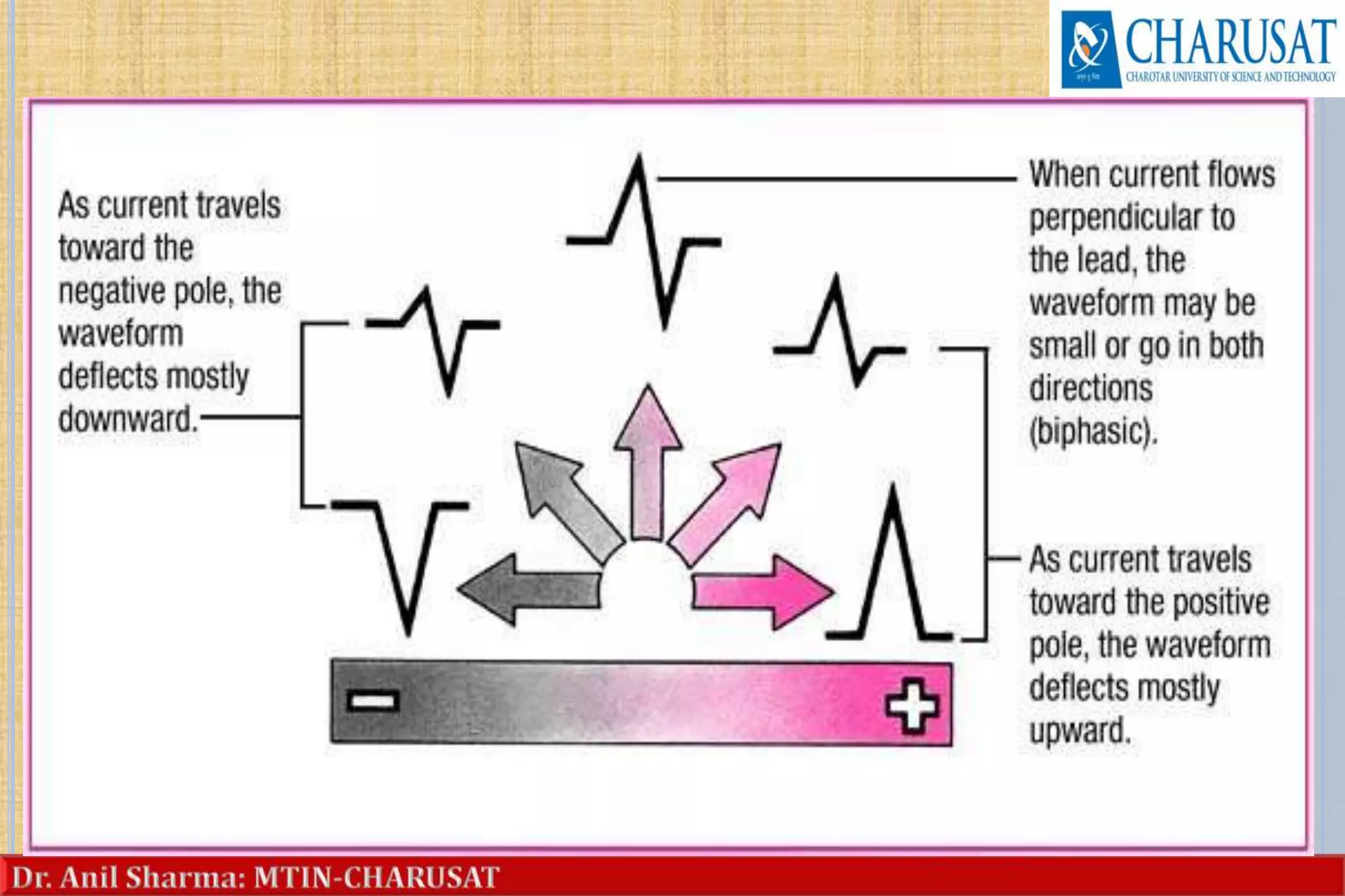
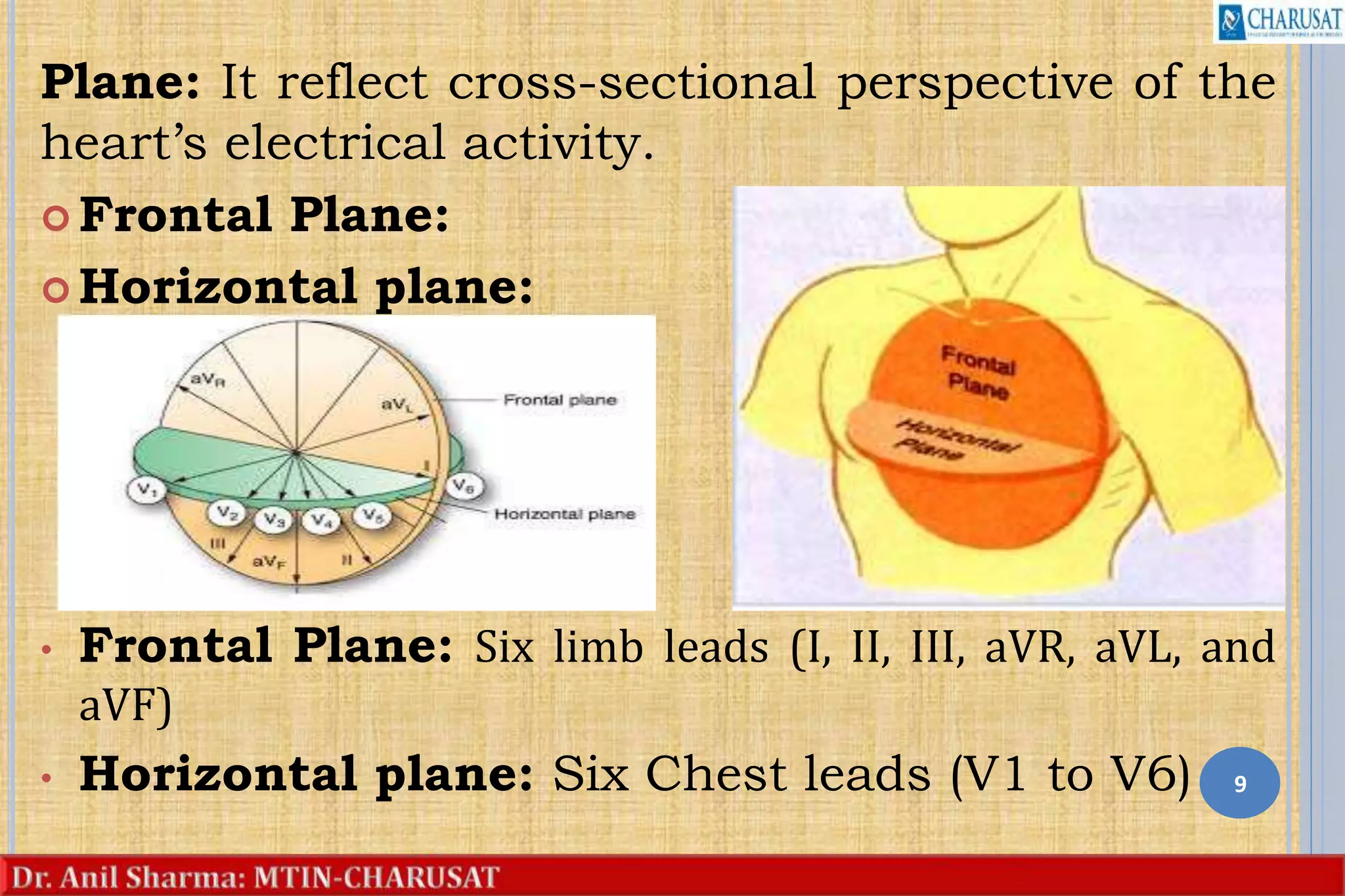
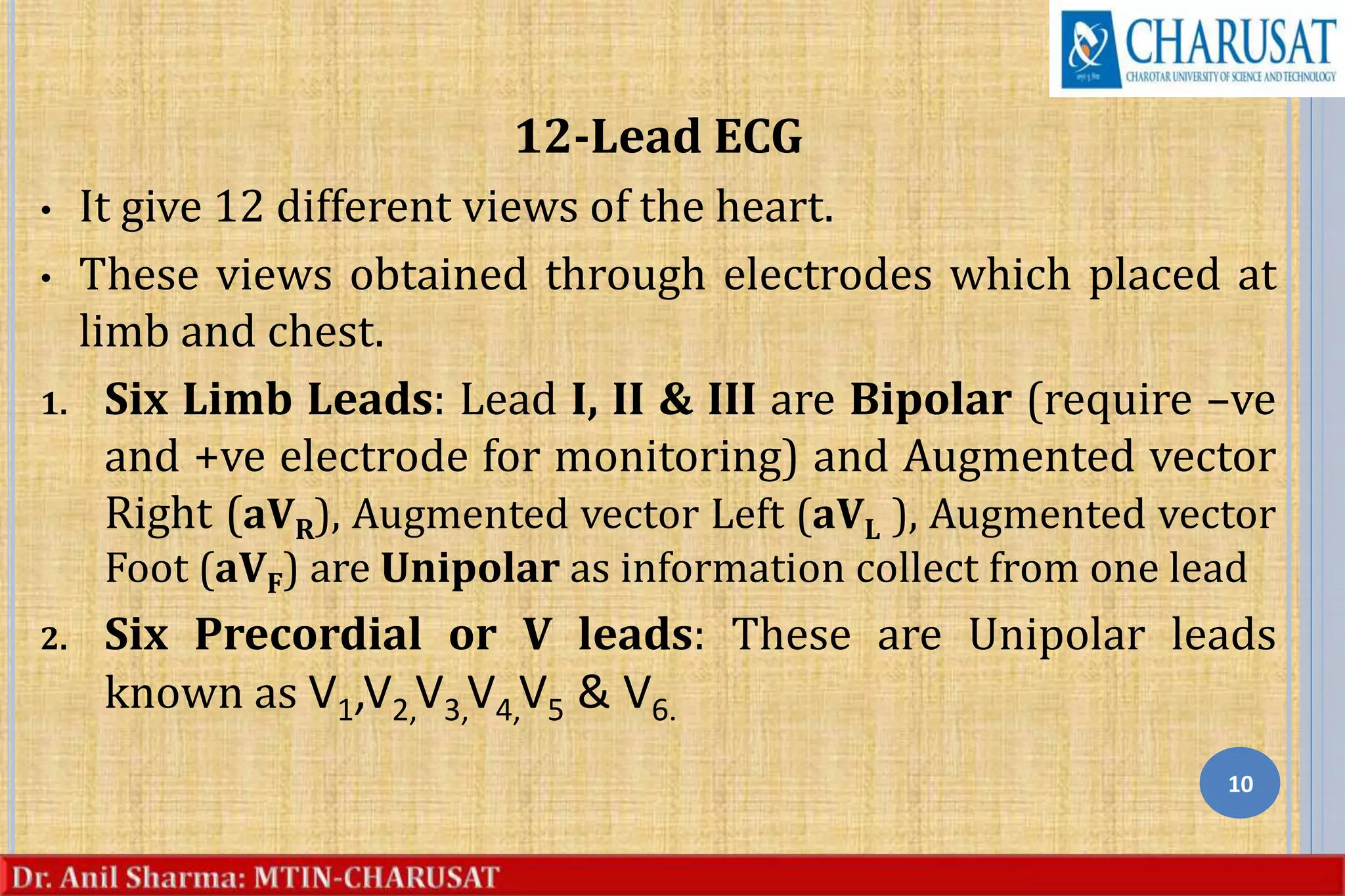
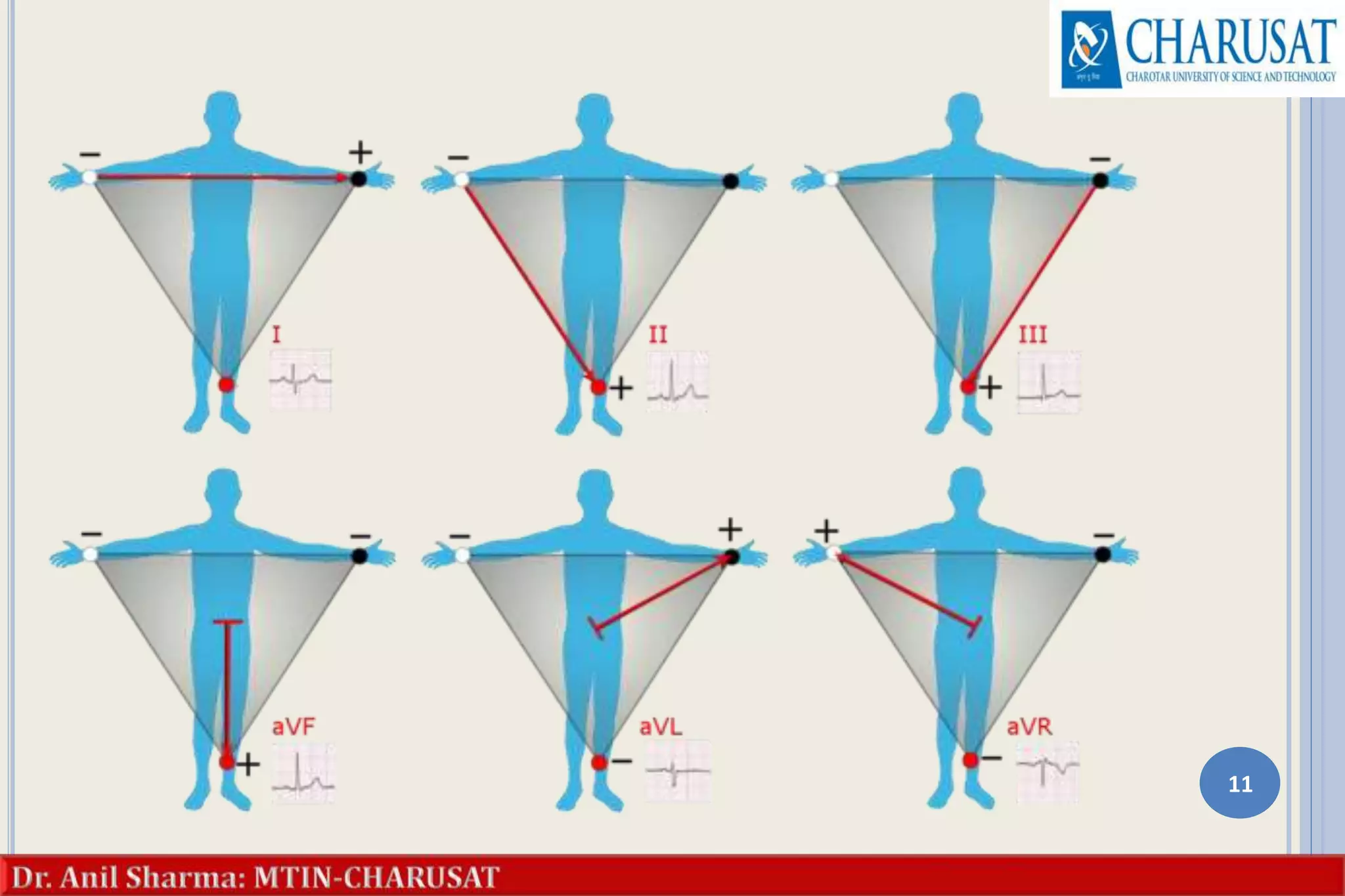
