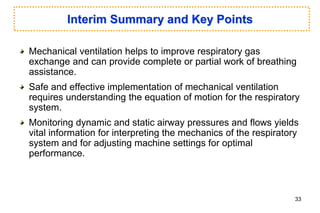
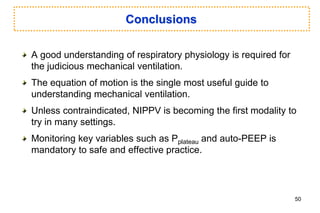
This document discusses mechanical ventilation, including:
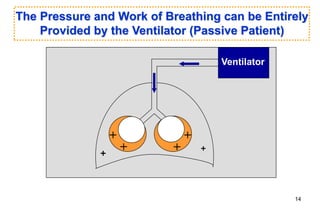
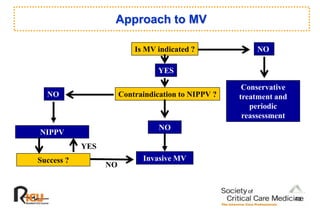
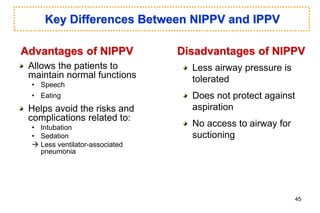
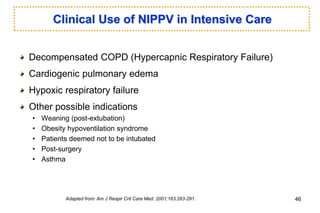
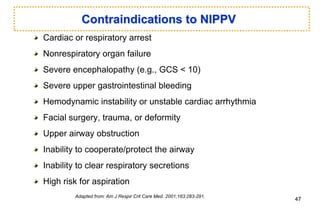
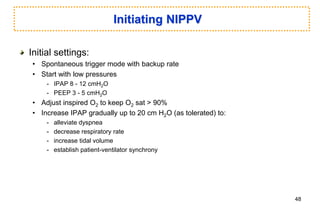
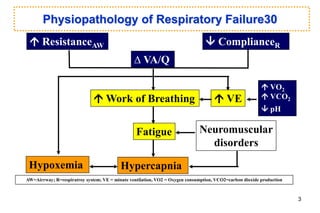
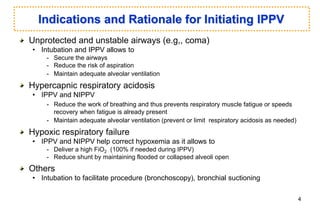
1) The basics of invasive positive pressure ventilation (IPPV) and noninvasive positive pressure ventilation (NIPPV) and how they help reduce work of breathing and restore gas exchange.
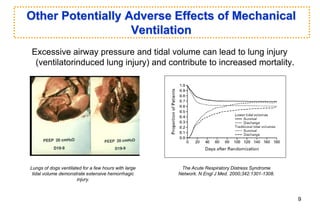
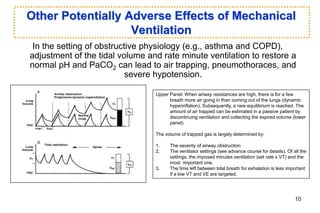
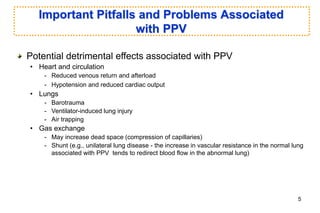
2) Important considerations for initiating IPPV including indications like respiratory failure and risks like hypotension and lung injury.
