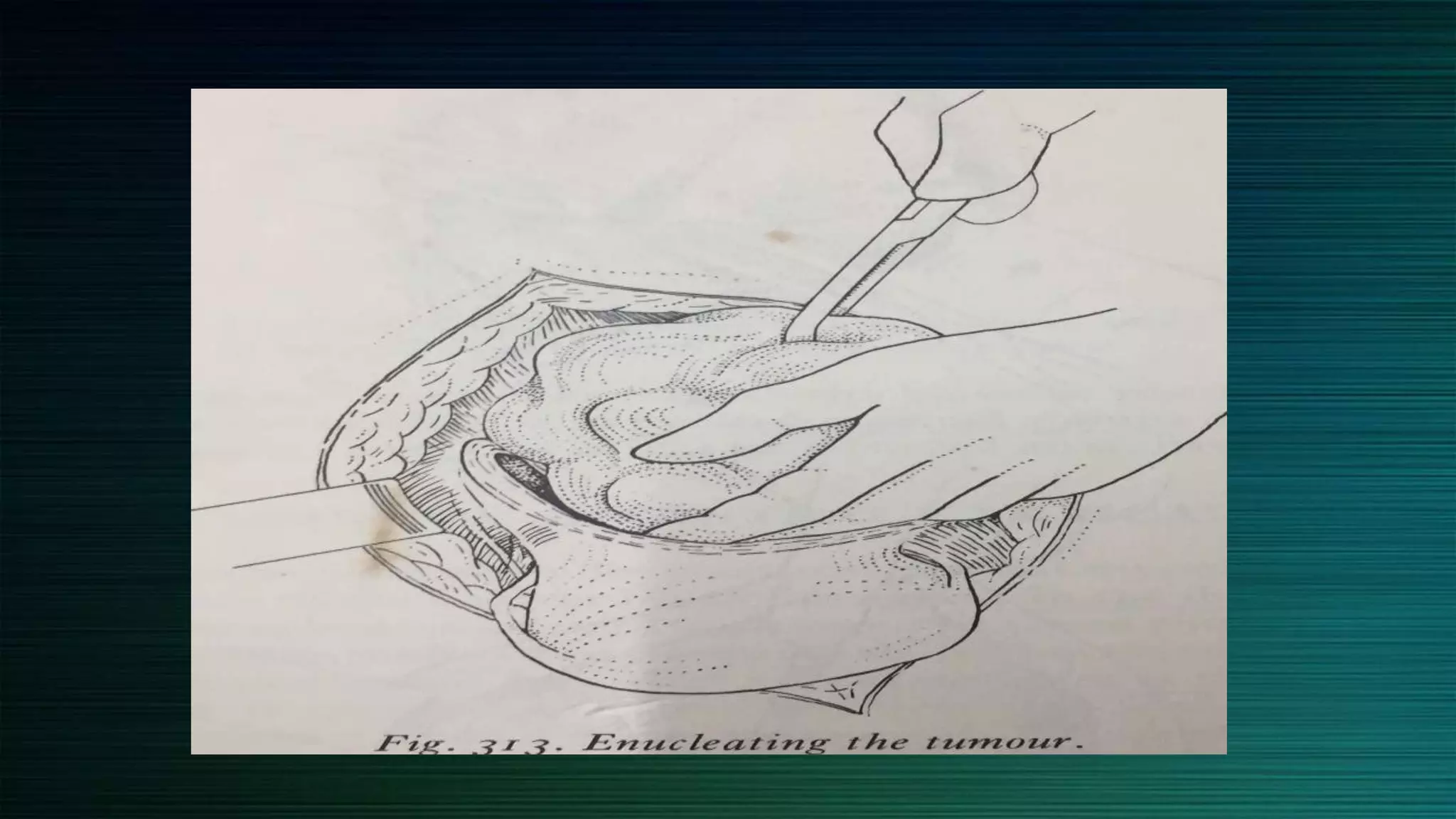
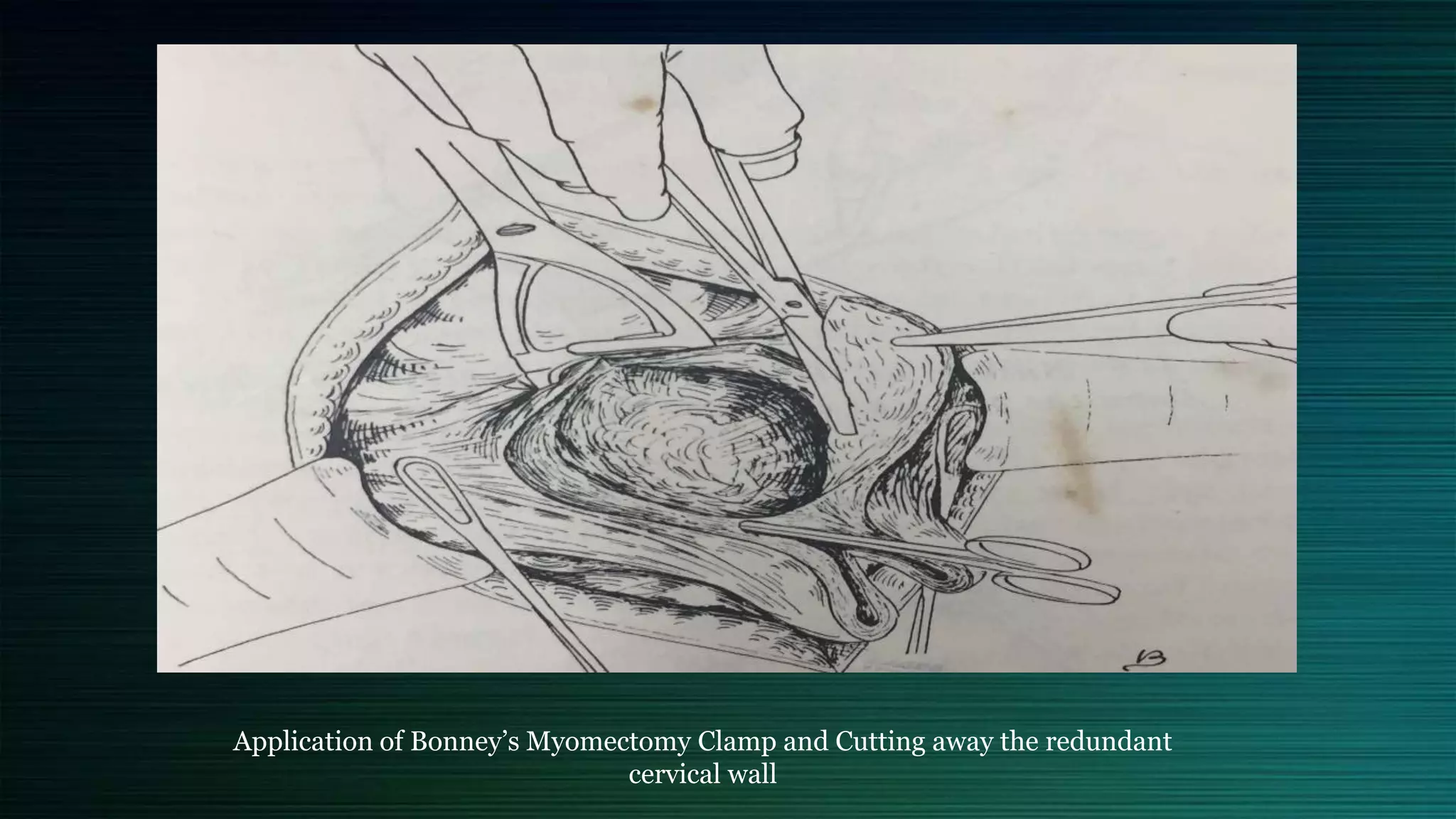
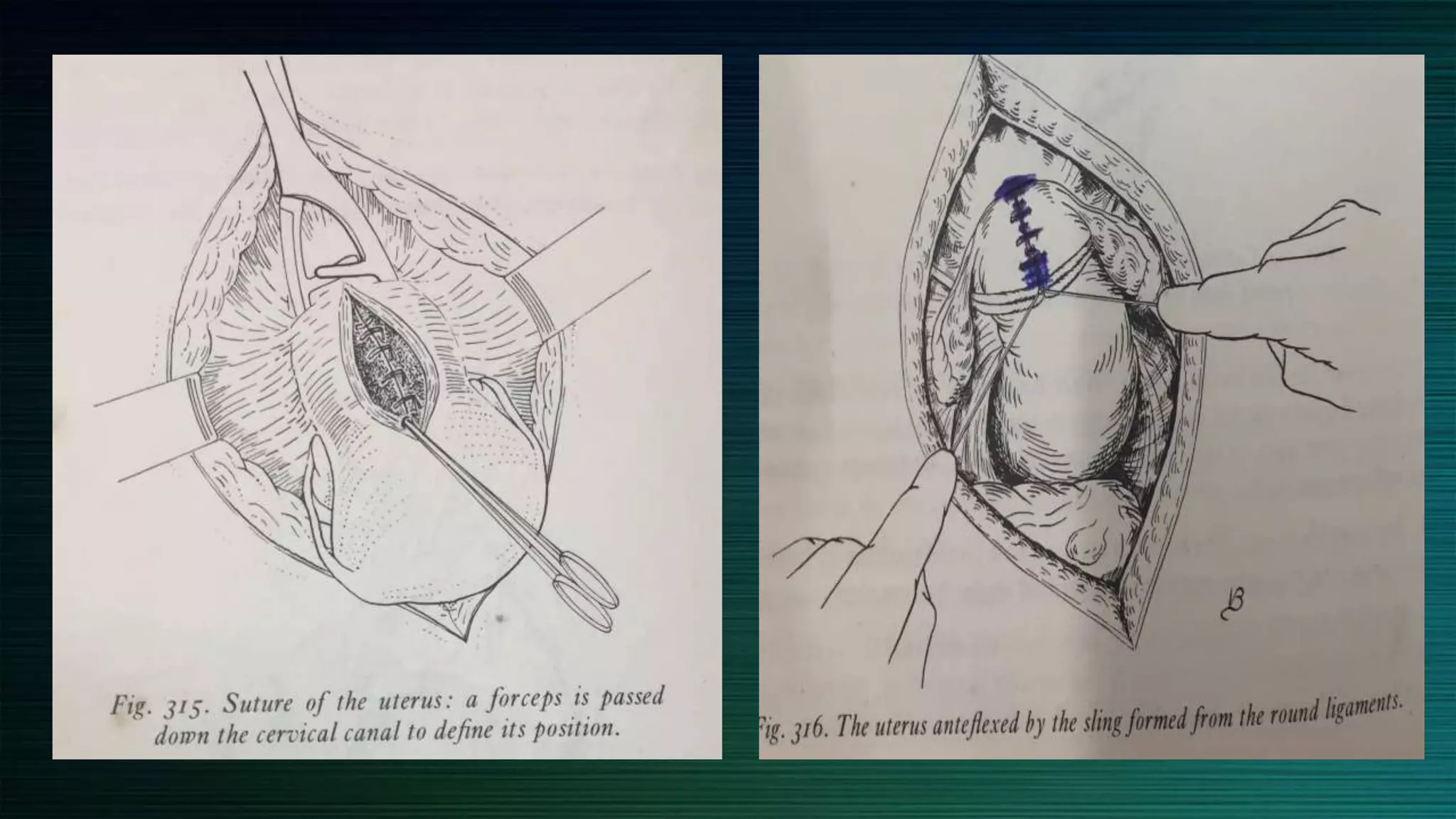
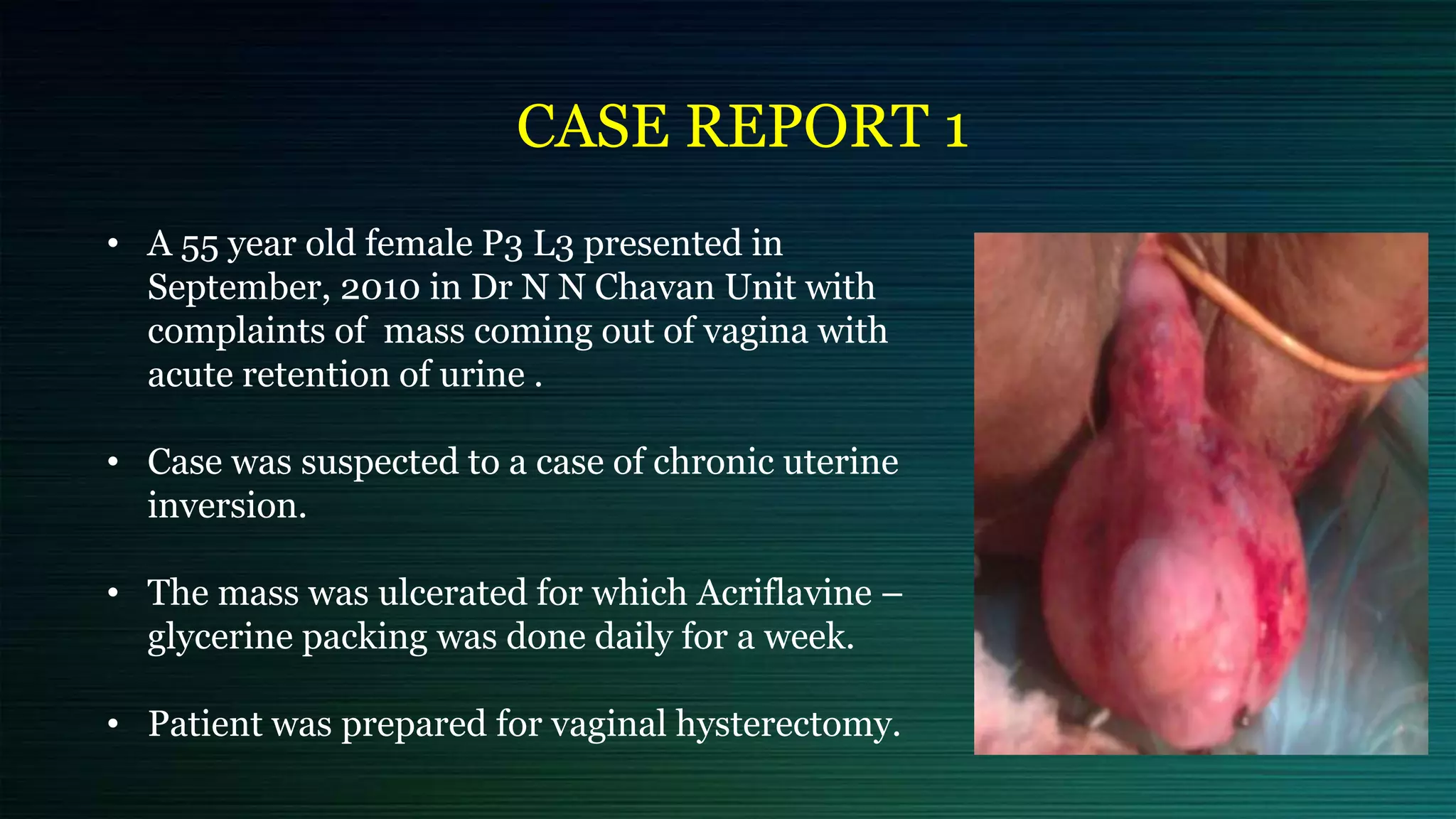
This document discusses cervical and broad ligament fibroids, which are rare types of benign tumors with an incidence of 2% and < 1%, respectively. It outlines their etiology, symptoms, diagnostic methods, differential diagnoses, complications, and management options such as myomectomy and hysterectomy, emphasizing the importance of considering the patient's fertility desires and the fibroid's characteristics when determining treatment. Additionally, the document presents case reports to illustrate the complexities involved in diagnosing and treating these fibroids.