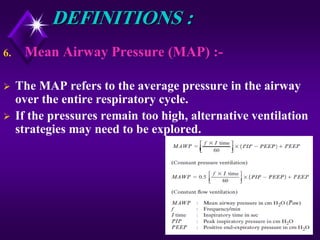
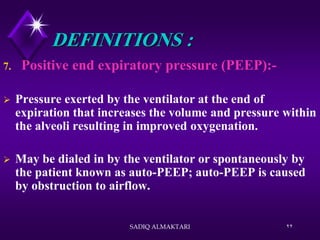
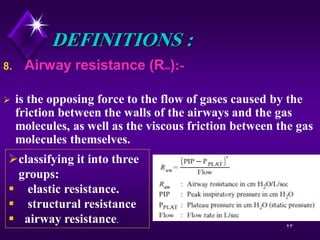
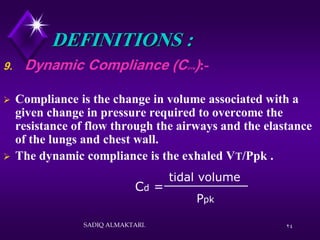
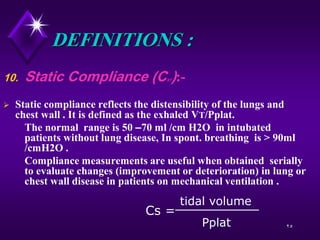
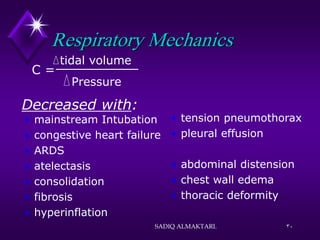
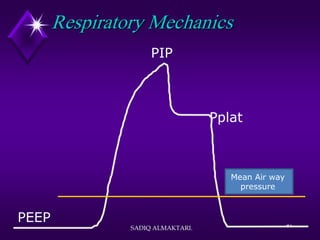
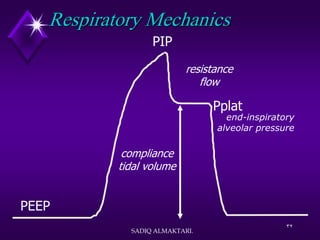
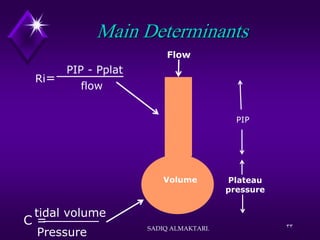
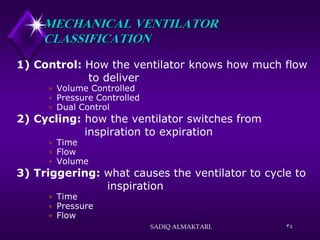
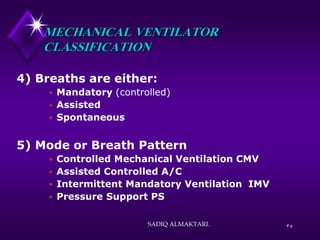
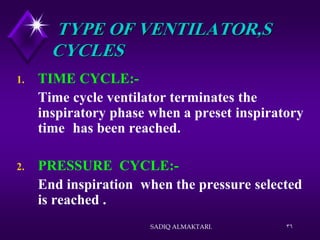
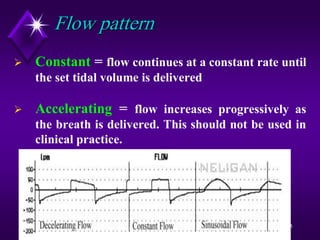
The document by Sadiq Almaktari outlines essential concepts in respiratory therapy, focusing on gas flow and pressure gradients during ventilation. It defines key pressures such as airway opening pressure, intrapleural pressure, and various pressure gradients crucial for understanding normal ventilation mechanics. Additionally, it discusses the different types of mechanical ventilators and the factors influencing their functions, including cycle and trigger settings.