This document provides an overview of percutaneous coronary intervention (PCI) including:
- A brief history of PCI and the development of stents.
- Clinical factors that can influence PCI outcomes like diabetes, kidney disease, and ability to tolerate dual antiplatelet therapy.
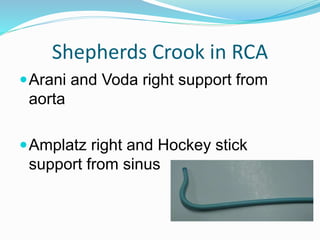
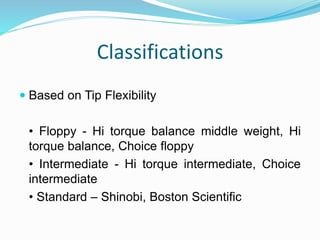
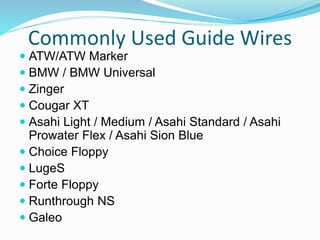
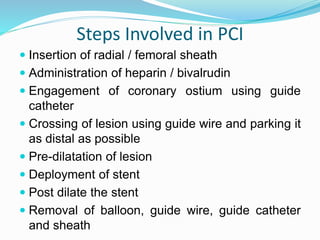
- Equipment used in PCI like guide catheters, guide wires, and balloon catheters.
- Medications given during and after PCI like aspirin, P2Y12 inhibitors, and GP IIb/IIIa inhibitors to prevent clotting and restenosis.
- Considerations for PCI in different clinical scenarios like UA/NSTEMI, STEMI, and adjunctive diagnostic devices that can