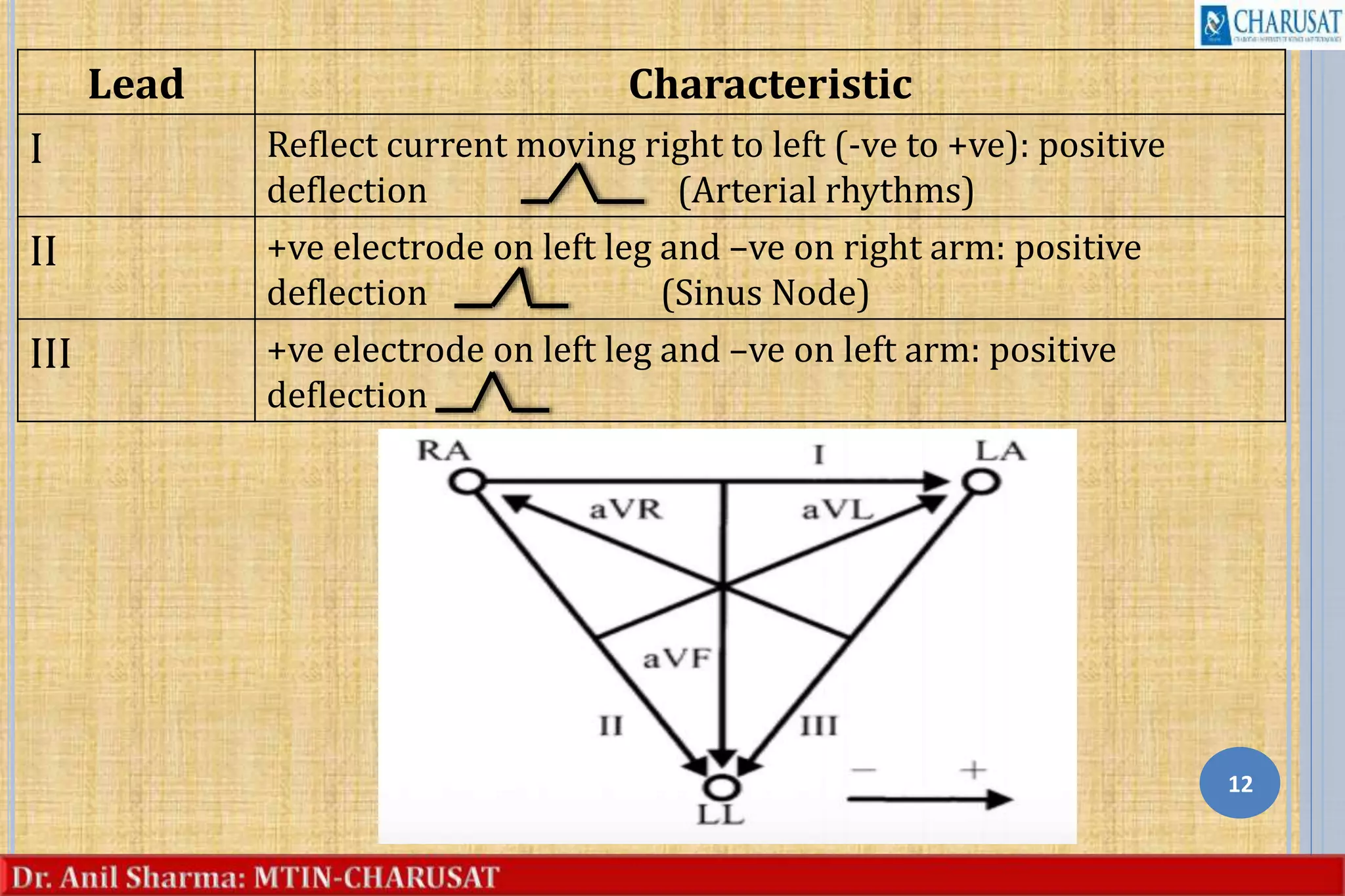
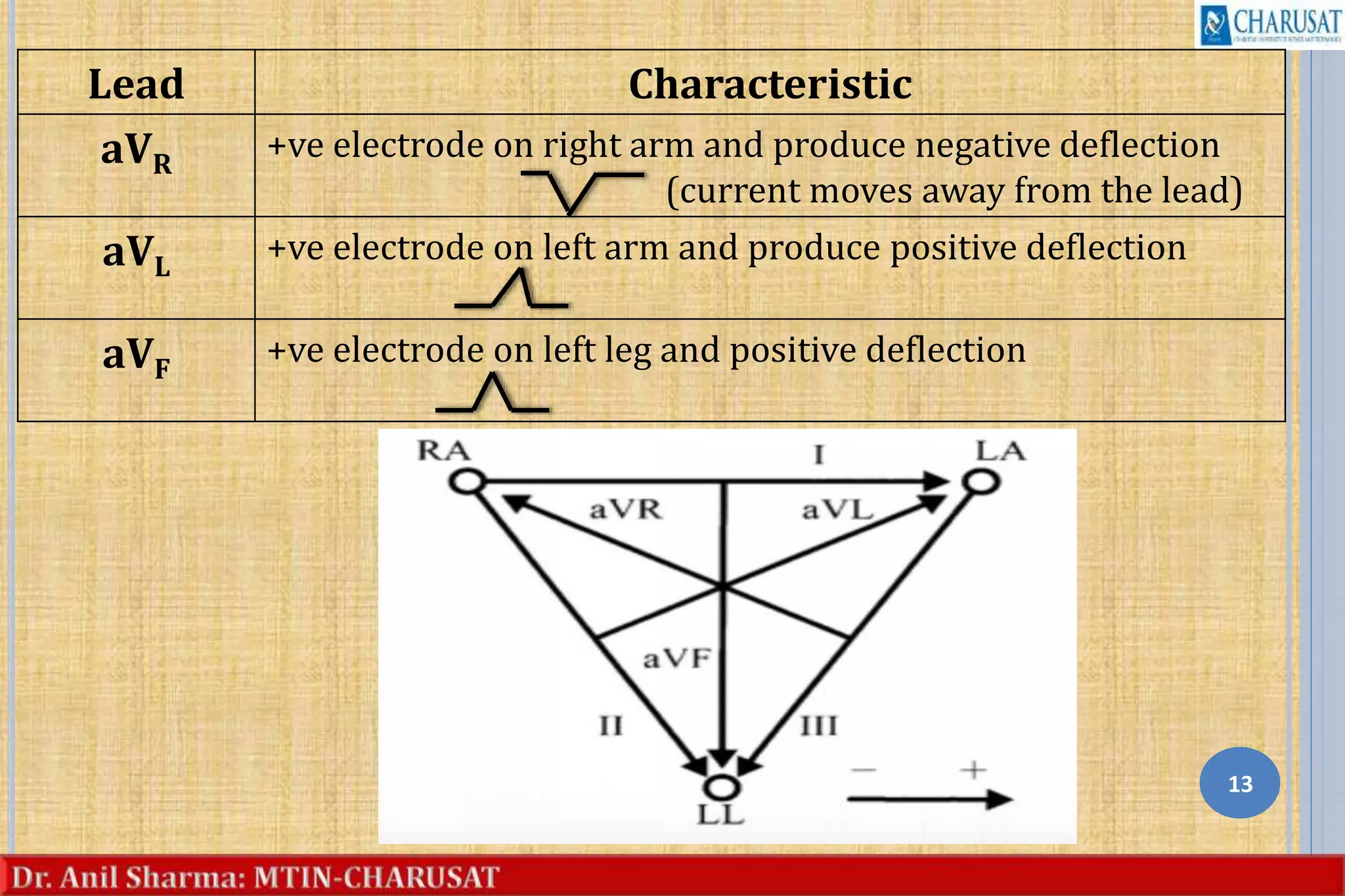
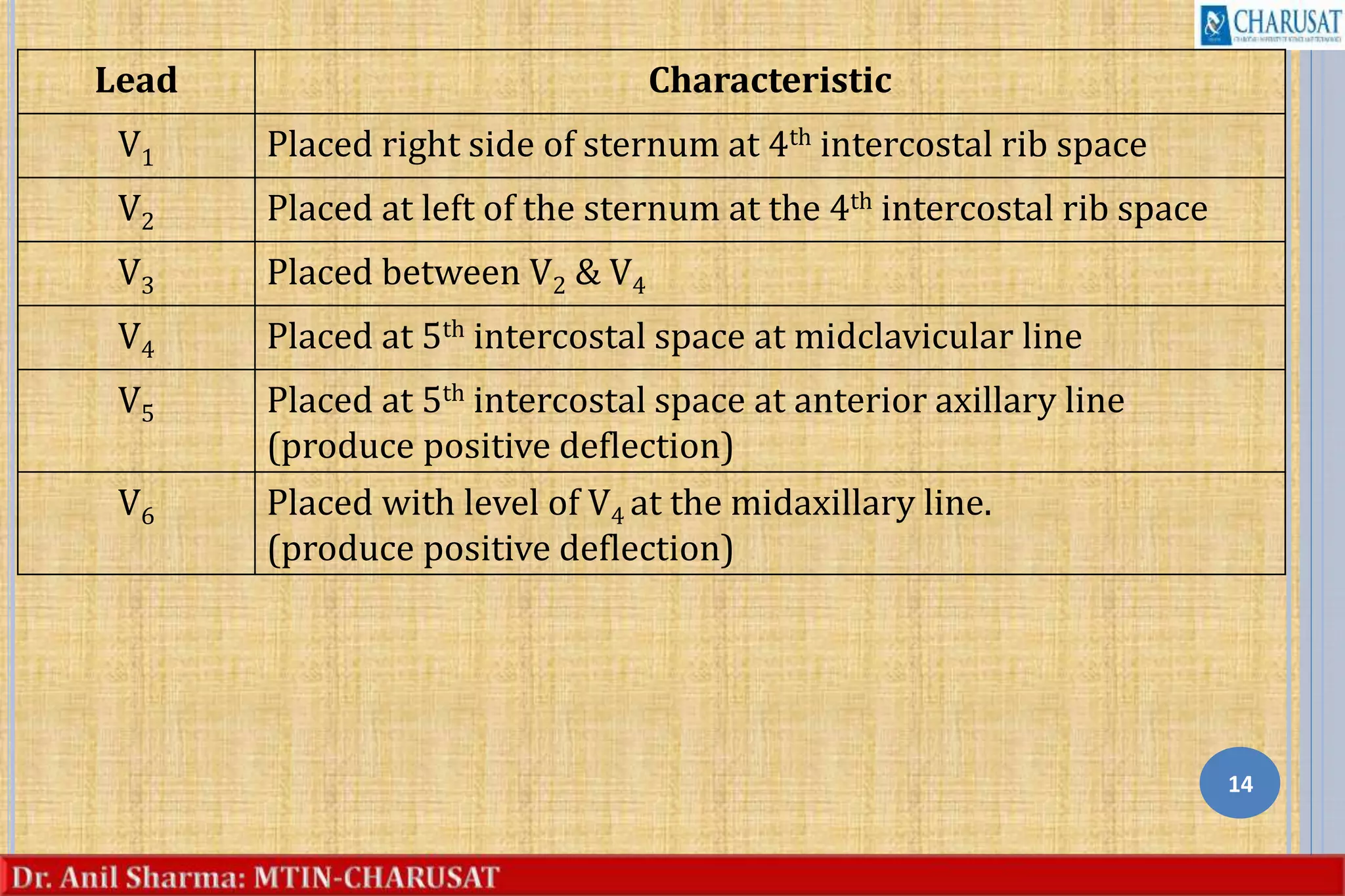
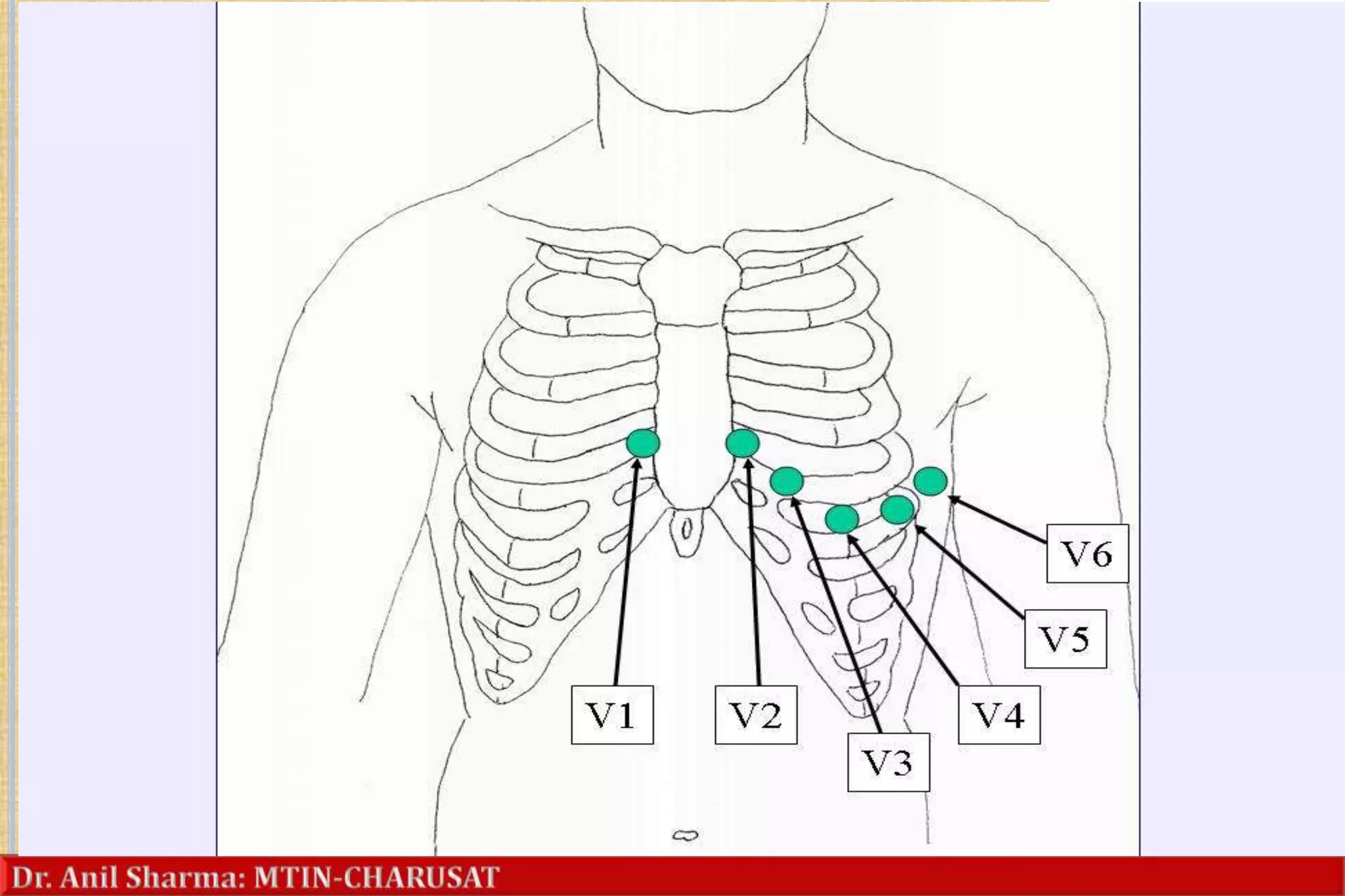
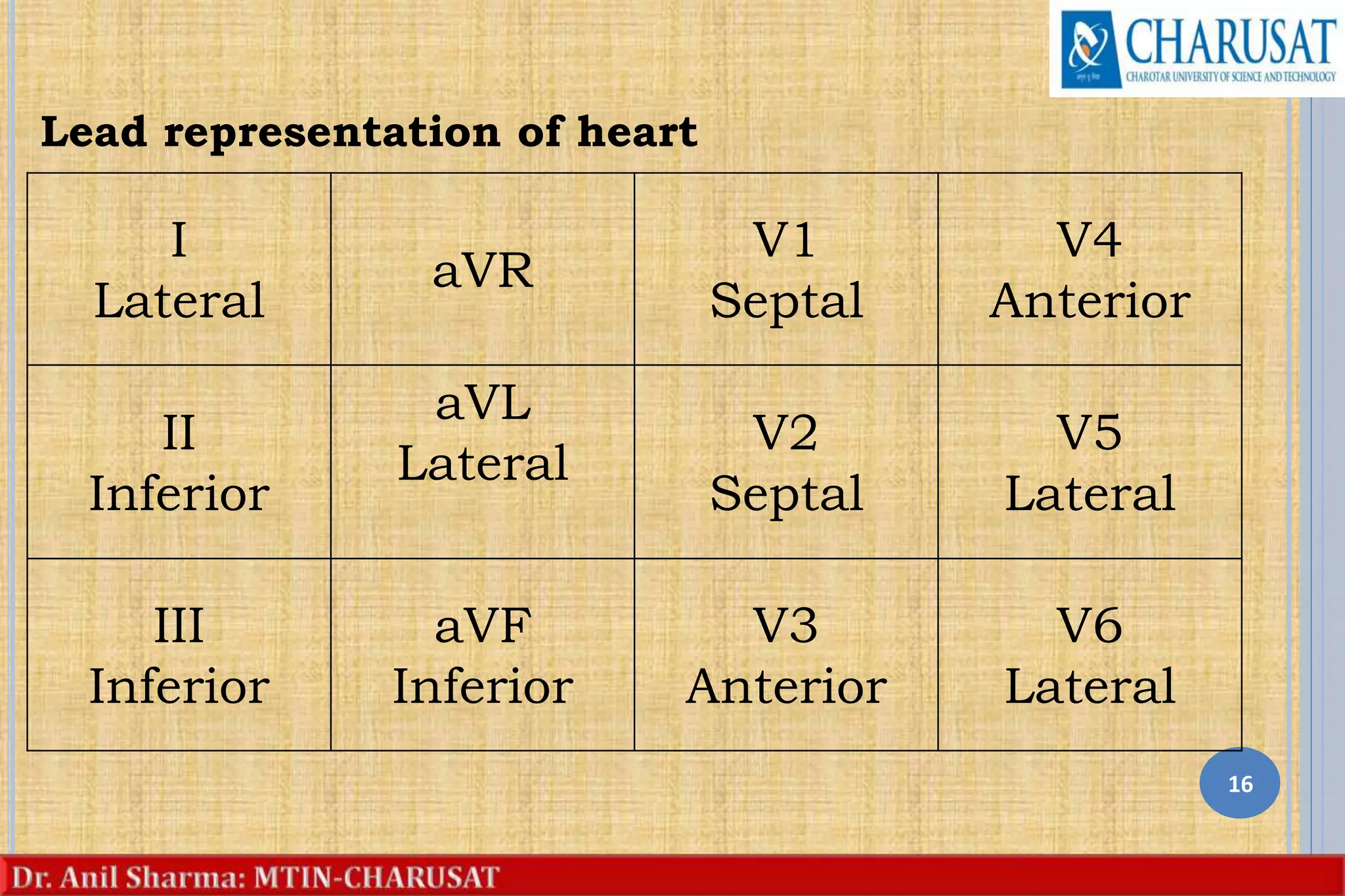
