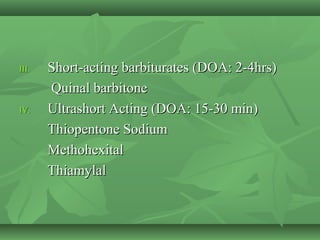
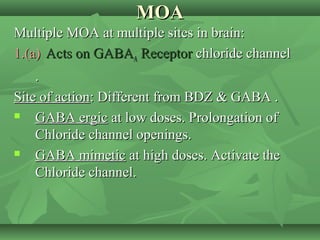
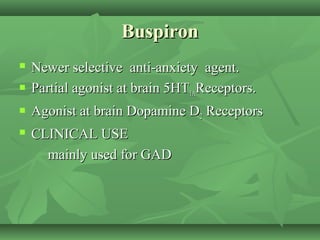
Barbiturates are derivatives of barbituric acid that act as central nervous system depressants. They have multiple mechanisms of action in the brain involving GABA receptors and ion channels. Barbiturates are classified based on their duration of action and include long, intermediate, short, and ultrashort-acting varieties. While once widely used as sedatives, hypnotics, and for anesthesia, barbiturates have significant disadvantages like low therapeutic index, drug interactions, abuse potential, and severe withdrawal syndrome. Newer agents like benzodiazepines, buspirone, zolpidem, and zaleplon have replaced barbiturates for most indications due to safer profiles