This document discusses pelvic organ prolapse, including:
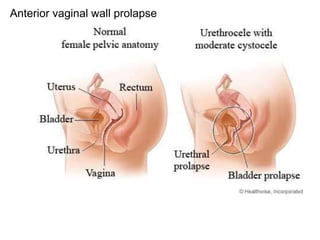
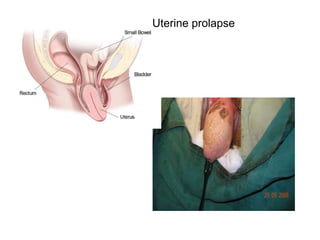
- A case scenario of a 43-year-old woman presenting with a mass descending from her vagina and difficulty initiating urination.
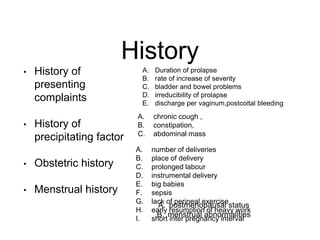
- Details to ask in the history, including obstetric history, menstruation history, bladder/bowel problems, and duration/progression of prolapse.
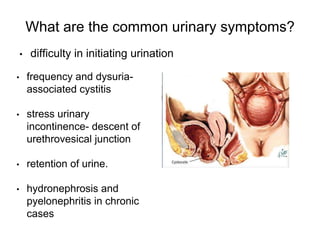
- Common urinary symptoms like frequency, dysuria, stress incontinence, and retention.
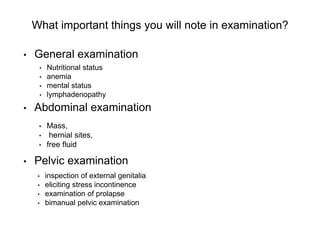
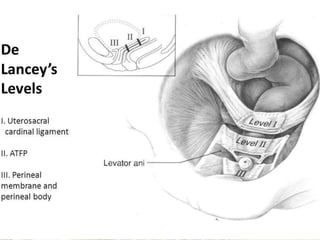
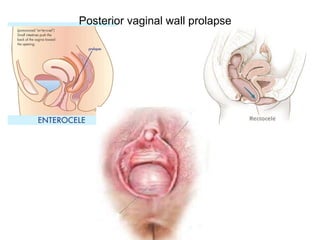
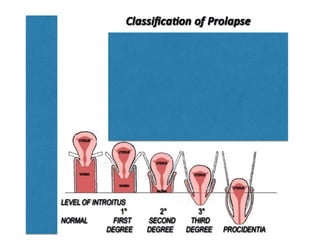
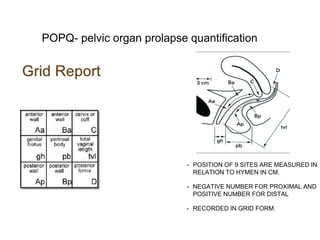
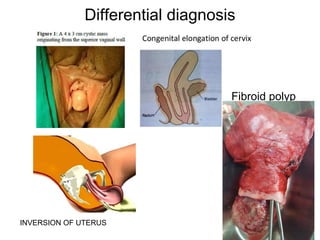
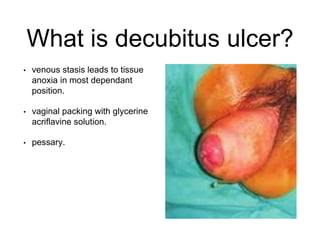
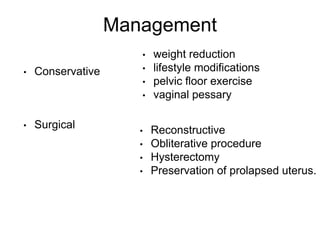
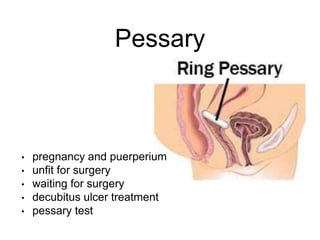
- Examination findings like prolapse classification systems, differential diagnosis, and management options like conservative treatments, reconstructive surgery, obliterative procedures, and hysterectomy.
![Preservation of Prolapsed uterus
• FOTHERGILL/MANCHESTER
A. amputation of cervix
B. cardinal ligaments cut and
fixed anteriorly to cervix
C. anterior colporrhaphy
D. if required post
colpoperineorrhaphy
• SLING SURGERIES
[nulliparous prolapse]](https://image.slidesharecdn.com/prolapseclass-160714061050/85/Prolapse-1-25-320.jpg)
