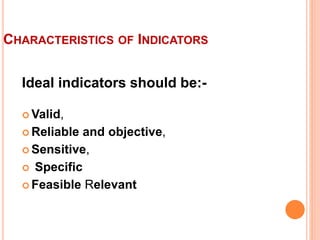
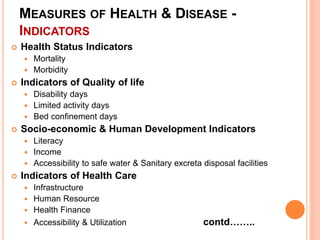
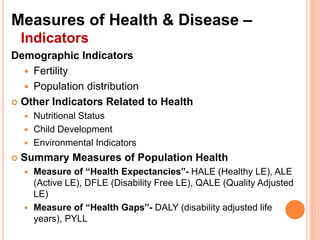
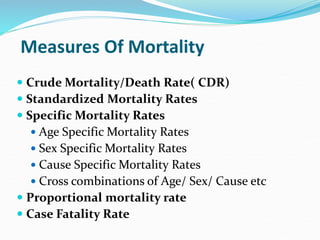
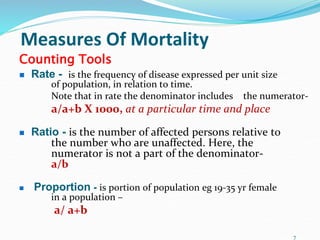
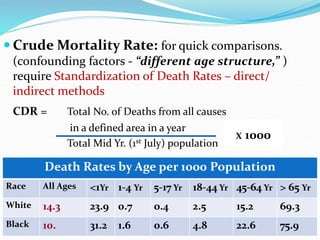
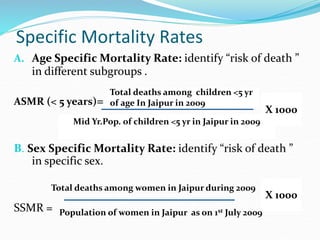
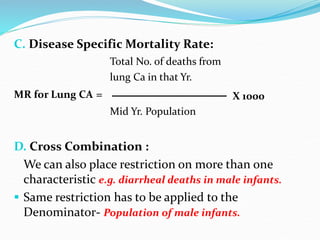
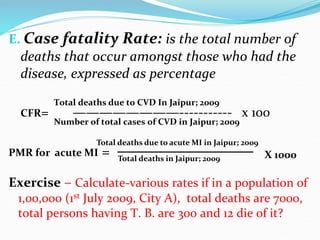
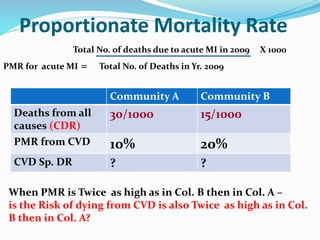
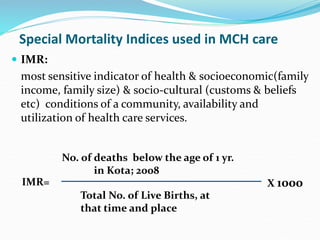
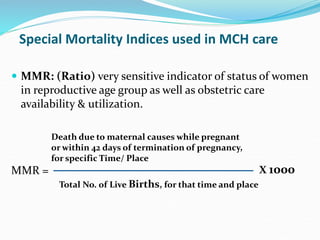
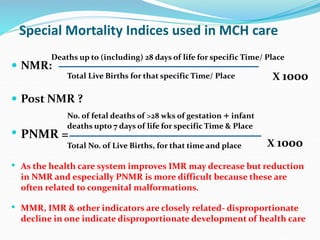
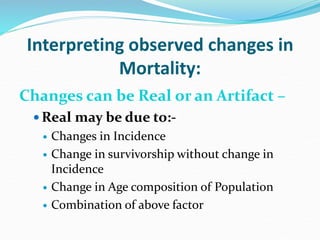
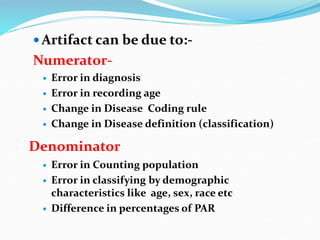
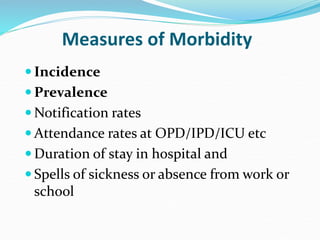
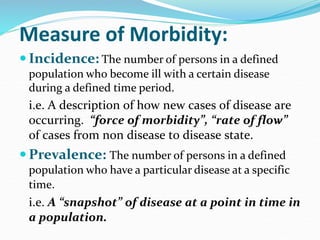
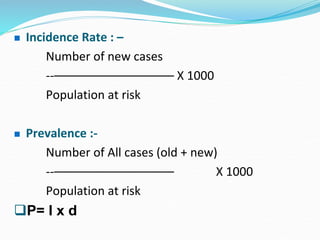
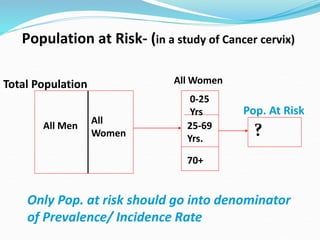
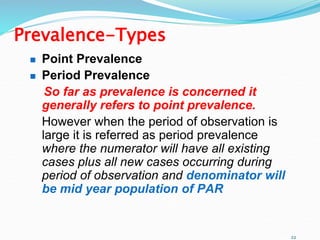
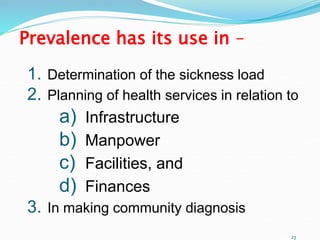
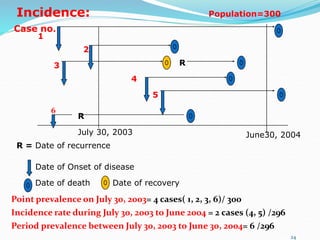
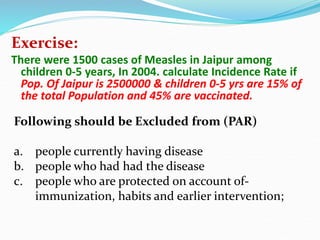
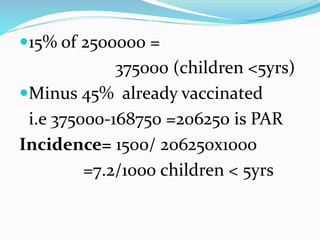
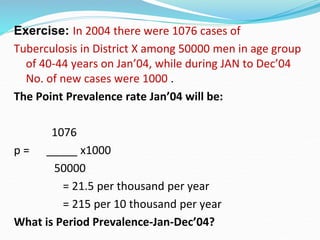
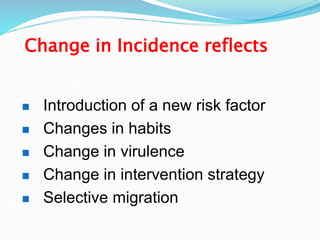
