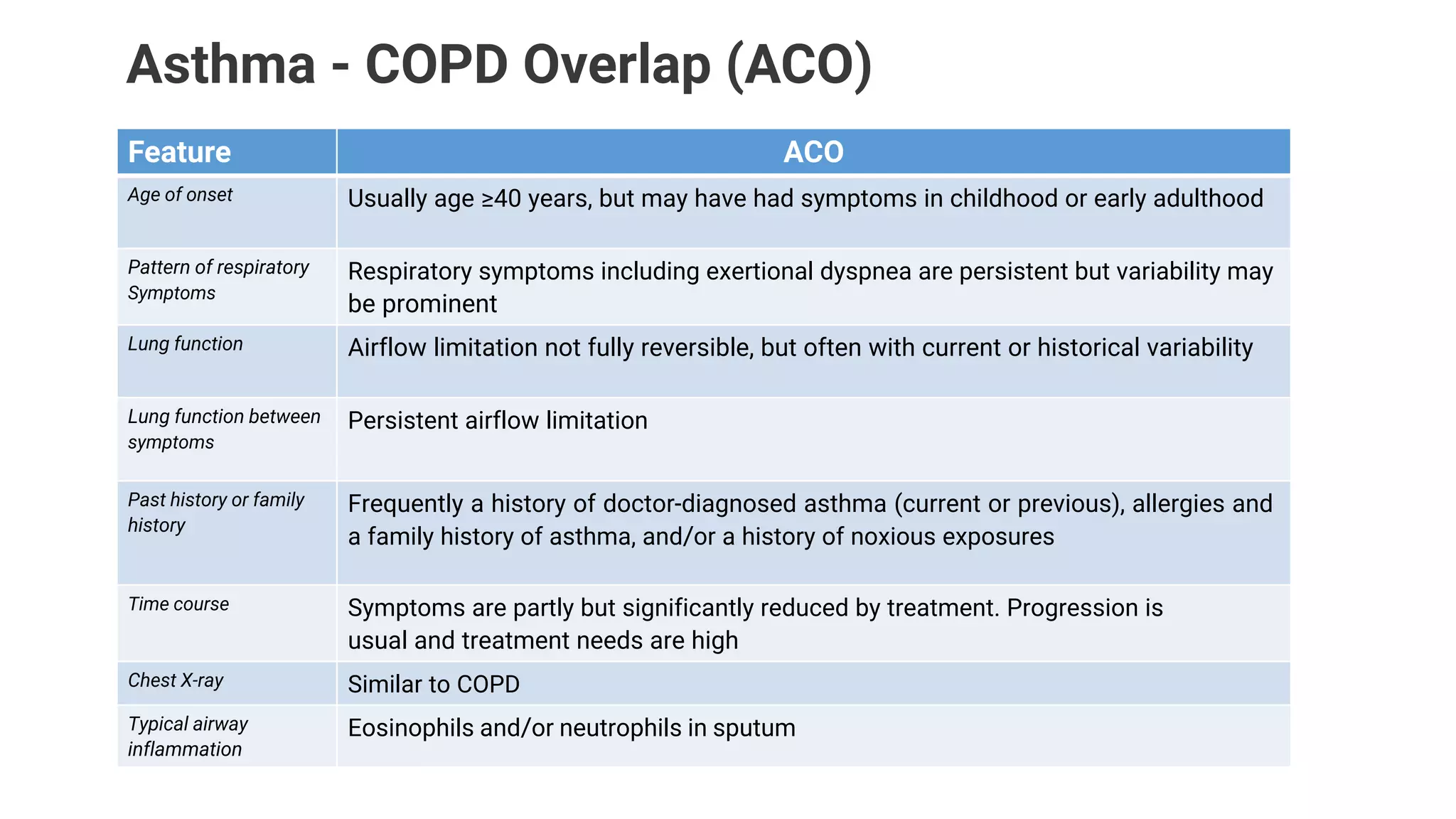
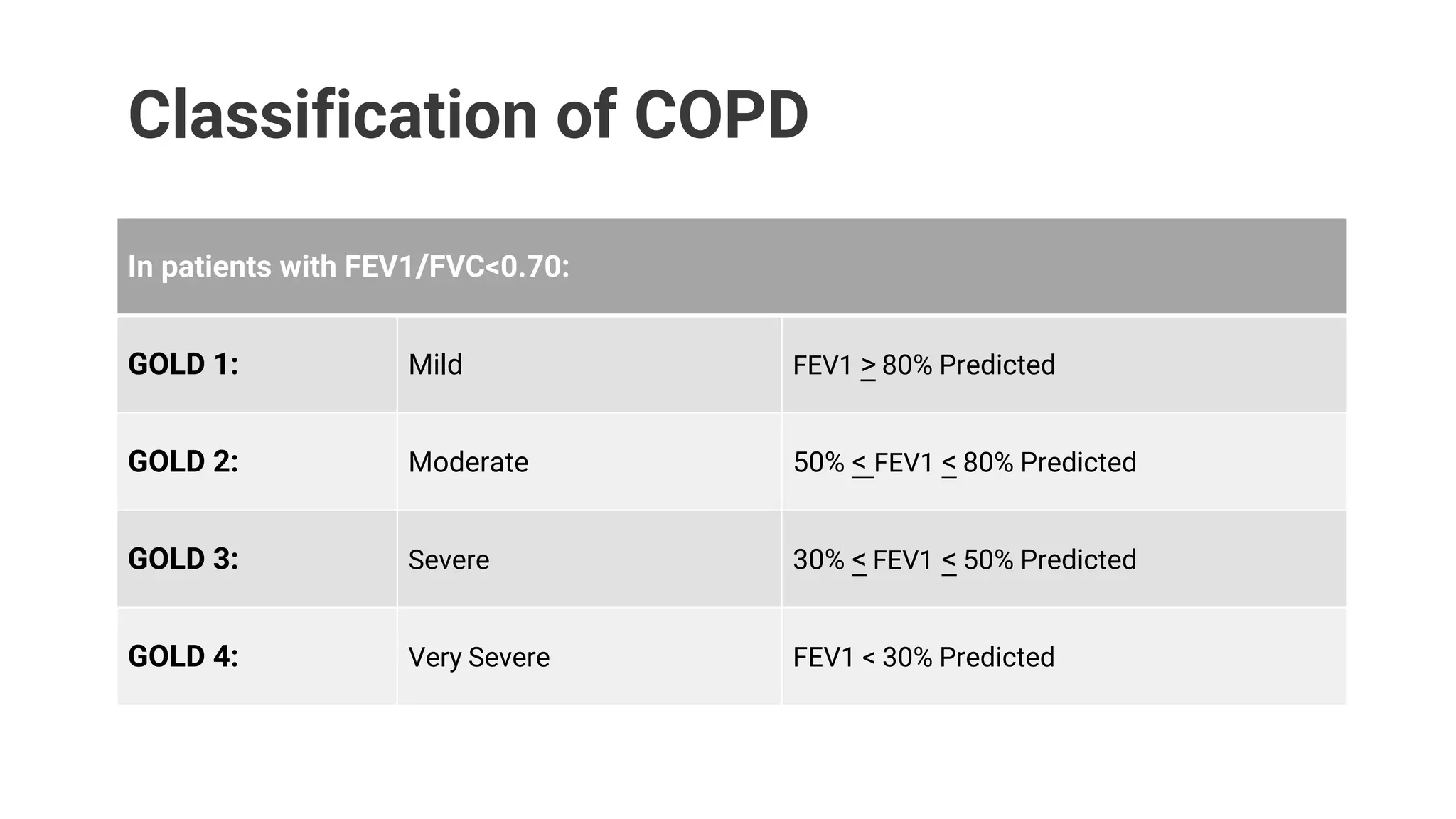
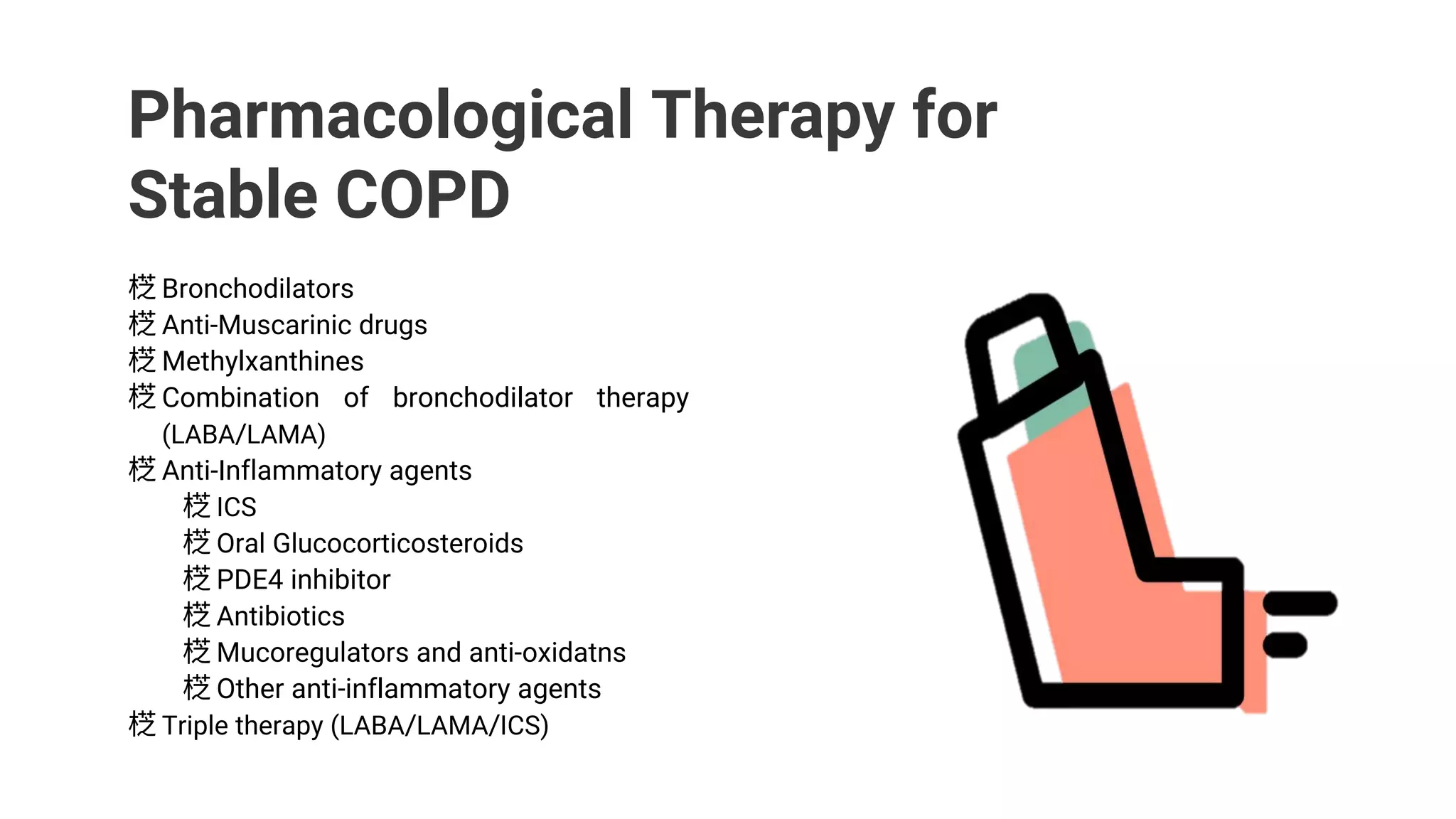