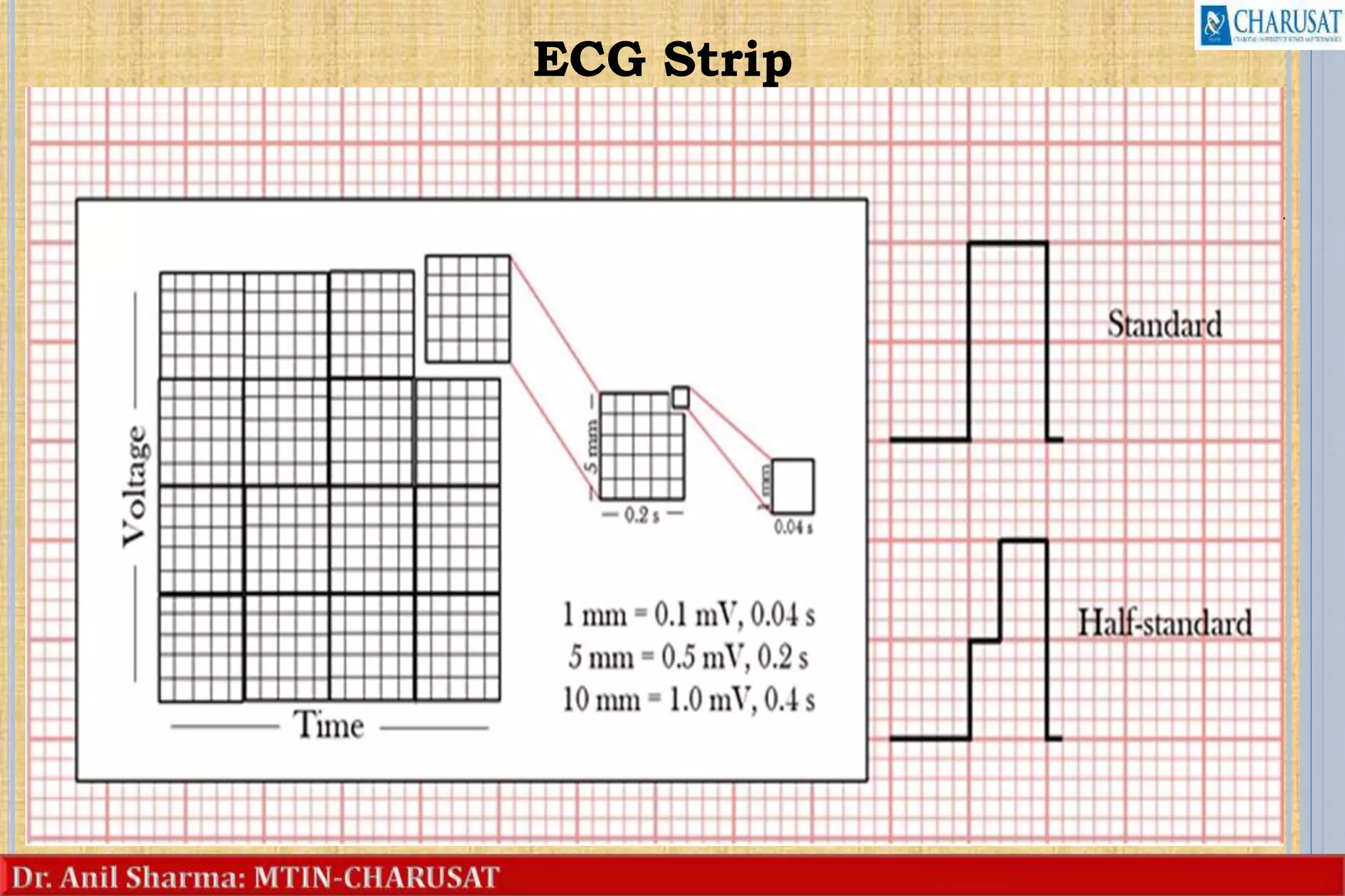
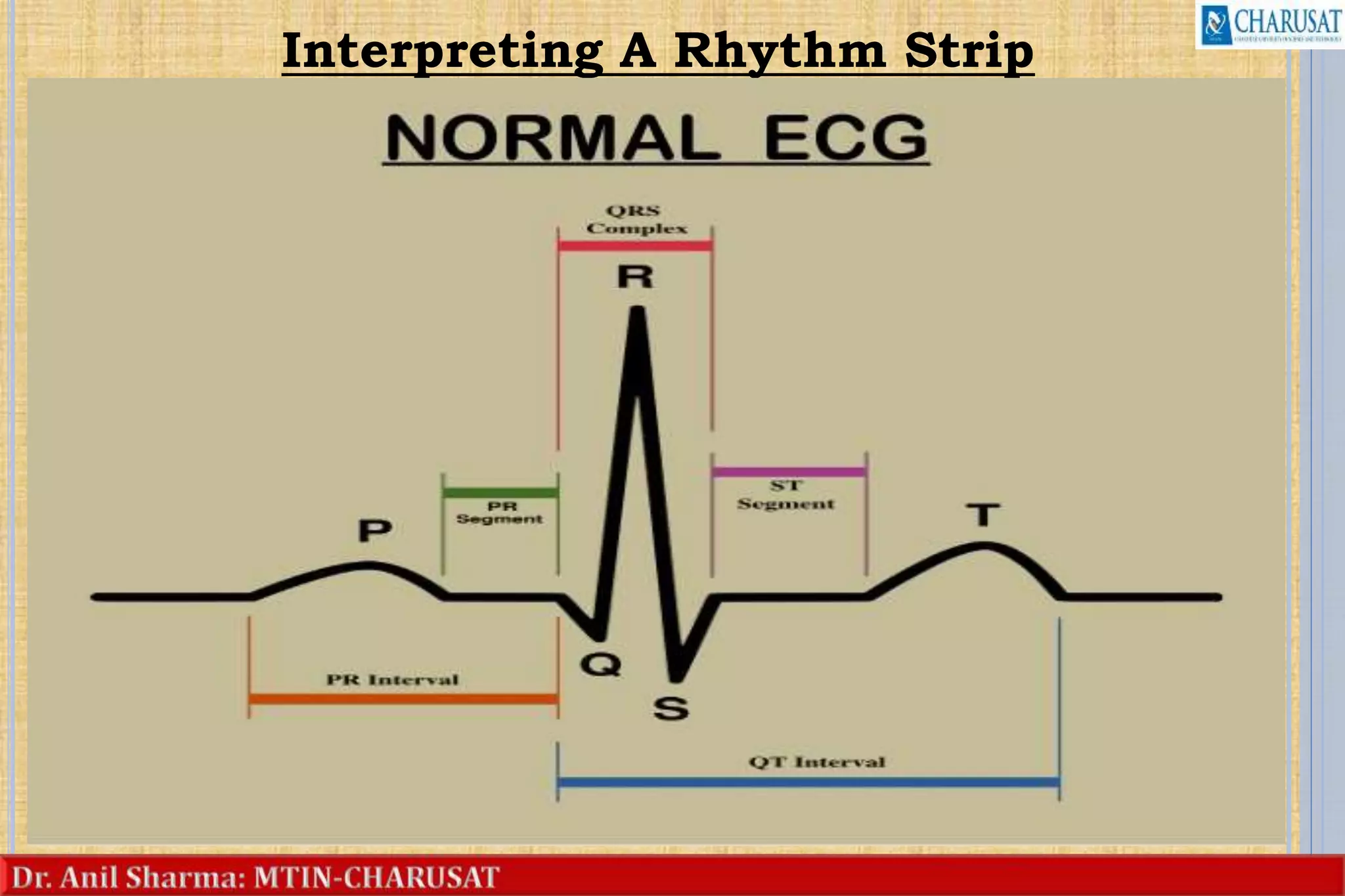
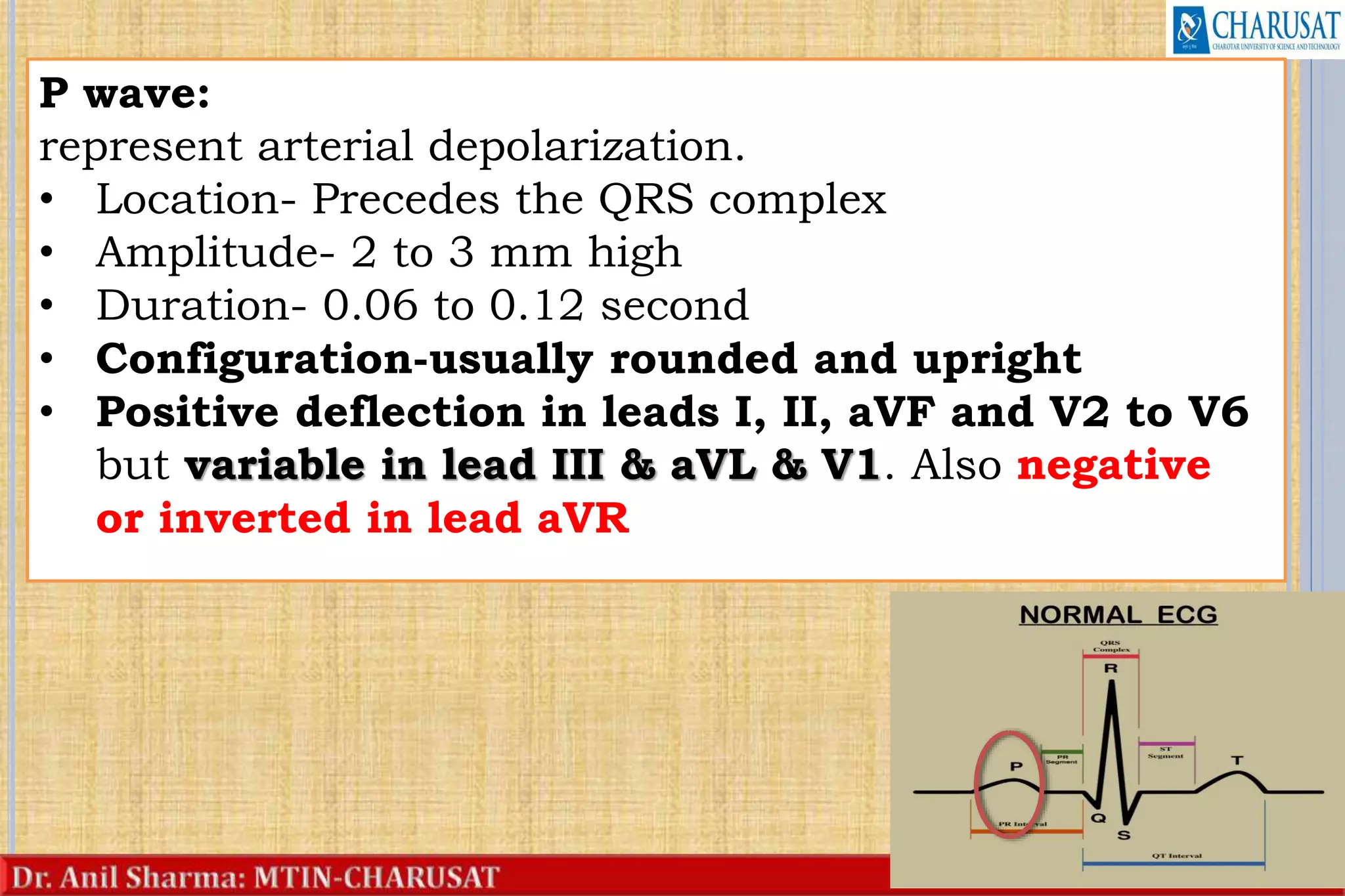
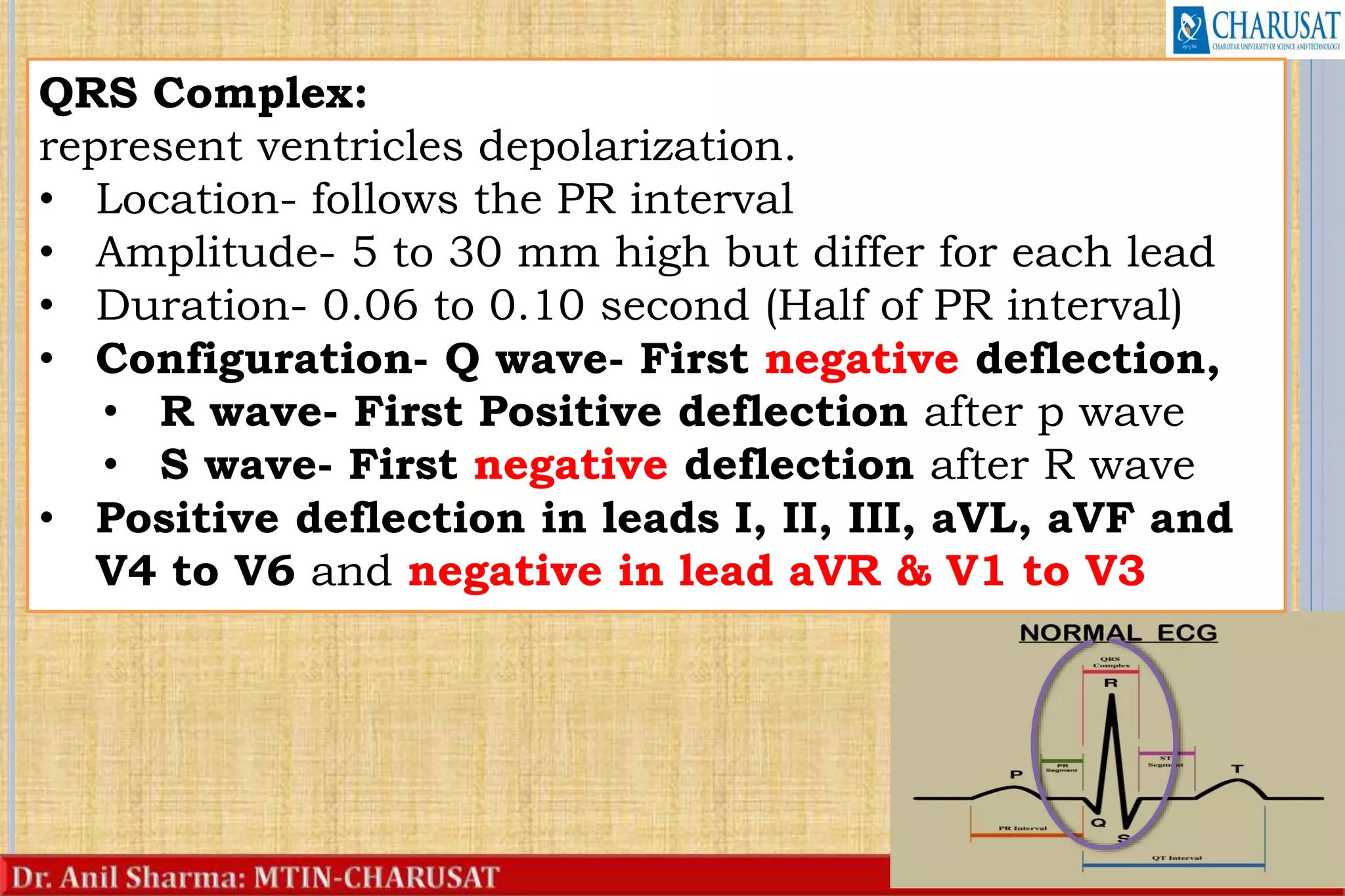