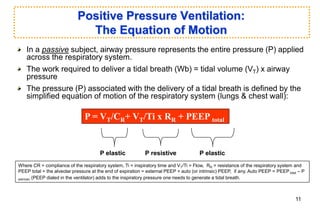
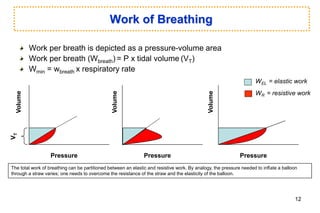
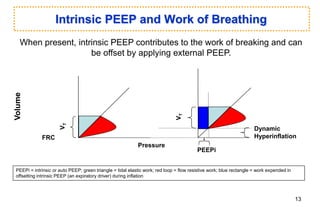
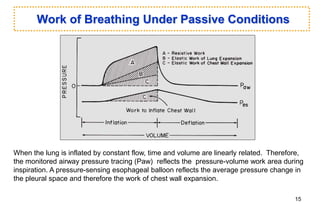
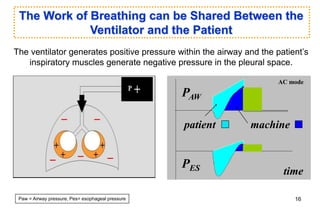
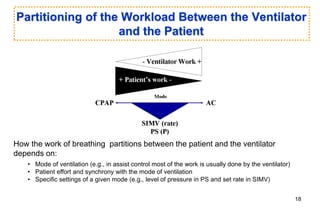
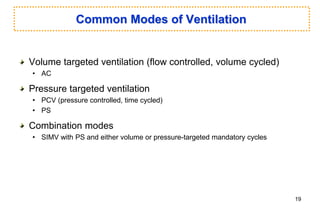
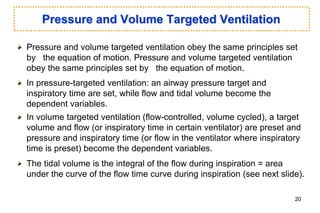
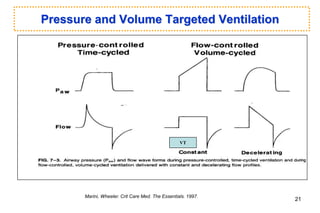
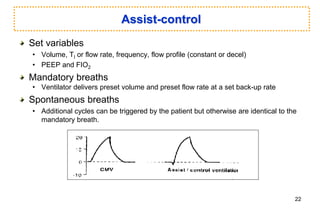
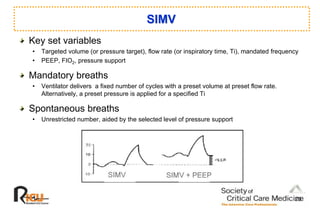
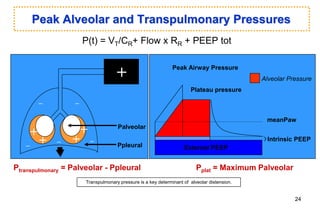
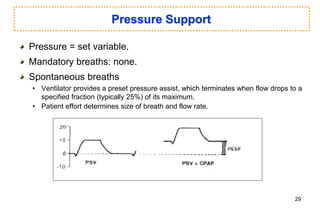
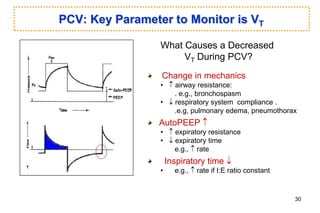
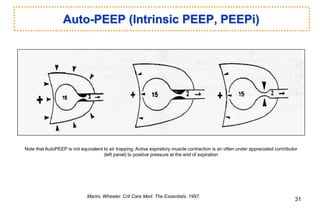
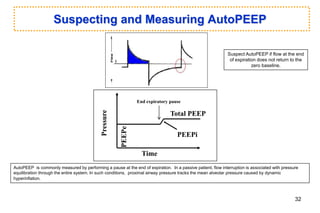
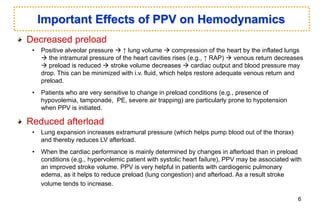
3) Key principles of mechanical ventilation including the equation of motion, partitioning work between the ventilator and patient, and common modes of ventilation.

![Alveolar Pressure and Gas Exchange
Intensity
of
the
effects
Alveolar Pressure
PaO2
Dead space
Oxygen transport
Adapted from: Marini, et al. Crit Care Med. 1992.
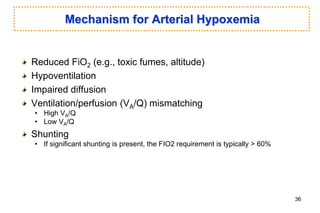
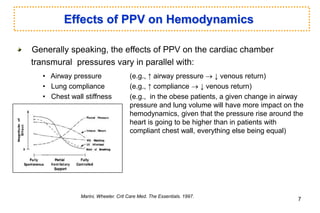
Note that as airway pressure increases above a certain level (e.g., high
PEEP [positive end-expiratory pressure]):
• Oxygen transport start to decline despite the rising PaO2 as cardiac output starts falling.
• Dead space also tends to increase due to compression of alveolar capillaries by high alveolar
pressure, creating ventilated but poorly perfused alveolar units.
8](https://image.slidesharecdn.com/ventilatoromar2016-220809033137-27aa7c0c/85/ventilator_Omar_2016-ppt-8-320.jpg)