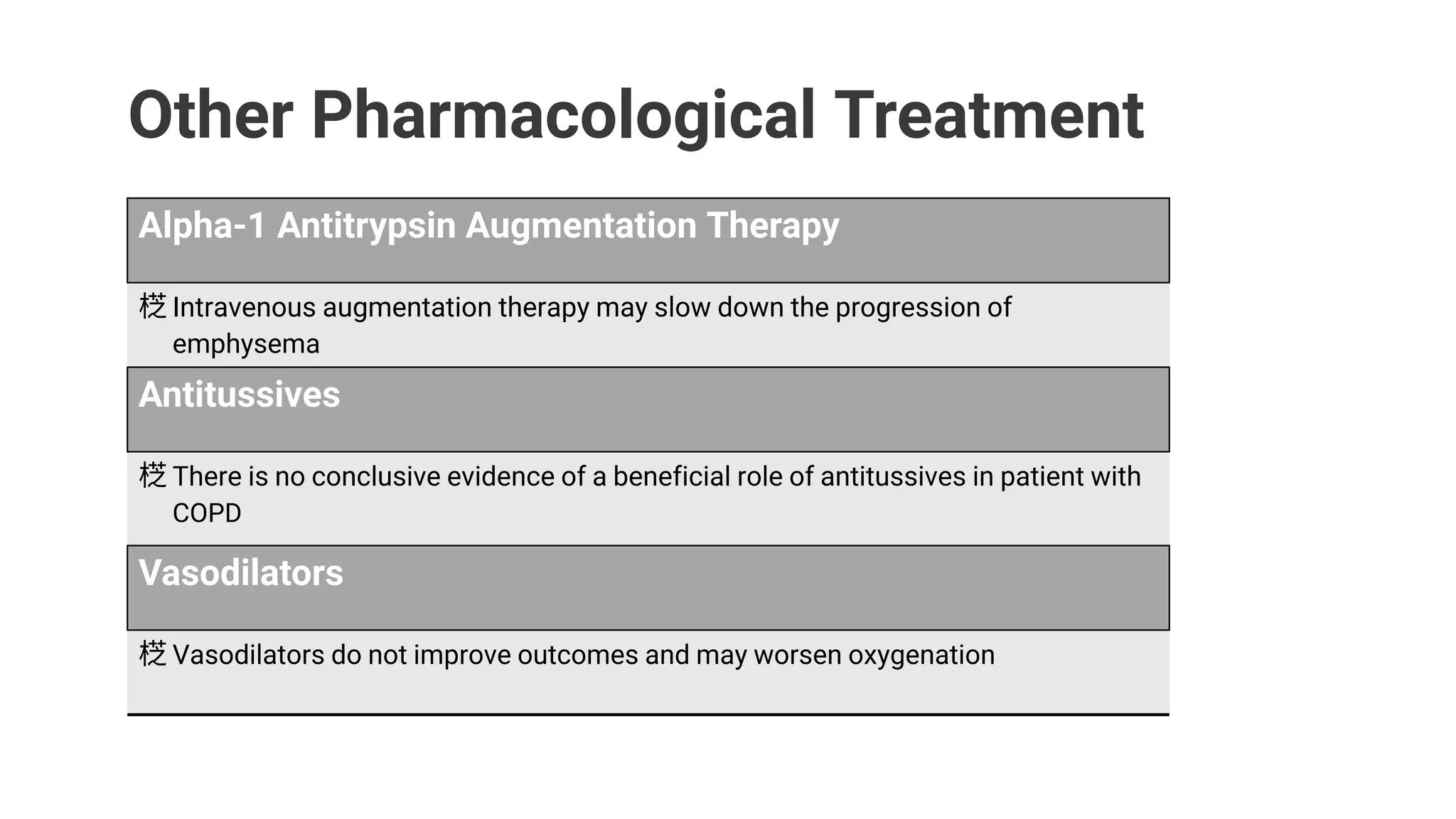
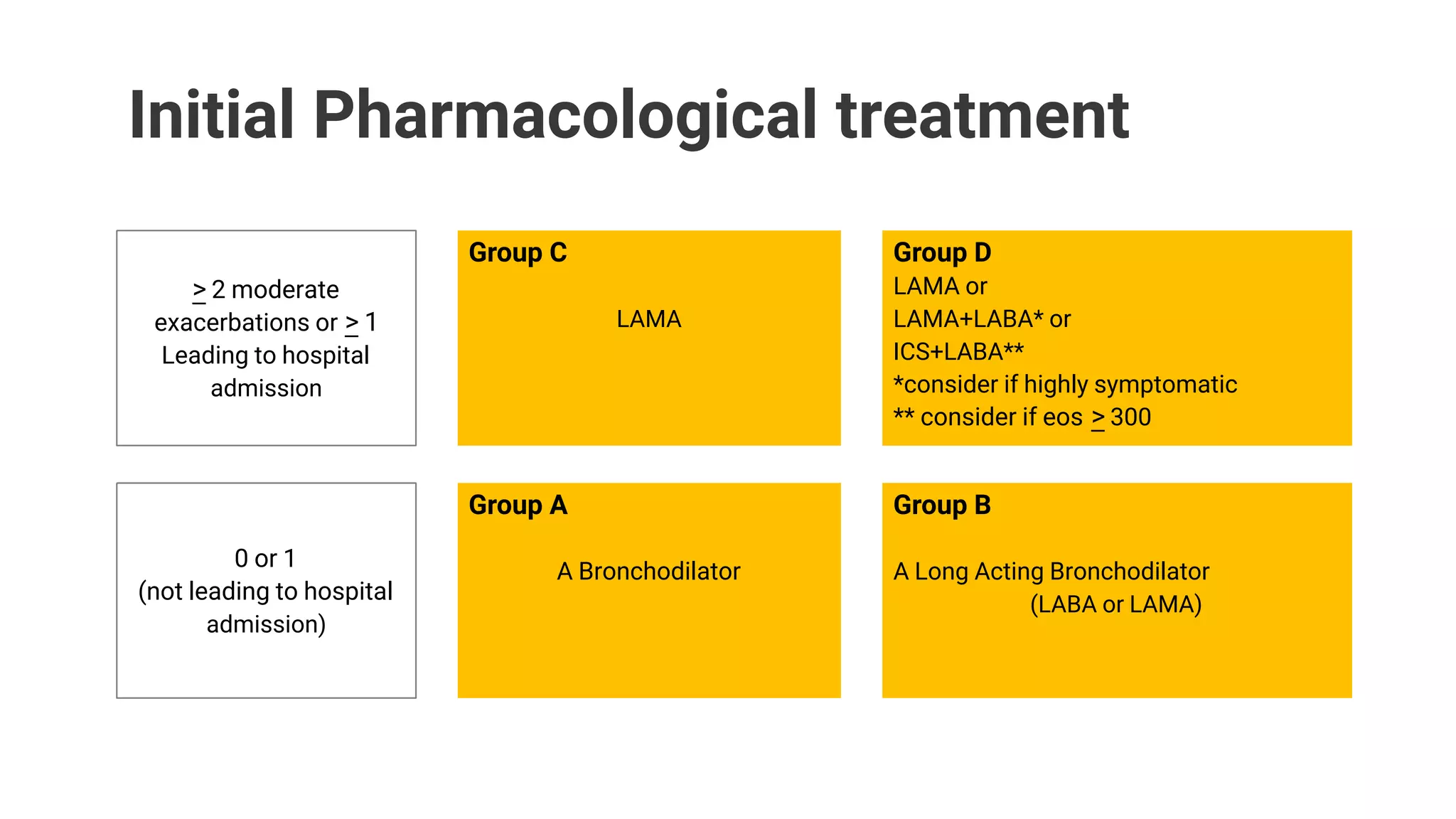
The document discusses COPD (chronic obstructive pulmonary disease), its causes, symptoms, differences from asthma, classifications, treatments, and management. It provides information from Dr. Mohammad Zannatul Rayhan on COPD, including that it is a lung disease caused by chronic interference with lung airflow and impairs breathing. The major cause of COPD is smoking. Treatments discussed include bronchodilators, anti-inflammatory drugs, oxygen therapy, pulmonary rehabilitation, and smoking cessation.