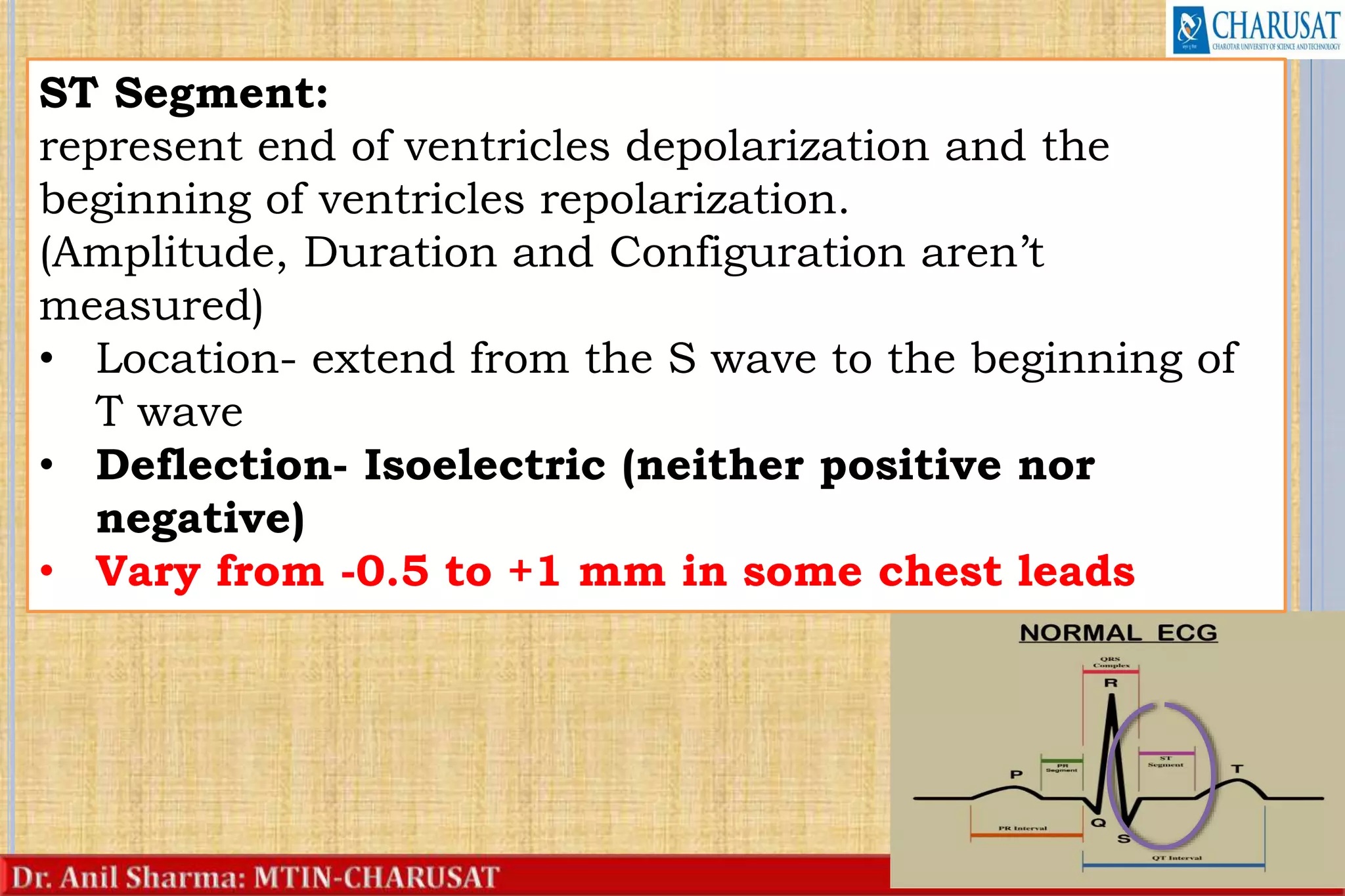
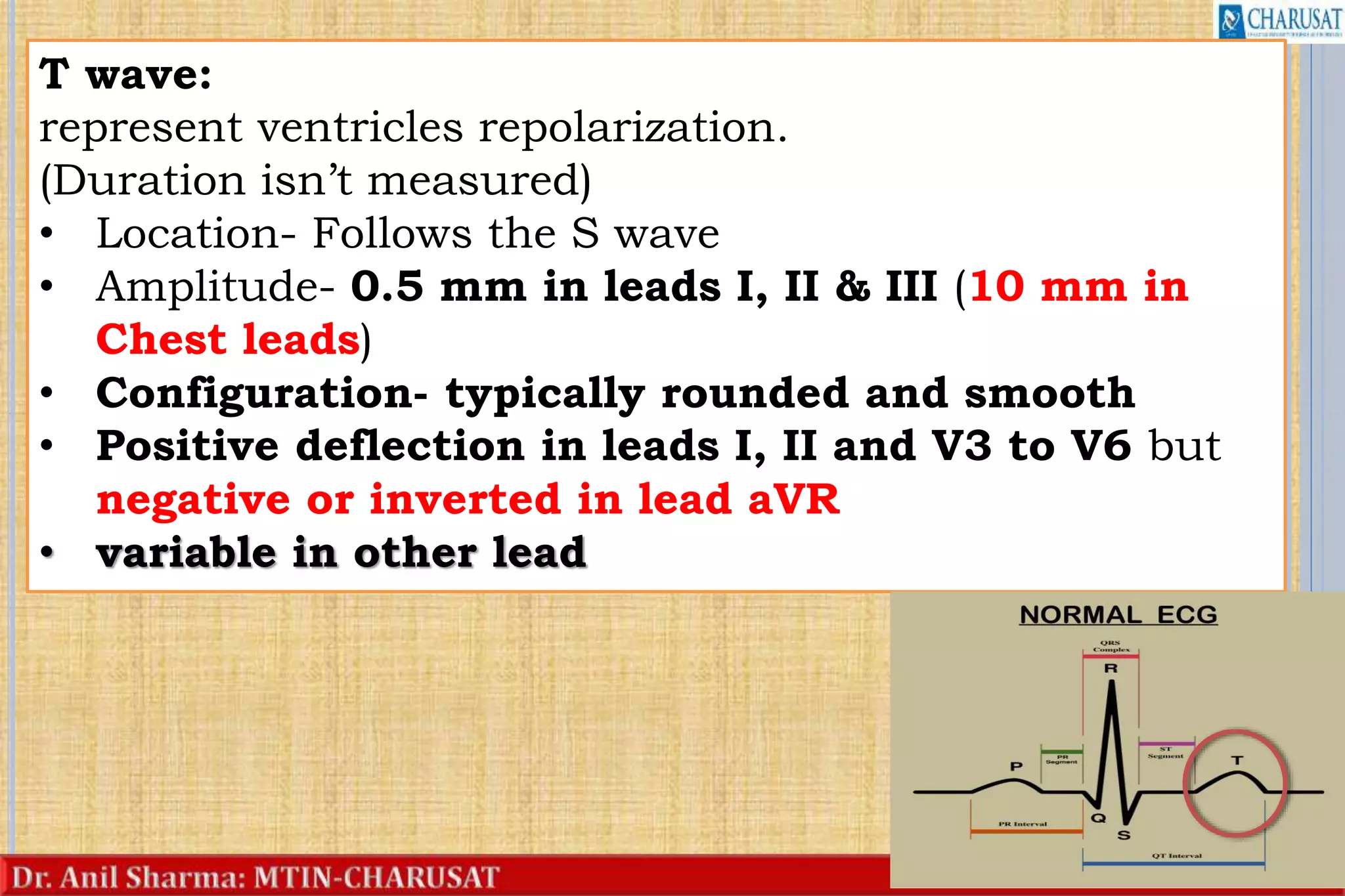
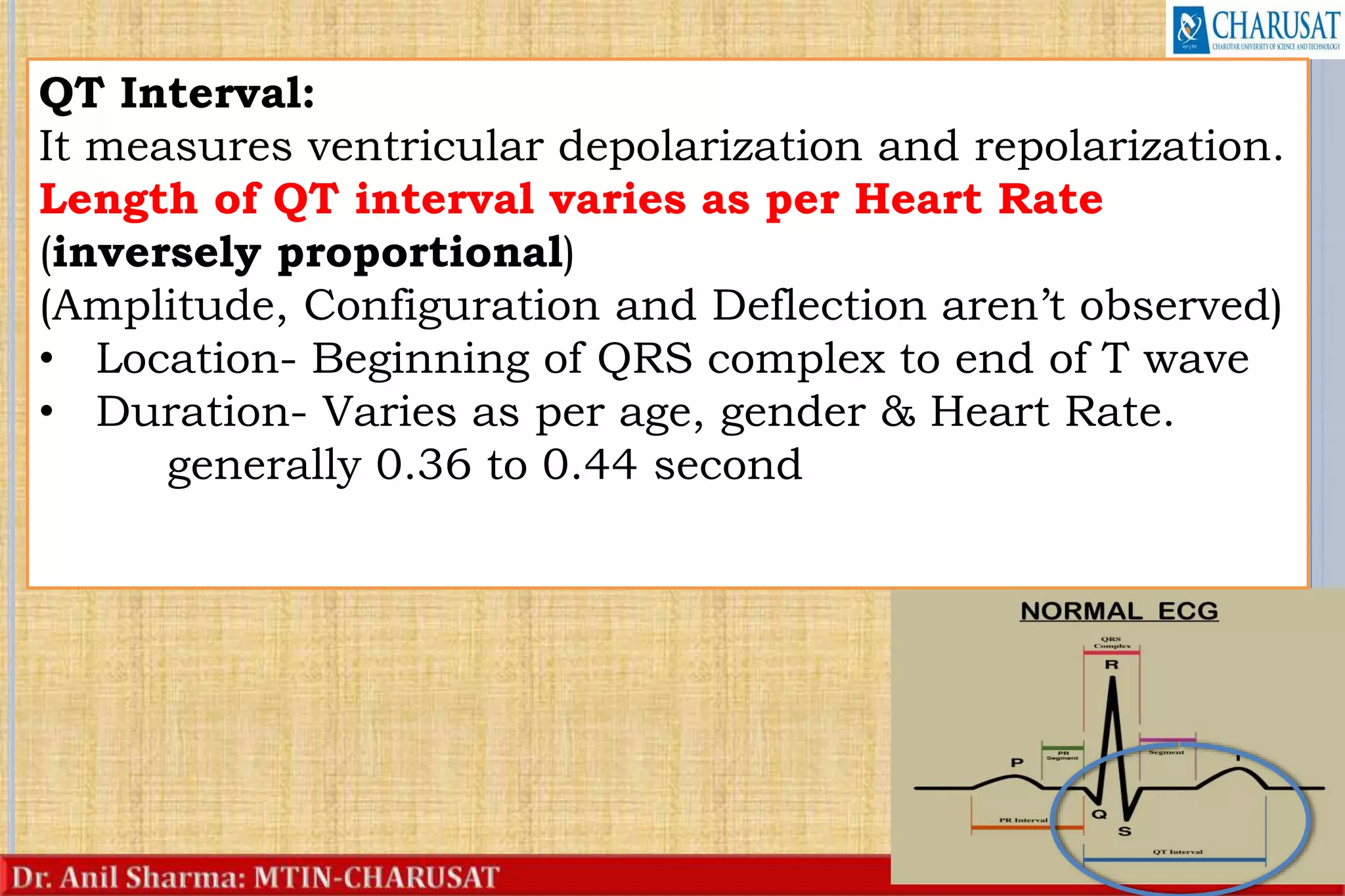
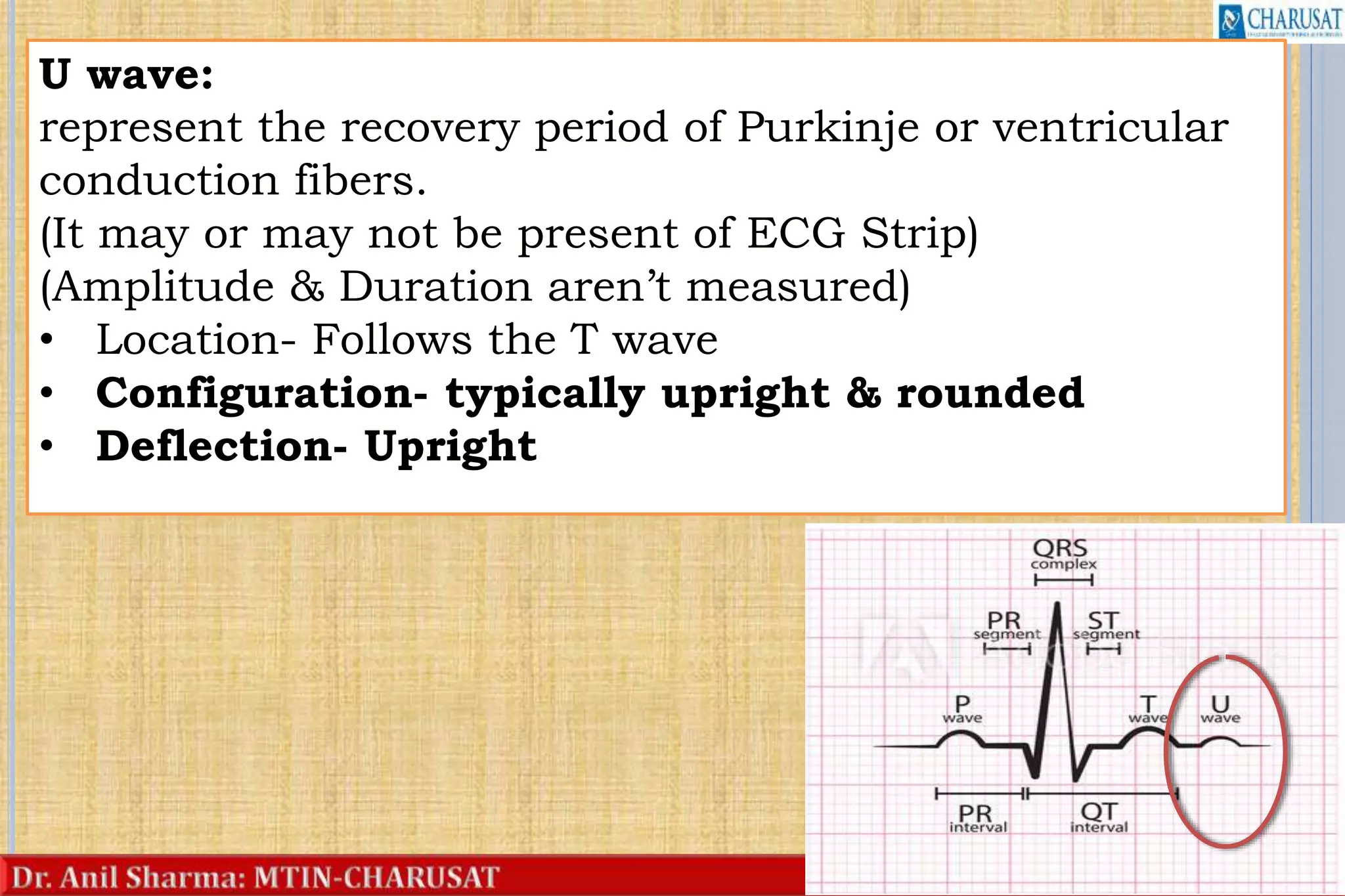
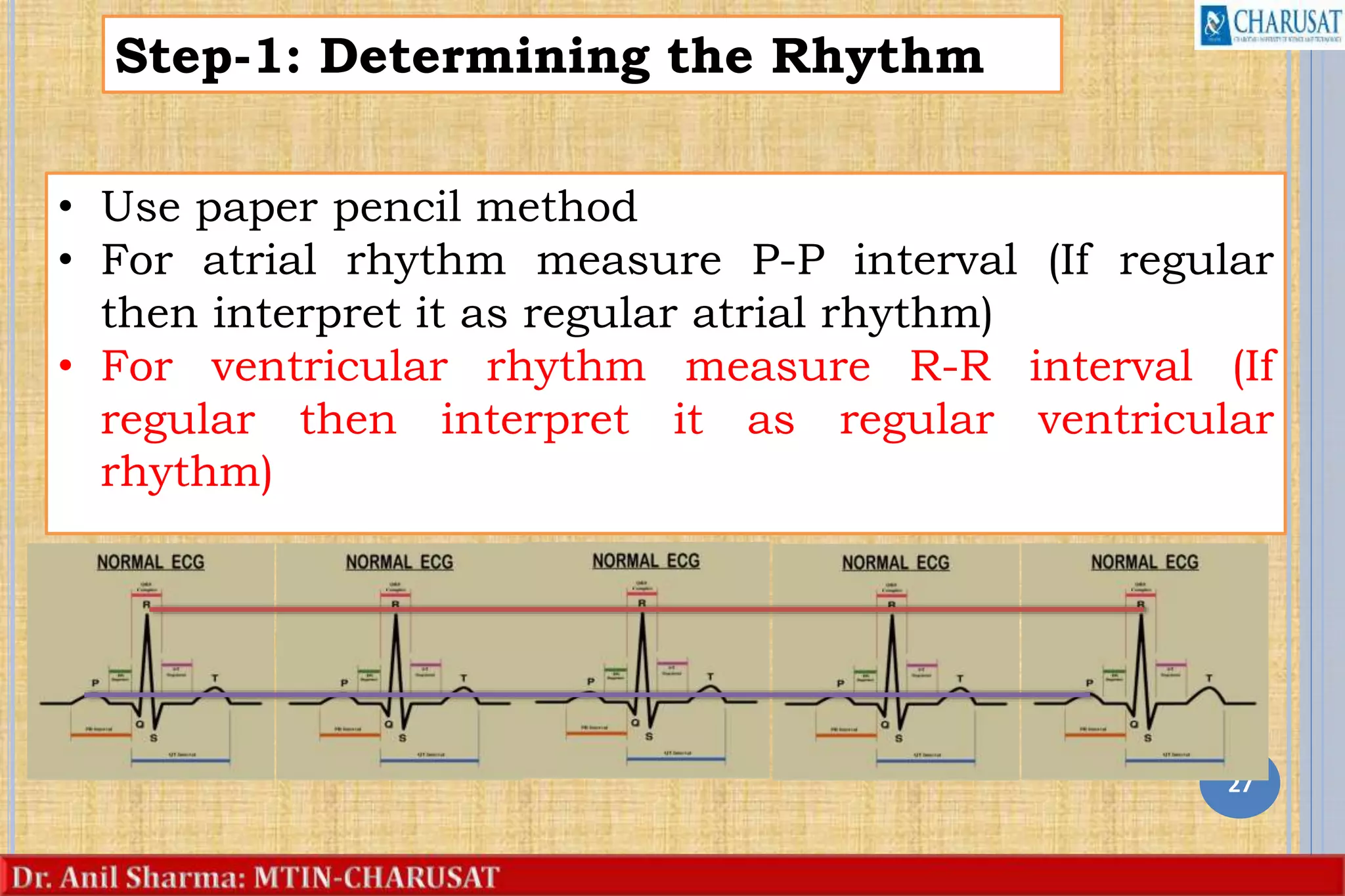