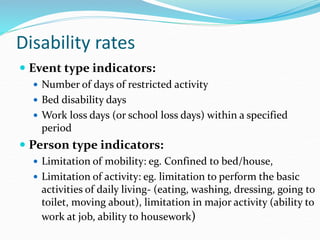
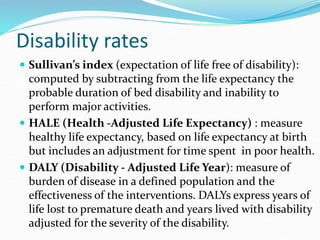
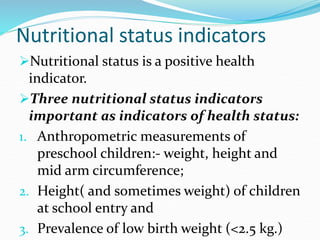
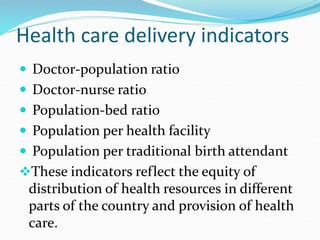
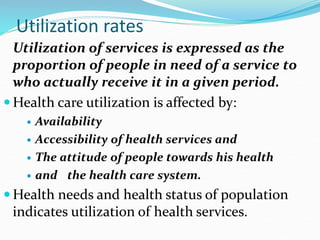
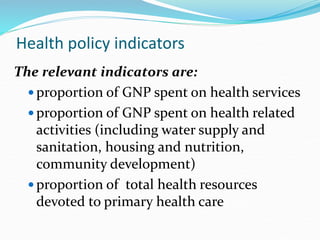
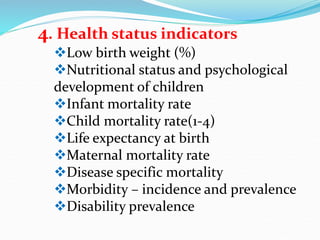
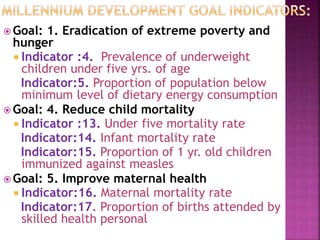
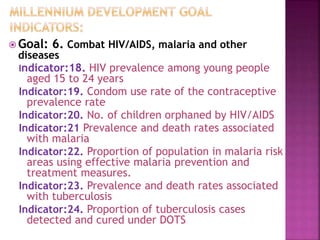
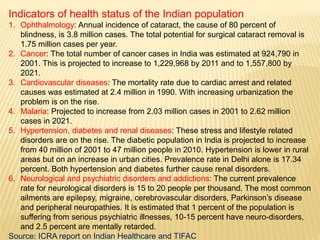
This document discusses various indicators that can be used to measure health and disease in a population. It outlines different types of indicators including health status indicators like mortality and morbidity, quality of life indicators, socioeconomic indicators, health care delivery indicators, and environmental indicators. Specific measures are provided for different types of indicators, such as crude mortality rate, standardized mortality rates, incidence rate, and prevalence. The indicators can help health administrators assess problems, design health plans, and evaluate schemes. Ideal indicators should be valid, reliable, sensitive, specific, and feasible.