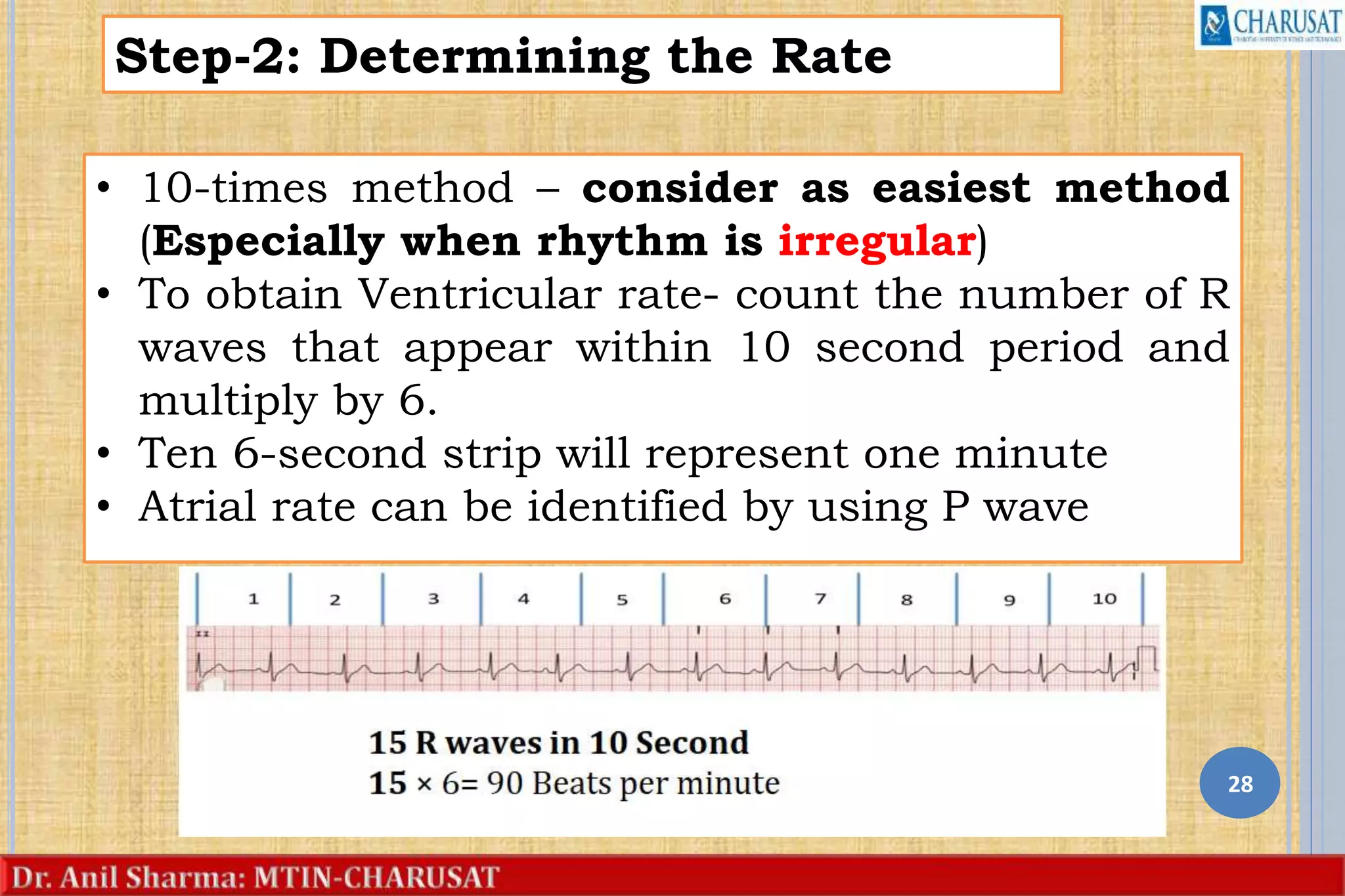
The document provides an overview of electrocardiogram (ECG or EKG) interpretation. It discusses cardiac anatomy and physiology relevant to understanding ECGs. The basics of the 12-lead ECG system are explained, including the six limb leads and six precordial leads. Components of the ECG waveform like the P, QRS, and T waves are defined. An 8-step method for ECG interpretation is outlined, beginning with analyzing the rhythm and rate, and then evaluating each waveform and interval. Key points include determining normal durations for the P wave, PR interval, QRS complex, QT interval, and identifying abnormalities. The summary restates normal findings for a sinus rhythm ECG.